Gavi’s impact
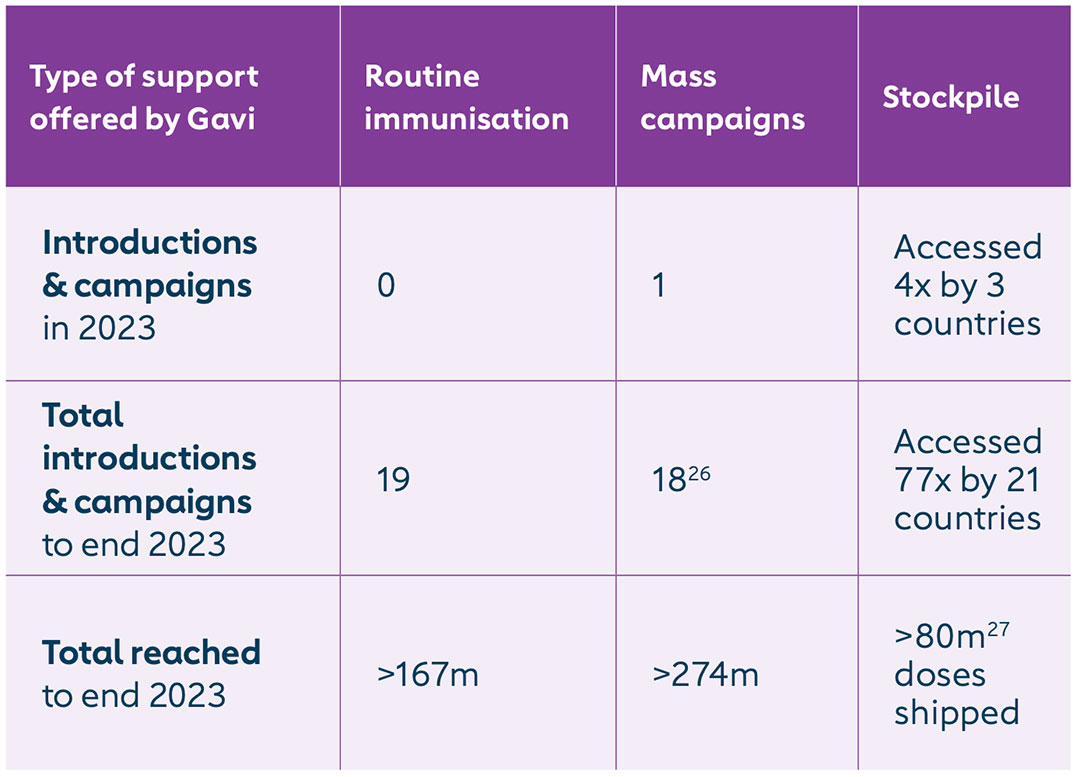
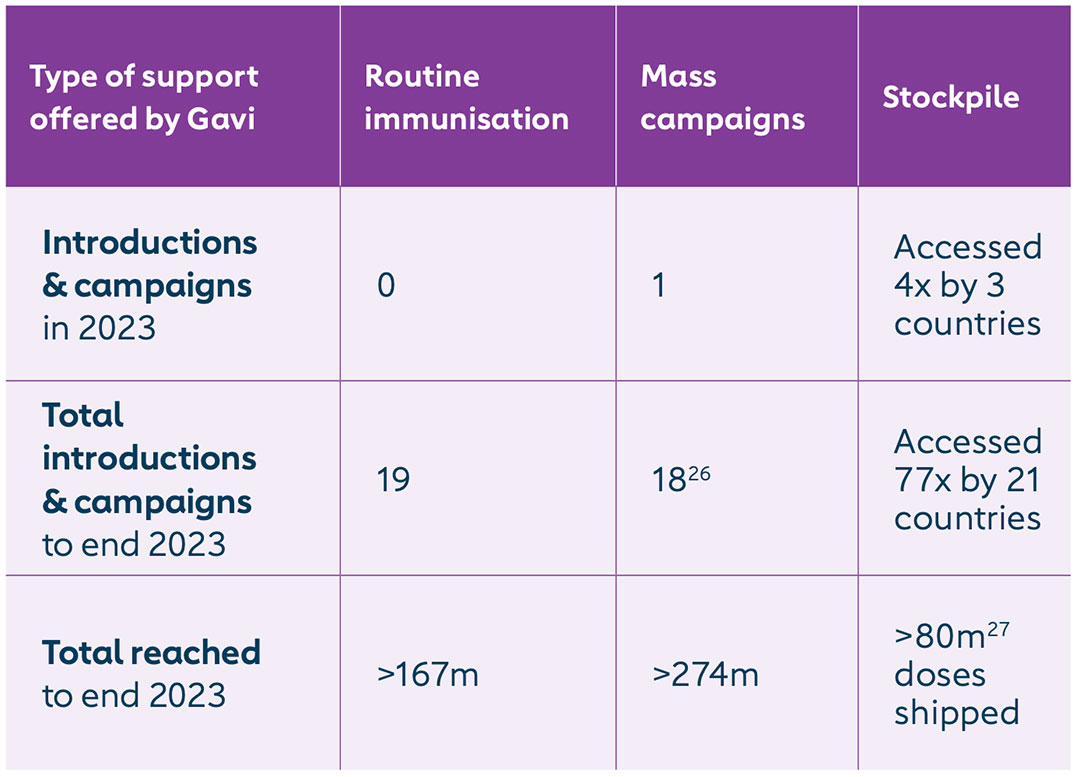
By end 2023, Gavi-supported yellow fever vaccine mass campaigns had reached more than 274 million children and adults in 18 countries in Africa; and more than 167 million children in 19 countries in Africa had been immunised through routine programmes. By end 2023, the Gavi-funded yellow fever vaccine emergency stockpile had been accessed 77 times by 21 countries, with more than 80 million doses shipped for outbreak response.
