Beyond cervical cancer: How Bhutan is winning the war against HPV
The small Himalayan country of Bhutan plans to eliminate cervical cancer, and sees vaccinating boys as well as girls as being crucial to that goal.
- 16 March 2023
- 11 min read
- by Linda Geddes

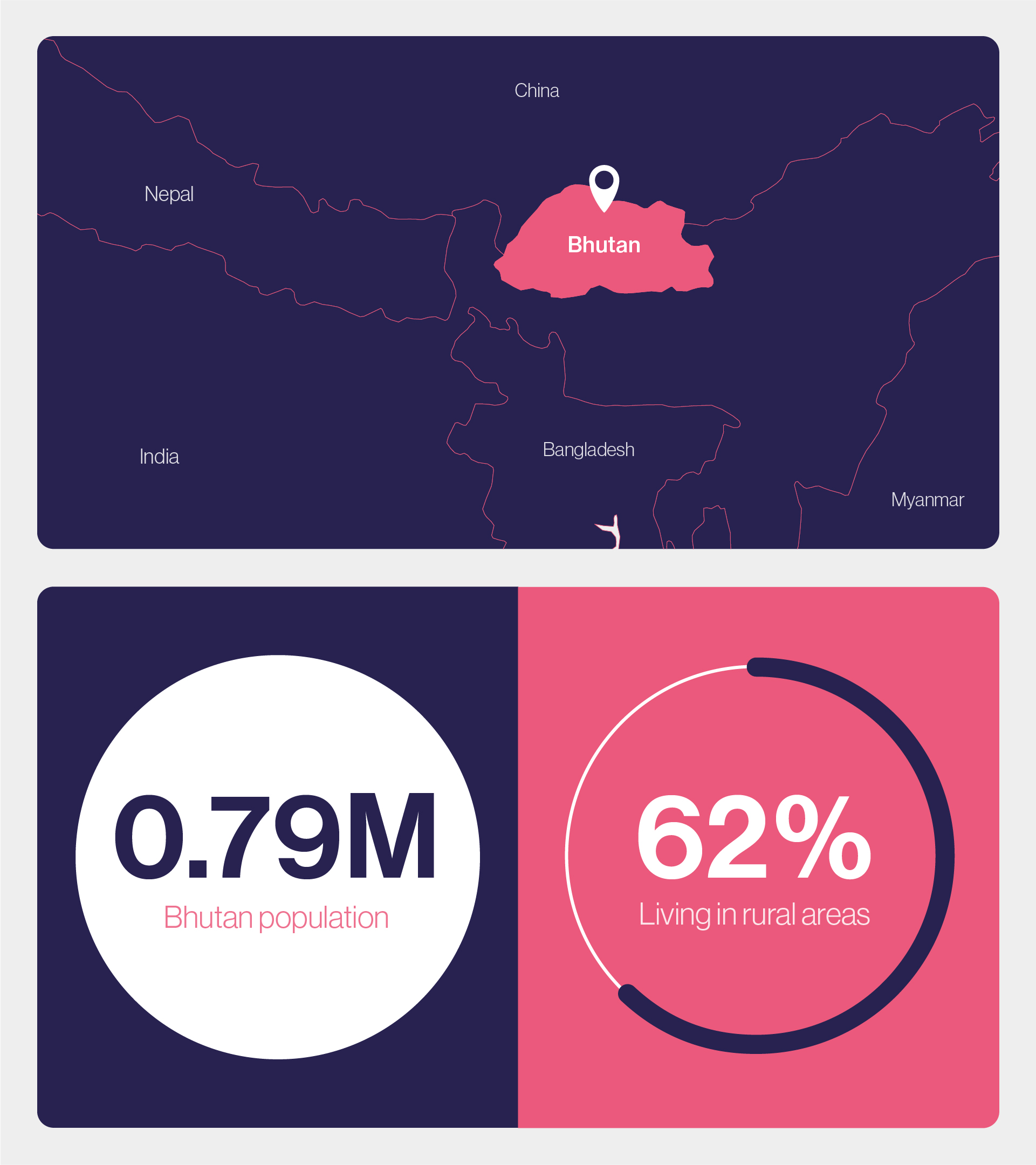
Criss-crossed by mountains and with relatively few doctors and nurses, the small Himalayan nation of Bhutan may seem an unlikely forerunner in the global fight against human papillomavirus (HPV). But while many low- and middle-income countries (LMICs) have begun vaccinating girls against this leading cause of cervical cancer, Bhutan has gone a step further and begun vaccinating boys as well – one of the only LMICs in the world to do so.
