What can we learn from HPV vaccine delivery costs?
New study results can inform planning and budgeting for sustainable human papillomavirus vaccination programs.
- 15 November 2023
- 4 min read
- by PATH

Human papillomavirus (HPV) vaccines are unique in the world of routine immunization due to their timing. Many vaccines are given to young children, but HPV vaccination occurs at adolescence, when pediatric visits are no longer routine. As HPV vaccine delivery strategies to reach this population vary by country, so does program cost.
PATH recently worked with immunization program managers on a study to assess operational context and estimate ongoing costs of HPV vaccine delivery (excluding the cost of vaccines and supplies) beyond the introduction years. The study generated evidence on delivering a two-dose HPV vaccination schedule in six countries: Ethiopia, Guyana, Rwanda, Senegal, Sri Lanka, and Uganda.
The results, described below and recently published in the journal Vaccine, shed light on the operational context and costs per HPV vaccine dose delivered. They point to key opportunities that policymakers may wish to consider for greater cost efficiencies, particularly as programs seek to rebuild and accelerate coverage after the acute phase of the COVID-19 pandemic.
Operational context and service volume impact vaccine delivery costs
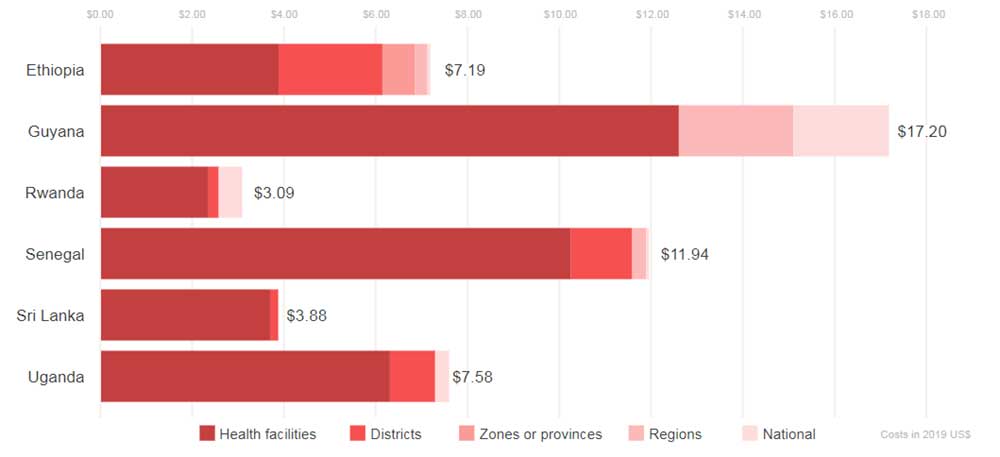
HPV vaccine delivery cost per dose varied widely across the study countries based on operational context (frequency and intensity of program implementation activities in each country) and service volume (number of doses delivered).
All immunization programs conduct ongoing activities, such as program planning and management, social mobilization, crisis management, and vaccine distribution and storage. "For HPV vaccination program activities, varying levels of engagement in these activities were apparent within and across countries, depending on context," said Rose Slavkovsky, MPA, health economics program officer at PATH and one of the study authors. "For example, training and crisis management activities were at lower intensities in Rwanda, the longest-running HPV vaccination program in this study sample. Conversely, sustained levels of social mobilization and program planning were apparent in several study countries."