In June 2023, Uganda launched phase 1 of a preventive mass vaccination campaign (PMVC) targeting more than 13 million people (aged 9 months to 60 years). Phases 2 and 3 will be conducted in subsequent years. Nigeria and the Democratic Republic of the Congo (DRC) continued roll-out of multi-year phased campaigns. Ethiopia and South Sudan remain the only countries in the WHO African Region (AFRO) at high risk of yellow fever yet to introduce the vaccine. Routine coverage remains suboptimal in most AFRO countries, and ten countries reported probable or confirmed cases of yellow fever – most had introduced yellow fever vaccine and completed a PMVC, often years ago, indicating the likelihood of significant immunity gaps within the current population. In 2023, three countries made a total of four outbreak response requests to vaccinate over 1 million people. This indicates growing immunity gaps -that could be most expeditiously addressed through preventive campaigns targeting birth cohorts not eligible since the PMVC.
The issue
Yellow fever is an acute viral haemorrhagic disease transmitted by mosquitoes of the Aedes and Haemagogus genera. Yellow fever causes devastating epidemics in areas where infected mosquitoes bite people who are not vaccinated. Death rates can be as high as 50% among those severely affected.
As of the 2024 risk assessment, 27 countries in Africa and 13 countries in the Region of the Americas are at high risk for yellow fever. The burden of yellow fever in Africa and South America in 2018 was estimated at 109,000 severe infections (95% credible interval [CrI] [67,000–173,000]) and 51,000 deaths (95% CrI [31,000–82,000]).1 Rapid urbanisation encroaching on nature, climate change and conflicts have exacerbated the issue. Cities provide fertile breeding grounds for mosquito larvae, as stagnant water collects in water containers, cans and tyres. Frequent travel by workers between forests or peri-urban areas with ongoing disease transmission and urban centers significantly increases the risk of initiating an urban transmission cycle. This risk is particularly high in areas where Aedes aegypti mosquitoes are present, and preventive measures or effective control strategies are lacking.
Climate change and human behaviour are influencing the risk of yellow fever. Changes in rainfall and temperature interfere in the sylvatic and mosquito transmission dynamics cycle, increasing the risk of zoonotic spillover from the sylvatic reservoir in non-human primates (NHP).2 Finally, conflict leads to population movements, increasing their risk of infection and reducing their access to routine immunisation programmes.
Gavi’s response
While yellow fever cannot be eliminated, one injection provides life-long protection. The risk of outbreaks can be substantially reduced by immunising at least 60-80% of the at-risk population. To achieve this high coverage and maintain immunity for life in the high-risk Gavi-eligible countries in Africa, Gavi currently supports:
- Preventive campaigns: Eligible countries receive support for preventive mass vaccination campaigns (PMVCs) targeting populations aged nine months up to 60 years on a one-dose vaccination schedule, as well as associated supplies. Achieving high coverage in these campaigns is key to reducing the risk of outbreaks and mitigating vaccine-preventable yellow fever deaths. Gavi has supported PMVCs since 2006.
- Introduction into the routine immunisation system: For countries introducing the vaccine to the routine immunisation programme for the first time, Gavi provides support for a one-dose vaccination schedule, as well as associated injection supplies. For the first year of introduction, Gavi supports a one-time vaccine introduction grant; and government or partners cover the remaining costs associated with the vaccine introduction. Gavi has supported yellow fever vaccination in routine immunisation since its inception in 2000.
- Yellow fever emergency stockpile: Countries eligible for Gavi support can rely on the Gavi-funded global stockpile of yellow fever vaccine for use in emergency outbreaks. This is managed and accessed through the International Coordinating Group (ICG) on Vaccine Provision. Gavi-funded stockpiles are open to all countries, but their use must be reimbursed by countries that are not eligible for Gavi support. Gavi has supported the yellow fever vaccine emergency stockpile since 2002.
- Diagnostics: Gavi supports countries to increase their testing capabilities with diagnostics, reducing yellow fever testing timelines and increasing immunoglobulin M (IgM)-positive specimens referred for confirmatory testing. Gavi support has broadened validated testing technologies; and strengthened laboratory capacity through regional workshops, WHO technical guidance and performance evaluations resulting in the procurement of three new quality-assured commercial assays. As a result of Gavi’s catalytic investments, at least three suspected outbreaks since 2019 were found not to be yellow fever, saving Gavi approximately US$ 18–40 million by averting vaccination campaigns.
Gavi’s yellow fever vaccine programme works in close partnership with the Eliminate Yellow Fever Epidemics (EYE) global strategy, housed in the World Health Organization (WHO). Gavi’s support primarily feeds into strategic objective 1: protect at-risk populations; 2: prevent international spread; and 3: contain outbreaks rapidly. Gavi played a crucial role in the midterm evaluation of the EYE Strategy conducted from 2022–2023. This evaluation highlighted significant achievements during the strategy's first five years (2017–2021), including the vaccination of 185 million people in yellow fever high-risk countries in Africa; a 75% increase in vaccine supply for Gavi-eligible countries; and improvements in laboratory capacity and international clinical specimen transportation systems, which led to faster outbreak containment and enhanced diagnostics.
From other sites
1. https://pubmed.ncbi.nlm.nih.gov/33722340/ 2. https://pmc.ncbi.nlm.nih.gov/articles/PMC7386919/pdf/elife-55619.pdf