Worldwide, HPV is responsible for approximately 4.5% of cancers, equivalent to some 630,000 new cases each year.
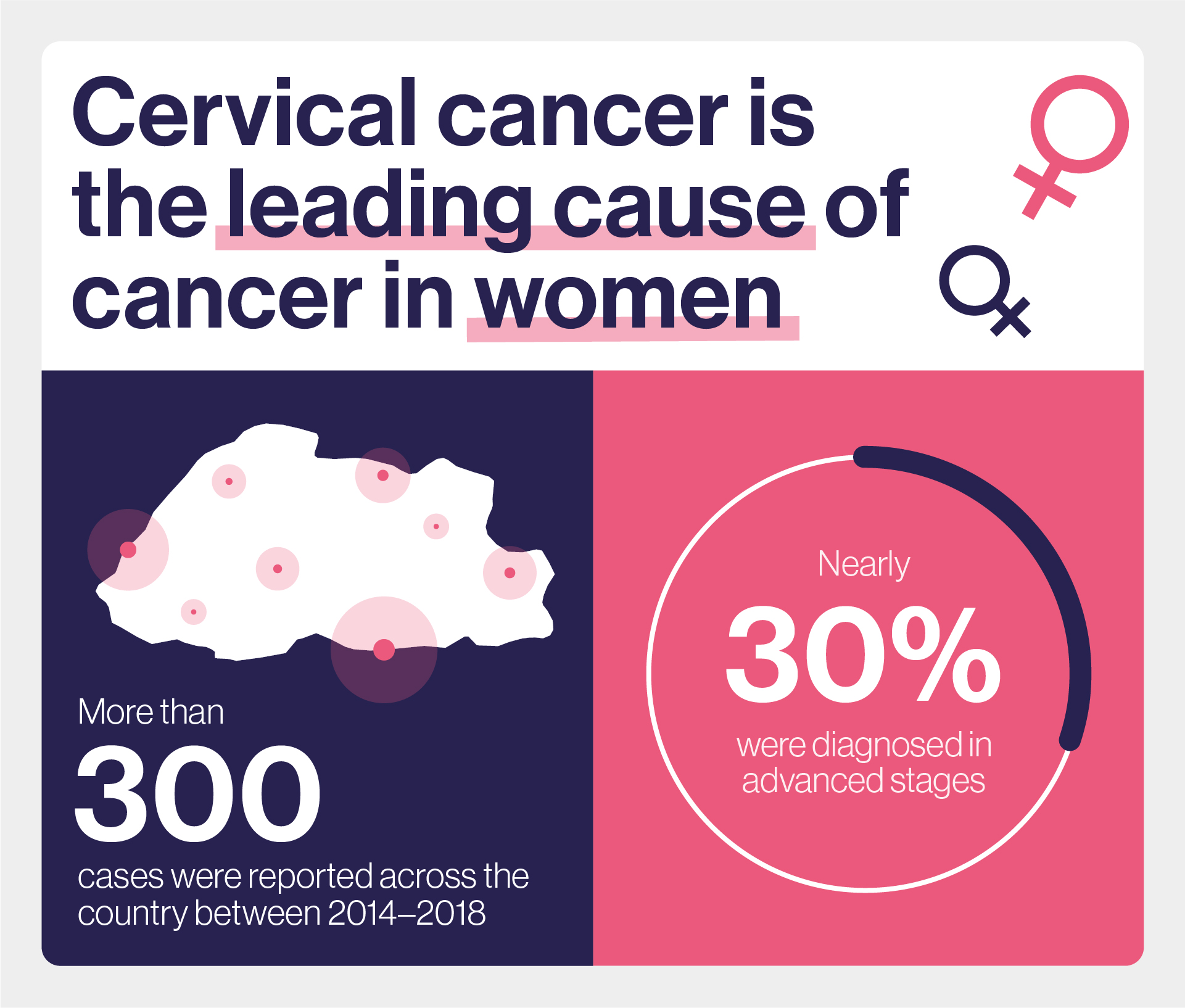
Its primary aim is to prevent cervical cancer, the most common cancer among women in the country. The World Health Organization (WHO) estimates that 342,000 women die each year from cervical cancer, 90% of whom are in LMICs. "Vaccinating both sexes can help prevent the transmission of the HPV, which is the primary cause of cervical cancer," Bhutan's health minister, Dr Dechen Wangmo, said.