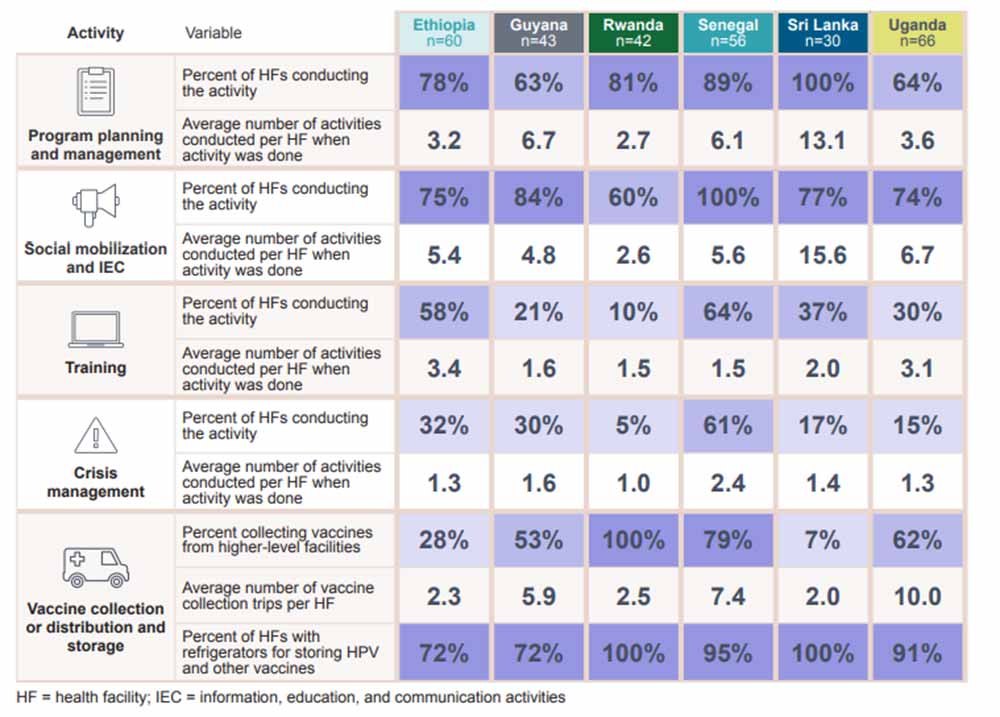
Varied service delivery intensity also contributed to differences in cost estimates across countries. Service volume was important because a lower number of doses delivered per health facility meant a higher cost per dose. The average number of doses delivered per health facility varied by country, as did the frequency of conducting HPV vaccination sessions and other program activities (fixed time points in Ethiopia versus year-round vaccination in Senegal, for example).
Despite the differences among the study countries, there were a couple notable trends. Activities and expenditures at health facilities contributed the largest proportion of the economic cost per dose (see figure below).
Have you read?
Additionally, the largest proportion of costs were opportunity costs. Separate from financial costs that measure direct expenditures, opportunity costs measure the value of existing resources (sometimes shared with other health programs) used by the HPV vaccination program. Of these, health worker and non-health worker time were the largest cost category across study countries, regardless of operational context. Direct expenditures accounted for a smaller share of the delivery costs.
Strategies to decrease HPV vaccine delivery costs
When more doses are delivered, resources are spread over a larger denominator, contributing to a lower cost per dose. A strategy to increase the number of doses delivered could include concurrently vaccinating multiple cohorts. Additionally, adopting a single-dose vaccination schedule, endorsed in December 2022 by the World Health Organization as an alternative to the current two-dose schedule evaluated in this study, could reduce the delivery cost per fully vaccinated child.
The study team used data from five of the six study countries to model the potential cost implications of implementing this single-dose schedule. This modeling analysis found that, although the estimated financial costs per dose for HPV vaccine delivery could increase because of the smaller number of doses delivered, the financial cost per fully vaccinated child could decrease by nearly half (excluding the cost of vaccine).
Economic cost, which is the sum of both financial and opportunity costs, also decreases significantly per fully vaccinated child on a single-dose schedule.
Reducing the costs of cervical cancer
Studies such as this one demonstrate how improving our understanding of the operational context and costs of vaccine delivery can help improve or reaffirm current strategies in not just the study countries, but other low- and middle-income countries (LMICs) as well. Cervical cancer is still a leading cause of cancer in women in LMICs, but widespread access to HPV vaccines would dramatically reduce the number of cases.
"The potential impact of more widespread HPV vaccine access on the health of women and girls is profound," said Mercy Mvundura, PhD, health economics technical advisor at PATH and study lead. "Our hope is that these study findings will inform planning and decision-making to revitalize cancer-preventing HPV vaccination programs, especially as health systems recover from COVID-related interruptions."
Website
This article was originally published by PATH on 13 November 2023.
More from PATH
Recommended for you