Could I have whooping cough?
Pertussis, or whooping cough, is on the rise in the UK and North America, but viral coughs are also common. So, how can you tell the difference?
- 15 March 2024
- 6 min read
- by Linda Geddes

Pertussis is caused by a bacterium called Bordetella pertussis, which is passed from person to person by coughing, sneezing or sharing the same breathing space.
The illness usually starts with mild, cold-like symptoms, a low fever, and occasional coughing. Some babies and young children may temporarily stop breathing (apnoea) and turn blue or purple. These early symptoms can last for one to two weeks, and because they often resemble the common cold, doctors may not suspect or diagnose whooping cough until later in the illness.
The next phase is characterised by violent coughing fits lasting several minutes each, which usually recur for one to six weeks, although they can last up to ten weeks – in China pertussis is known as the 100-day cough.
[Pertussis] tends to trigger violent and uncontrolled fits of coughing, interspersed with a loud, high-pitched “whoop” sound as individuals try to draw breath.
Recovery takes several more weeks, with the cough gradually becoming milder and less common, although coughing fits may return if the person catches another respiratory infection.
Antibiotics can reduce the severity of the infection and prevent it from spreading to others, but these need to be started early – ideally before the coughing fits begin. Starting antibiotic treatment after three weeks of illness is unlikely to help, because the body has usually cleared the bacteria by then and the ongoing cough is due to damage they have already inflicted.
How common is it?
Worldwide, there are an estimated 24.1 million cases of pertussis each year, although the true prevalence is unknown because it is likely that many cases are not diagnosed. The illness is thought to be a frequent cause of prolonged coughing in adults and adolescents. However, it is most dangerous for babies, who often don't cough at all, but temporarily stop breathing, turn blue, and may experience seizures or brain damage.
Before vaccines were developed, the disease killed one in every ten children who became infected. Even now, approximately one third of infants under the age of one who become infected require hospital care, and one out of 100 who receive hospital treatment die.
Can I catch it if I've been vaccinated?
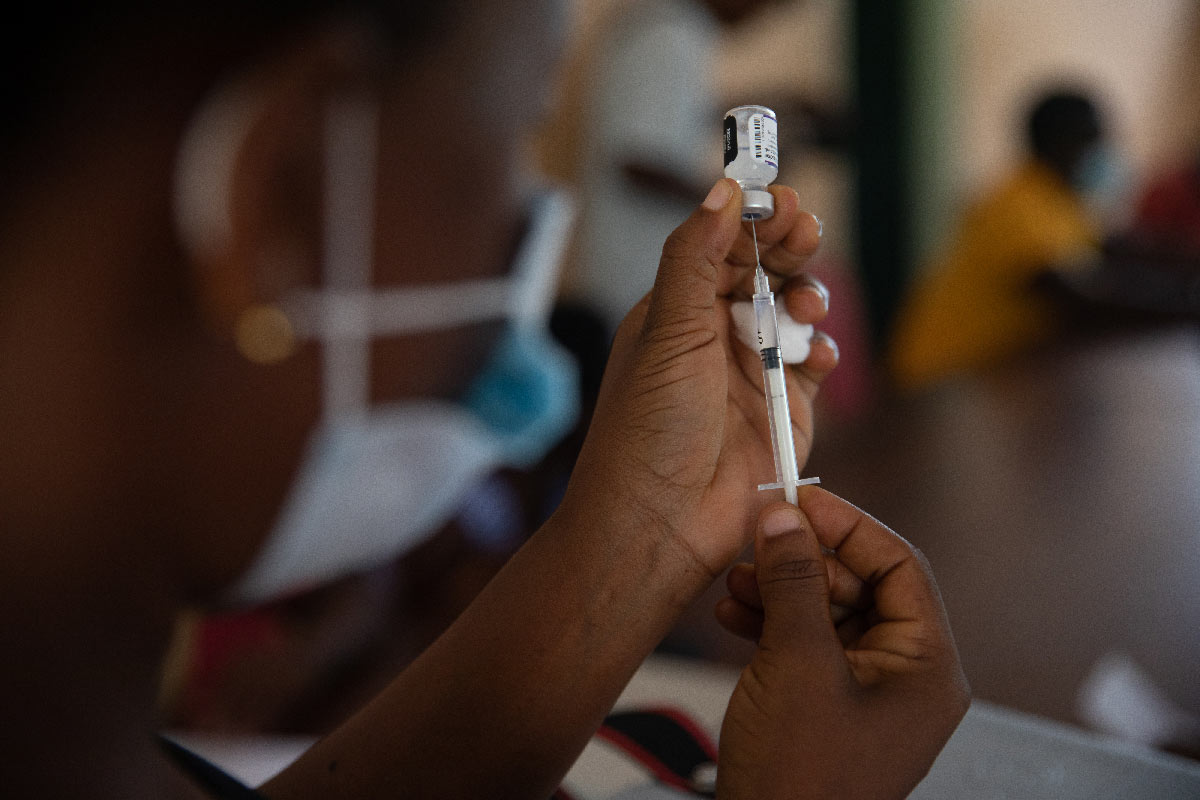
Infants are usually immunised against pertussis alongside other infections, including diphtheria and tetanus, as part of their routine childhood immunisations. The World Health Organization (WHO) recommends providing all infants with three doses of pertussis vaccine in infancy, with one booster dose in children one to six years of age. Some countries also offer booster doses to adolescents and adults, as well as to pregnant women to protect their newborn infants, who cannot be vaccinated yet.