However, the ultimate goal istoeliminate all HPV-related diseases – which include genital warts and a substantial proportion of anal, vulval, penile and head and neck cancers – in both women and men.
Gender-neutral vaccination
Though rare among LMICs, Bhutan's approach is gaining traction in other nations as well. In early 2021, the European Union launched its Beating Cancer Plan, which committed to preventing all cancers caused by HPV through gender-neutral HPV vaccination, with the goal of vaccinating 90% of adolescent girls and significantly higher numbers of boys by 2030.
Meanwhile, Australia, which has been vaccinating girls against HPV since 2007, and boys since 2013, is on track to eliminate the most harmful HPV subtypes from its population. "They haven't done it yet, but they are definitely on their way," said Prof Lynette Denny, director of the Gynaecological Cancer Research Centre at the University of Cape Town, South Africa. "The programme has been so unbelievably successful, that the incidence of genital warts, which are caused by HPV types 6 and 11, has dropped to virtually zero among vaccinated populations."
Yet, global health agencies are still focusing on vaccinating girls. In 2020, WHO launched its 'Global strategy to accelerate the elimination of cervical cancer as a public health problem' setting targets for 90% of girls to be fully vaccinated against HPV by age 15 years; 70% of women screened with a high-performance test; and 90% of women identified with cervical disease to receive treatment – all by 2030.
Gavi's Board also recently relaunched its HPV vaccine programme, with more than US$ 600 million of funding committed towards purchasing vaccines, strengthening health systems and providing technical and learning support. The Alliance hopes to deliver HPV vaccine to more than 86 million girls by 2025 and avert more than 1.4 million deaths from cervical cancer. In line with WHO guidance, Gavi's support is also focused on girls aged 9 to 14 years.
The costs and benefits of vaccinating boys are still heavily debated. The burden of HPV-associated disease is predominantly borne by women in the form of cervical cancer. "The reason girls are vaccinated against HPV, is because that's where you get the biggest bang for your buck," said Denny. "The proportion of the population who get penile, oropharyngeal (a type of head and neck cancer) and anal cancer is minute compared to the number of women who get cervical cancer."
HPV vaccination programmes for girls are also relatively expensive to implement – adding boys would increase these costs. What's more, global supplies of HPV vaccine are limited, so vaccinating boys could reduce the availability of doses for girls. On the other hand, some argue that female-focused vaccination targets miss the fact that HPV is mainly transmitted from men to women, or men to men, during sexual intercourse. Vaccinating boys as well as girls would not only help to reduce rates of cervical cancer – it would drastically reduce rates of other HPV-associated disease as well.
Killer virus
HPV belongs to a family of viruses that infect cells buried in the lining of our reproductive organs, throat and anus. Most sexually active men and women will be infected with it at some point in their lives, and some may be repeatedly infected – but not all types of HPV trigger cancer, and many of those who become infected will clear the infection and remain cancer-free.
However, infection with certain types of HPV – particularly types 16 and 18 –- significantly increases the risk of cancers developing. This is because these viruses hijack infected cells and force them to proliferate, creating more copies of themselves in the process. The viruses also prevent cells with damaged DNA from destroying themselves, and their unrestrained growth can ultimately lead to cancer.
Worldwide, HPV is responsible for approximately 4.5% of cancers, equivalent to some 630,000 new cases each year. About 570,000 of these cancers are in women, and the majority of them (530,000) are cervical cancers – hence the focus on vaccinating girls before they become sexually active.
Male disease
While most HPV-related cancers are cervical cancer, robust cervical cancer screening – including many high-income countries – have been effective at detecting and treating cases early. This means that now, other HPV-related cancers in men and women now have an equivalent prevalence to cervical cancer. In the US, for instance – where nearly 45,000 HPV-associated cancers are diagnosed each year – around 40% of these cancers are now in men.
"These other cancers are proportionally important in places such as the US because they're not screened for and they're not prevented," said Dr Gary Clifford, an epidemiologist in the International Agency for Research on Cancer's Early Detection Prevention and Infections section.
Rates of these cancers are also increasing in many countries – most likely because more relaxed attitudes to sex and morality in recent decades have increased people's exposure to HPV.
