A rare but deadly brain infection is gaining ground in North America
Once confined to a few select regions, eastern equine encephalitis appears to be spreading to more US states, as climate change alters mosquito habitats.
- 9 July 2025
- 4 min read
- by Linda Geddes
It begins with a fever that escalates to confusion, drowsiness and seizures, before slipping its victims into a coma that one third will never wake from. For survivors, permanent brain damage is often the cost.
Though mercifully rare, eastern equine encephalitis (EEE), also known as Triple E or sleeping sickness, is appearing in an increasing number of US states, with researchers warning that climate change may be fuelling its spread.
Writing in the Journal of the American Medical Association (JAMA) this week, Dr J. Erin Staples and Dr Carolyn V. Gould at the US Centers for Disease Control and Prevention’s Division of Vector-Borne Diseases in Fort Collins, Colorado, outlined the growing threat posed by this mosquito-borne illness.
With no approved treatments or human vaccines available, surveillance among mosquitoes and animals is becoming increasingly important, along with measures to control mosquito populations and avoid bites in affected areas, they said.
Sleeping sickness
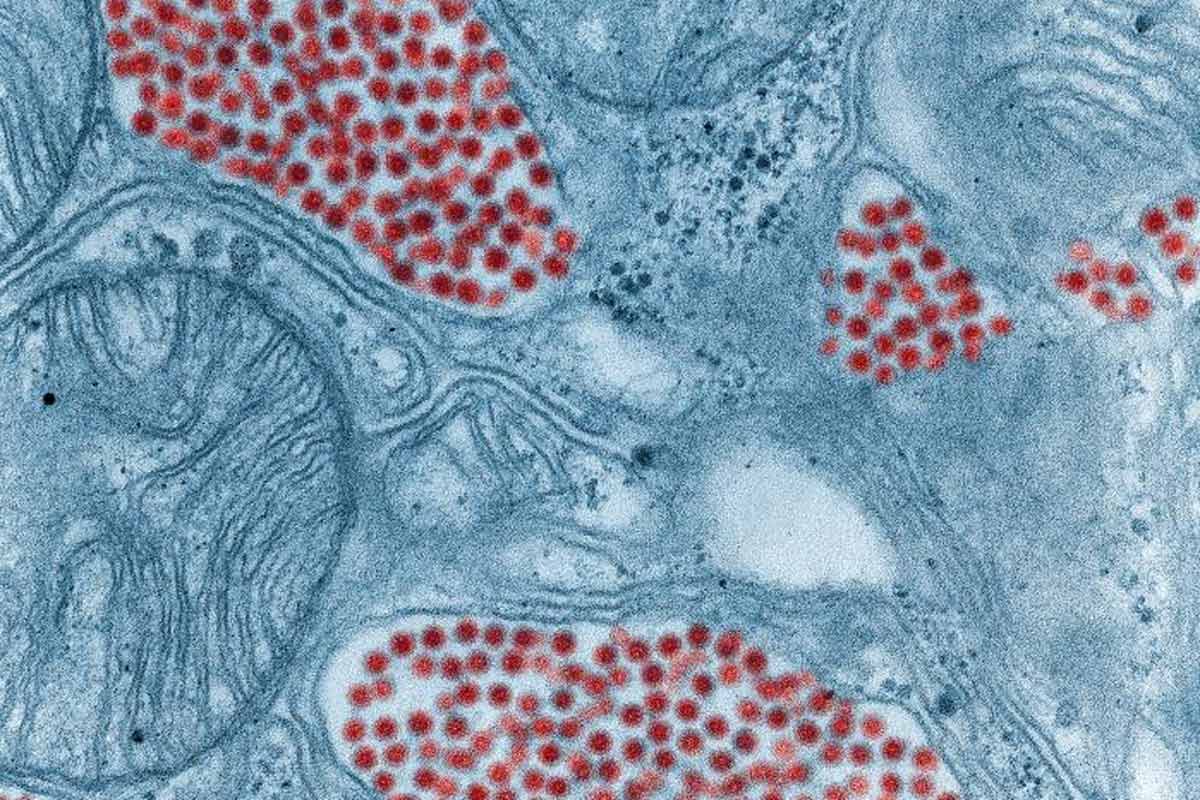
EEE virus is primarily transmitted by Culiseta melanura (black-tailed) mosquitoes that traditionally live in freshwater swamp forests in the Atlantic, Gulf Coast and Great Lakes regions of North America. These mosquitoes rarely bite humans, but they do feed on birds. These birds can then be bitten by a different mosquito species, who can pass the infection on to humans or horses they bite.
