Genomic data sheds light on monkeypox origins
The current monkeypox outbreak arose from a single human case, amplified through one or more super-spreader events, according to new research.
- 24 June 2022
- 4 min read
- by Linda Geddes

The current monkeypox outbreak continues to perplex experts. Previous cases outside West and Central Africa, where the disease is endemic, spread to only a few people before transmission stopped. However in this outbreak, since the first case was reported in the UK on 7 May, 2022, more than 2,500 cases have been confirmed worldwide (as of 18 June). Now, a new genomic analysis – a study of the virus's genetic makeup – has shed fresh light on how the outbreak began, and how the virus is evolving as it spreads.
To investigate how the 2022 outbreak began, João Paulo Gomes at the National Institute of Health Doutor Ricardo Jorge (INSA) in Lisbon, Portugal and colleagues analysed viral genome sequences sampled from 15 infected individuals, to better understand the nature of the virus’s genetic mutations.
What is the research about?
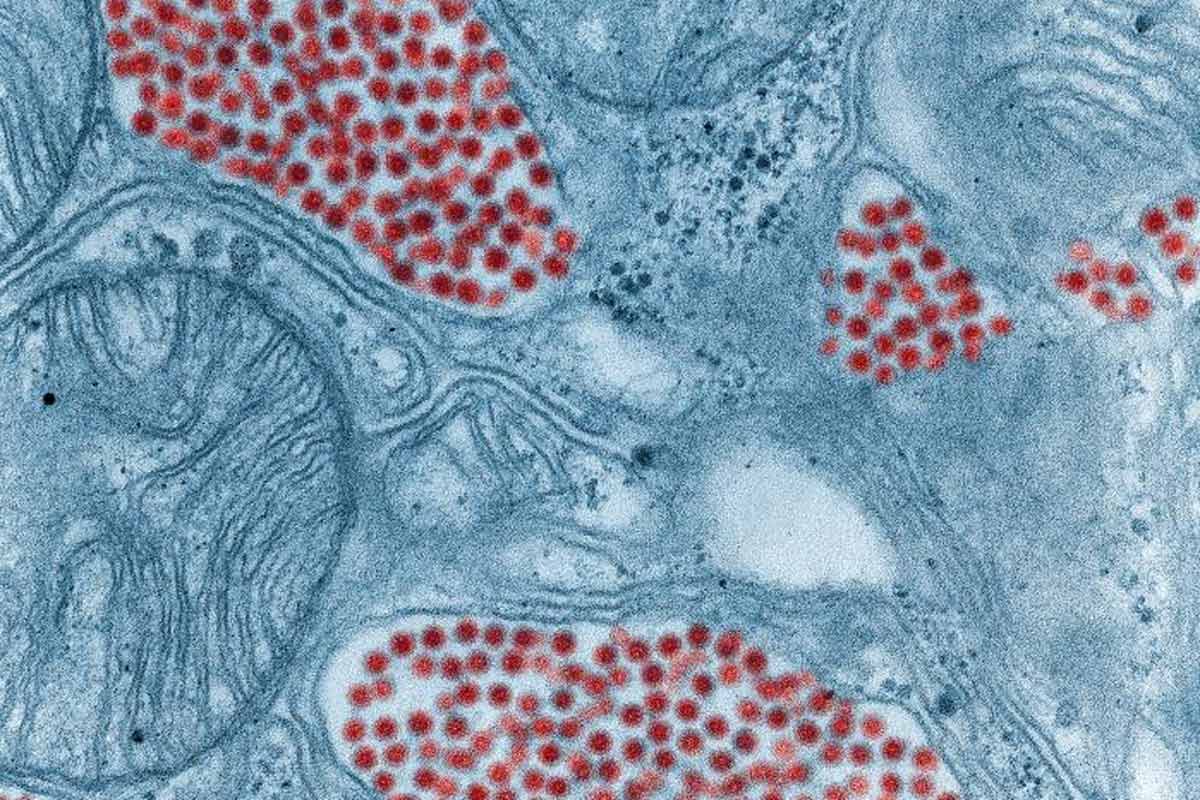
Monkeypox is an infectious disease caused by the monkeypox virus, typically carried by livestock and other animals. Occasionally, it spreads from animals to humans, which is how the current outbreak is thought to have started. Usually, such human outbreaks quickly fizzle out, but this one is unusual in that it has affected thousands of people in multiple countries. Understanding whether the virus has mutated, and the nature of any such changes, is therefore important.
What did the researchers do?
To investigate how the 2022 outbreak began, João Paulo Gomes at the National Institute of Health Doutor Ricardo Jorge (INSA) in Lisbon, Portugal and colleagues analysed viral genome sequences sampled from 15 infected individuals, to better understand the nature of the virus’s genetic mutations. Their aim was to establish how closely related these viruses were to each other, and to those responsible for previous outbreaks of monkeypox.
What did they find?
Their analysis, published in Nature Medicine, revealed that the viruses responsible for the current monkeypox outbreak may be related to ones responsible for causing a handful of human cases in the UK, Israel and Singapore during 2018 and 2019 – although the virus has changed significantly since then. These earlier cases (all linked to travel from Nigeria) themselves showed genetic similarities to viruses associated with a large monkeypox outbreak in Nigeria during 2017-18.
However, the current circulating viruses were genetically quite similar to one another. This suggests that the ongoing outbreak most likely arose from a single human case, with signs of ongoing evolution as the virus passes from person to person.
Have you read?
What does this mean?
Given these findings, it is likely that the current outbreak resulted from the virus being imported from a country where monkeypox is endemic, “potentially representing the continuous circulation and evolution of the virus that caused the 2017-2018 Nigeria outbreak”, the authors wrote.
“We cannot however exclude the hypothesis of a prolonged period of [undetected transmission] in humans or animals in a non-endemic country (e.g., after the reported 2018-2019 importations). Altogether, current data points for a scenario of more than one introduction from a single origin, with superspreader events (e.g., saunas used for sexual encounters) and travel abroad likely triggering the worldwide rapid dissemination.”
Notably, the current viruses contain far more genetic changes than one would expect, given previous estimates about how quickly this particular family of viruses evolves.
“Considering that this 2022 monkeypox virus is likely a descendant of the one in the 2017 Nigeria outbreak, one would expect no more than five to ten additional mutations [when compared with the 2018-2019 imported viruses] instead of the observed about 50 mutations,” said Gomes.
Possibly, the nature of some of these mutations has accelerated the virus’s evolution, although further research is needed to confirm this. For instance, a network of human enzymes known as the APOBEC3 system sometimes tries to disarm viruses by making changes to their genome – but in this case, those changes may not have had the desired effect, Gomes told Gavi.
For now, the implications of these changes for disease severity or transmissibility are unclear, but this should also be explored, the authors of the study said.