"The increase in these other HPV-associated cancers is likely what we would have observed also for cervical cancer, if we hadn't been preventing it through screening," Clifford said.
Effective screening methods for these other types of cancer don't currently exist. But because the HPV vaccine doesn't discriminate between cancer sites, many of these cases could potentially be prevented by extending HPV vaccination to boys. As of 2022, 125 countries had introduced HPV vaccine in their national immunisation programmes for girls, and 47 countries were also vaccinating boys.
Girls before boys
Well-intentioned as these efforts are, they have also created some issues with HPV vaccine supply. In 2019, WHO called on countries with gender-neutral HPV vaccination programmes to suspend them, until all girls who needed the vaccine could get it. Its Strategic Advisory Group of Experts on immunisation (SAGE) was concerned that shortages of the vaccine could result in failure to introduce or sustain programmes in certain countries – particularly those with a high burden of cervical cancer. The International Papillomavirus Society (IPVS) has predicted that these vaccine shortages could last until 2023-25.
Have you read?
For now, at least, the WHO recommends prioritising HPV vaccination in girls aged 9 to 14 years – which, it says, also reduces the risk of HPV infection in boys. According to its latest position paper on HPV vaccines, vaccination of older girls and women, boys, and older males "is recommended only if this is feasible and affordable, and does not divert resources from vaccination of [girls] or effective cervical cancer screening programmes".
Clifford agrees with the WHO's position of prioritising girls for HPV vaccination – especially in lower-income countries where the cervical cancer burden is greatest, and successful screening programmes still don't exist: "Even if you are already vaccinating girls, probably the best investment you can make is to try and further improve your vaccine coverage in this group, because it is rarely optimal."
Yet, gender-neutral vaccination against HPV carries a number of additional advantages. For one thing, it simplifies the public health message, which may increase vaccine uptake. It may also make vaccination programmes more resilient to disruption. "If a programme suffers temporary problems, such as we have seen with the COVID-19 pandemic or media scares, having had both sexes vaccinated provides more time for the programme to recover," Clifford said.
Vaccinating boys also benefits women and girls, by reducing circulation of HPV and their chances of becoming infected with it. Eventually, it should also reduce rates of anal, penile and head and neck cancers in men – although most boys who have been vaccinated have not yet reached the age where these cancers start to occur.
Vaccinating boys also benefits women and girls, by reducing circulation of HPV and their chances of becoming infected with it. Eventually, it should also reduce rates of anal, penile and head and neck cancers in men.
"It is fair to say that even vaccinating girls at high coverage offers a lot of protection to the boys. But that does create an equality issue for homosexual males, who are not really offered much herd immunity through female-only vaccination," said Clifford. "Gender-neutral vaccination has the advantage of protecting all men and boys, before they, society, or any health worker, has to identify what their sexuality is."
The reduction in genital warts is another bonus. Though painless and benign, these fleshy growths around the genital or anal areas can still cause considerable damage to people's health. "For some of our female patients, the psychological impact is as bad as cancer," said Denny. "They have these huge, disfiguring cauliflower-like lesions on their vulvas, which are so psychologically and emotionally damaging that some women would rather die than live with them.
Equitable healthcare
Bhutan was the first LMIC to introduce a nationwide HPV vaccination programme for girls aged 12 to 18 in 2010. A year later, this was mainstreamed into a routine immunisation programme for 12-year-old girls, delivered through schools.