EEE was first identified in North American horses in 1831, with the first human cases reported during a large outbreak that resulted in 38 human and 248 horse infections in 1938.
Since then, sporadic infections have been reported almost every year, with around seven human cases reported annually in the US over the past two decades. It is likely that many more infections go unreported because the vast majority of cases are thought to be asymptomatic.
Although EEE is not yet a global health emergency, the recent uptick in cases has highlighted our lack of preparedness for unexpected infectious disease outbreaks.
If people do develop symptoms, the consequences can be extremely serious, as the virus can breach the protective barriers of the nervous system and trigger a type of brain swelling called encephalitis.
“Among the 193 EEE virus disease cases reported to the US Centers for Disease Control and Prevention from 2005 to 2024, 99% were neuroinvasive and 41% of these patients died,” Staples and Gould said.
For those who survive, more than half experience ongoing neurological problems, such as personality changes, difficulty speaking or understanding words, or paralysis, they added.
Viral spread
Although EEE virus disease is still rare, 38 cases were reported across seven midwest, north-east, and south-east US states during 2019. Cases have also been reported across a growing number of north-eastern states in recent years, with 17 of the 19 cases reported in 2024 occurring in the New England region, including Maine and Vermont.
People at highest risk of EEE virus infection are those living in or visiting endemic forested areas near swamps or marshes and those whose occupations or hobbies involve outdoor exposure.
While the reason for this recent increase in cases is uncertain, some researchers believe changing temperatures and rainfall patterns could be expanding the range of those mosquito species that transmit the virus to humans.
“Although EEE is not yet a global health emergency, the recent uptick in cases has highlighted our lack of preparedness for unexpected infectious disease outbreaks,” a group of biologists led by Ranjit Sah at Harvard Medical School argued in a recent article in Frontiers in Tropical Diseases.
“It is anticipated that the range of mosquitoes in the Americas, especially vectors of EEE virus, may be impacted by predicted climate change, which may modify disease risk and constitute a public health problem,” they said.
EEE isn’t the only mosquito-borne disease that could become more commonplace in North America because of climate change. The mosquitoes that spread malaria and dengue are expanding their geographic range, which could explain recent clusters of locally acquired malaria in Florida, Texas, Arkansas and Maryland, and dengue in California.
Cases of West Nile Virus, which is also transmitted by infected mosquitoes, are also increasing in US cities, as well as in northern parts of Europe.
Have you read?
Targeted surveillance
Although veterinary vaccines to protect horses against EEE are available, no human vaccines have been approved, though several candidates have shown promise in early-stage clinical trials. In the absence of a human vaccine, surveillance remains our best line of defence, Staples and Gould said.
Monitoring mosquitoes, birds, and unvaccinated animals could help to identify precisely where the virus is circulating, and guide public health responses such as targeted mosquito control and community education.
“People at highest risk of EEE virus infection are those living in or visiting endemic forested areas near swamps or marshes and those whose occupations or hobbies involve outdoor exposure,” Staples and Gould added.
“EEE virus surveillance in birds and mosquitoes can provide early warning indicators for human disease risk. Clinicians should alert public health authorities of suspected disease cases to enable rapid preventive messaging to reduce risk of further disease.”