Pertussis vaccines reduce the risk of severe disease in infants and young children – the group at greatest risk of hospitalisation and death.
However, while vaccinated children are far less likely to develop pertussis than unvaccinated children, this protection isn't lifelong. One study, which evaluated the effectiveness of pertussis vaccinations in Canada, found that vaccines provided 80% protection against infection during the first year after vaccination, 84% protection over the next three years, but that immunity started to wane beyond four years, with little to no protection beyond seven years from the last vaccination.
Even so, the disease tends to be milder, and shorter-lived in people who have been vaccinated. "The whooping cough vaccine is highly effective at preventing severe disease and complications. Protection from the vaccine does wane over time in the same way that protection built up from natural infection does, but the primary purpose of the vaccine programme is to prevent severe disease in those at highest risk, including young infants, and the combination of maternal and infant vaccination is highly effective in achieving this," said Dr Gayatri Amirthalingam, Consultant Medical Epidemiologist, Immunisation and Vaccine Preventable Diseases Division at UK Health Security Agency (UKHSA).
How do you distinguish whooping cough from other coughs?
Pertussis cases often peak during summer and autumn, but the UK has been logging larger than normal numbers of infections over the past few months, even though it is winter there. However, there are also plenty of other respiratory viruses co-circulating, with adenovirus, parainfluenza and human metapneumovirus (hMPV) all recently peaking or showing continued upwards growth in the UK.
All of these can cause a cough, although the type of cough differs, even within the same group of viruses. For instance, parainfluenza viruses can cause a mild cough, a persistent cough with mucus, or a barky, seal-like cough and a high-pitched, squeaky noise with breathing (croup). Adenoviruses can also cause croup.
Have you read?
Then there's respiratory syncytial virus (RSV), which is also common during autumn and winter and typically causes a wet-sounding, forceful cough.
Pertussis is a little different. It tends to trigger violent and uncontrolled fits of coughing, interspersed with a loud, high-pitched "whoop" sound as individuals try to draw breath. These coughing fits may last for several minutes, are more common at night and may be so severe that they cause retching, vomiting, loss of bladder control or fractured ribs. People may feel very tired after coughing fits, but otherwise well in-between.
Children also often make the characteristic whooping sound, but not everyone with pertussis whoops, so you shouldn't rely on this for diagnosis. Babies may not cough at all, but rather turn blue or struggle to breathe. They can also go on to develop other complications including pneumonia or seizures.
When should I consult a doctor?
If you suspect that you or someone in your household has whooping cough, you should consult a health care professional as soon as possible – particularly if the patient is under six months old, has a very bad cough that is getting worse, has a weakened immune system, or has been in contact with someone with whooping cough and is pregnant. Because it is very contagious, it is best to telephone the health care facility before you visit.
You should also seek emergency care if the patient's lips, tongue, face or skin suddenly turn blue or grey (this is easier to see on palms of the hands or soles of the feet on black or brown skin), if they are struggling to breathe, have chest pain that is worse when breathing or coughing, or are experiencing seizures.
Even if you have been coughing for more than three weeks and aren't getting any worse, you should still consult a doctor, because there could be various reasons for this, Amirthalingam said: "In instances where whooping cough is suspected, it is also important to contact the doctor, because the case will be reported to the local public health team, which will help determine if further follow-up is required with their close household contacts, such as administering antibiotics as a preventative treatment and vaccination," she added.
More from Linda Geddes
Recommended for you