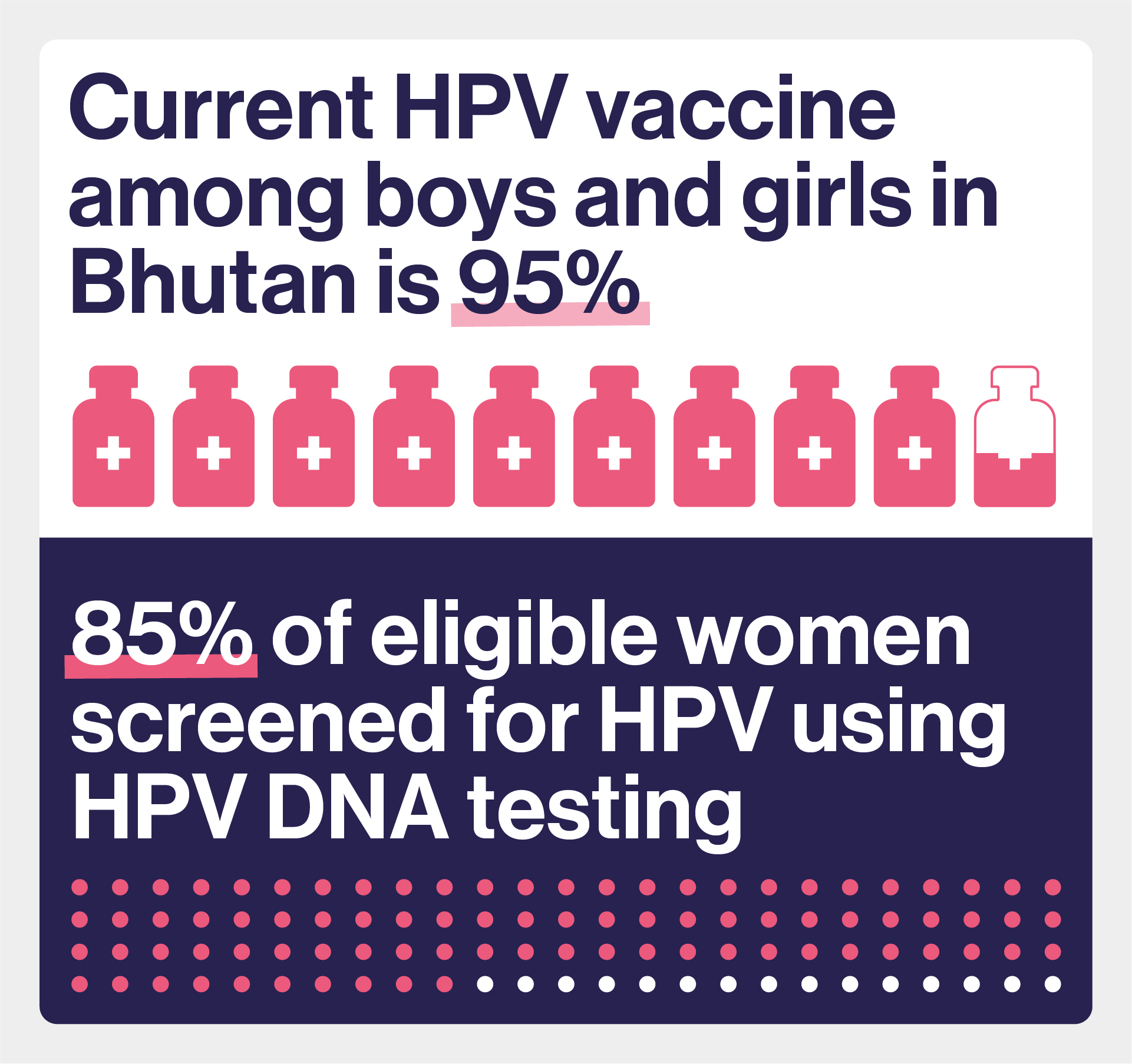
"The campaign was a resounding success, with reported initial coverage reaching about 95% of girls in the target age group," said Wangmo.
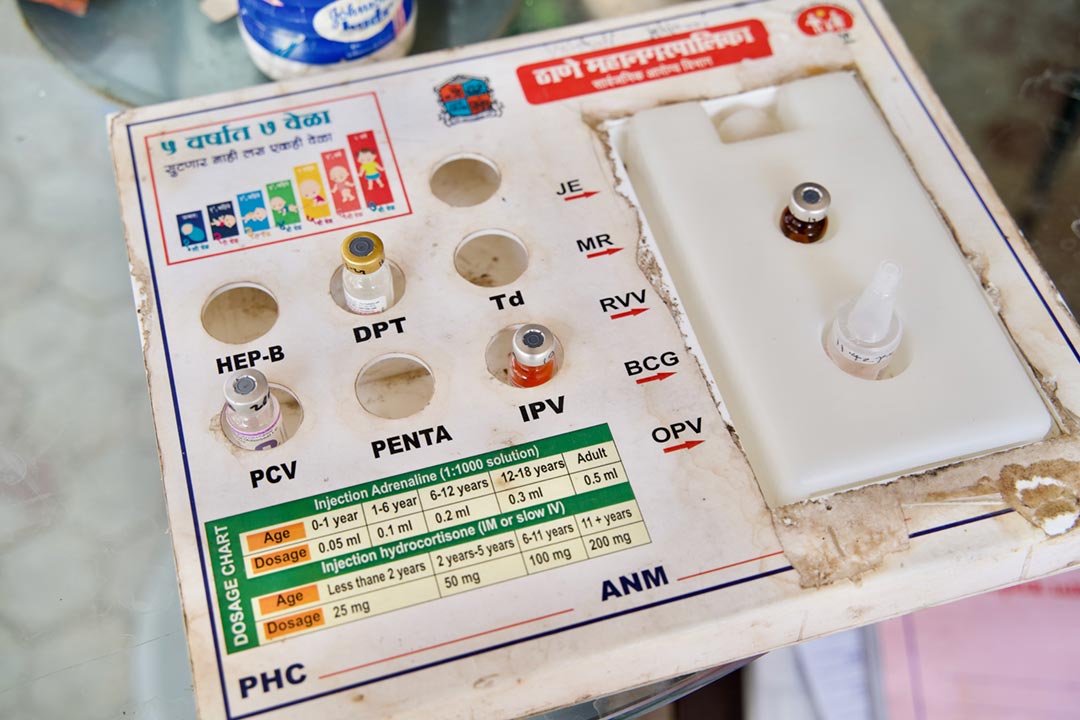
Bhutan launched its cervical cancer elimination programme in 2019 – a year before WHO's global strategy. In addition to vaccinating both girls and boys against HPV achieving 90% coverage, the country has introduced HPV DNA testing for all women aged 30 to 69,with those who test positive offered further tests and treatment for pre-cancerous cells.
"Bhutan has made significant progress in increasing access to healthcare in recent years, and the gender-neutral vaccination programme is also a reflection of our commitment to ensuring equitable quality access to healthcare services for all," says Wangmo.
Despite economic and infrastructure challenges, with rugged terrain and poor road connectivity limiting access to hospitals, Bhutan has a free healthcare system, and a well-established network of primary healthcare clinics. Bhutanese people tend to place high levels of trust in their political leaders – which include several doctors and public health experts – and levels of vaccine hesitancy within the population are low.
Wangmo credits Bhutan's good healthcare system, strong political and leadership commitment to reducing cervical cancer, uninterrupted supply of HPV vaccine, and strong advocacy and awareness programme for these high coverage rates. Following the same, school-based implementation strategy, for boys and girls has also helped, she said.
Expanded access
So, could other LMICs follow suit? "Bhutan is quite a special and unique place. It is a fairly small country, very strong on public health," said Clifford. "They are committed to eradicating cervical cancer by taking all the steps possible."
For as long as global HPV vaccine supply remains limited, wider introduction of HPV vaccination for boys in other LMICs seems unlikely. Many countries would also struggle to afford additional doses without additional support.
