Gavi's impact
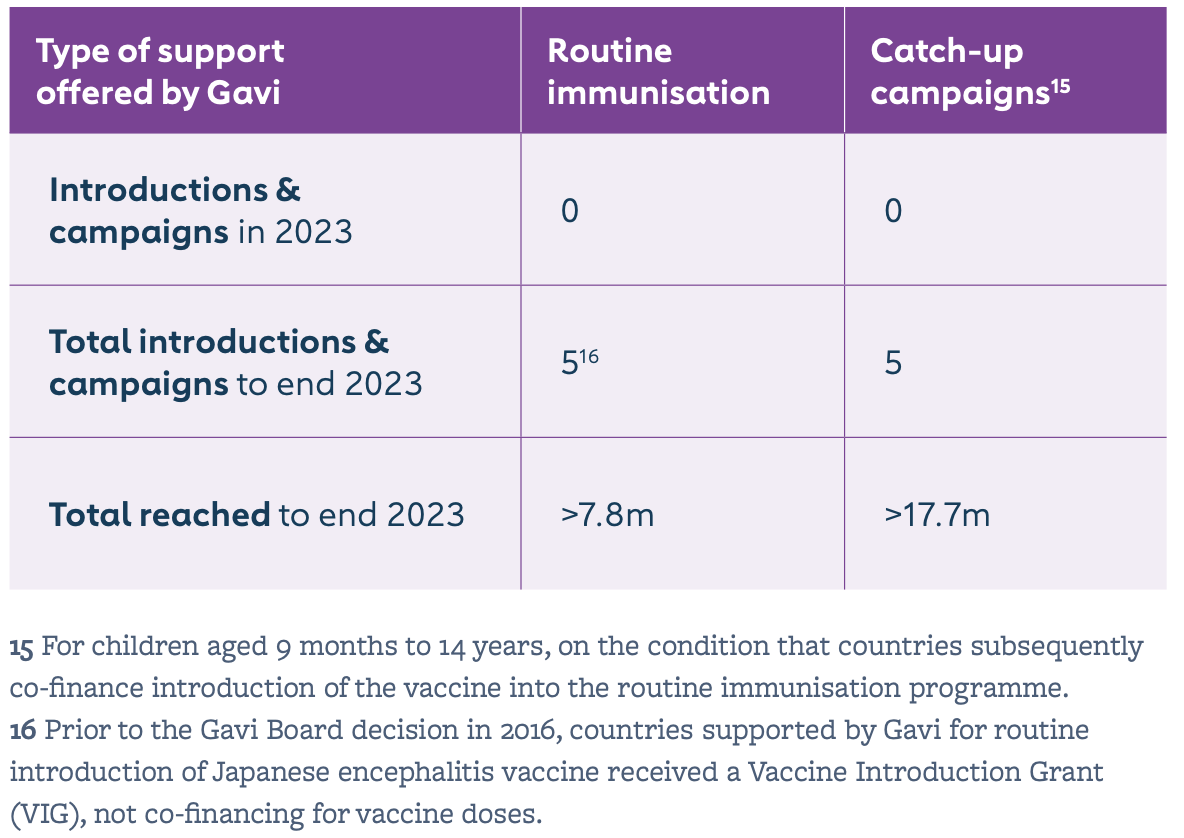
Since its Japanese encephalitis (JE) vaccine programme began in 2015, Gavi has supported five countries – Lao People’s Democratic Republic, Nepal, Myanmar, Cambodia and Indonesia – to conduct JE vaccination campaigns and to introduce the vaccine into the routine immunisation system. By end 2023, more than 7.8 million children had been immunised through Gavi-supported routine immunisation programmes; and more than 17.7 million children through catch-up campaigns. Bangladesh will be the next Gavi-supported country to introduce, with a sub-national campaign approved and planned for 2026.
Partnership engagement is crucial to support countries not only to develop a sound application, but also to plan and implement immunisation activities, as well as to detect and respond to JE cases. It is important to consider other immunisation activities in the country (e.g. typhoid conjugate vaccine campaigns) to apply lessons learned and integrate when possible.
The issue
JE is a flavivirus, transmitted to humans by the bite of Culex mosquitoes that have contracted it from infected pigs or wading birds such as herons and egrets. It cannot, however, be transmitted from one person to another.
JE is the main cause of viral encephalitis in many countries of Asia, with an estimated 100,000 clinical cases every year – the majority of whom are children aged under 15 years. Although symptomatic JE is rare, the case-fatality rate among those with encephalitis can be as high as 30%. Permanent neurologic, cognitive and behavioural sequelae occur in 30–50% of those with encephalitis. Often called “brain fever”, it begins with flu-like symptoms before progressing to brain infection.
Over 3 billion people live in at-risk areas, particularly in low-income rural communities across eight Gavi-supported countries in South-East Asia and the Western Pacific. WHO estimates that JE causes approximately 25,000 deaths each year. WHO recommends that JE vaccination be integrated into national immunisation schedules in all areas where JE disease is recognised as a public health issue. Gavi provides details on quantifying JE burden to support routine introduction and campaigns in its Vaccine Funding Guidelines, based on technical partner recommendations, to support countries looking to apply.
Gavi’s response
In 2014, Gavi first invited countries to apply for support to introduce the JE vaccine. The first Gavi-funded JE vaccination campaign started in the Lao People’s Democratic Republic in 2015, with Nepal and Cambodia following suit in 2016. Myanmar conducted a nationwide campaign in 2017 targeting children aged from 9 months to under 15 years, with introduction into routine nationwide in 2018; and Bali in Indonesia conducted an island-wide campaign in 2018 with introduction into routine the same year.
Gavi provides support for JE vaccine catch-up campaigns (vaccine procurement and operational costs); and, for applications received since 2016, Gavi co-finances the vaccine for use in routine immunisation programmes. Campaigns target children aged from 9 months to under 15 years and ensure sustainability by embedding JE vaccine into national immunisation programmes. Where the vaccine is introduced into the routine system, children are vaccinated at 12 months.
From other sites