However, this could change if vaccine doses became cheaper. In 2021, a Chinese-made HPV vaccine called Cecolin received WHO prequalification – meaning it meets strict international quality, safety, and efficacy standards —a crucial step towards entering the global vaccine market. It protects against HPV types 16 and 18, which cause about 70% of cervical cancers.
Then, in January 2023, the Serum Institute of India launched the country's first "home-grown" HPV vaccine domestically, which protects against the same 4 HPV types as Merck's quadrivalent Gardasil vaccine – including types 16 and 18 – at a fraction of the cost. India bears a fifth of the world's cervical cancer burden, with 123,000 new cases of cervical cancer and 67,000 deaths each year, but SII ultimately hopes to produce its vaccine for the global market.
This increased competition should theoretically drive down vaccine prices, which could make widespread gender-neutral HPV vaccination a more realistic prospect.
"Affordability has been an issue in recent years with reduced supply and high-income countries expanding to gender-neutral vaccination quicker than expected – meaning those that could afford to pay took twice as many doses – creating further difficulties for poorer countries that needed them most," said Clifford.
Also important, is the outcome of a recent review by the WHO's SAGE group, which concluded that that a single-dose of approved HPV vaccines provides comparable efficacy to two or three-dose regimens. Delivering a single dose would be less costly and require fewer resources, helping to bring the WHO's goal of 90% of 15-year-old girls being fully vaccinated against HPV within reach. Targeting boys might be a logical next step.
Achieving any of this will require strong political commitment and focus, but cervical cancer alone kills some 300,000 women each year – often in the most active phase of their economic and social lives. Thanks to vaccines, HPV-associated diseases are also preventable, and most can be successfully treated if they are detected early enough. Bhutan, at least, believes the investment is worth it.
More from Linda Geddes
Recommended for you