HIV among older South Africans in rural areas: big study shows there’s a problem that’s being neglected
A significant number of older adults in rural South Africa are HIV-positive. Awareness programmes and self-testing would reduce cases.
- 29 February 2024
- 5 min read
- by The Conversation
South Africa continues to have a high prevalence of HIV among all age groups. About 8.2 million people or 13.7% of the population live with HIV, one of the highest rates in the world.
The country also has one of the world’s most impressive antiretroviral therapy programmes. Over 5 million people living with HIV are currently on chronic treatment. Widespread access to antiretroviral therapies since 2008 has led to millions of people ageing with chronic HIV infection. Consequently, people with HIV are older on average than they were just a decade ago.
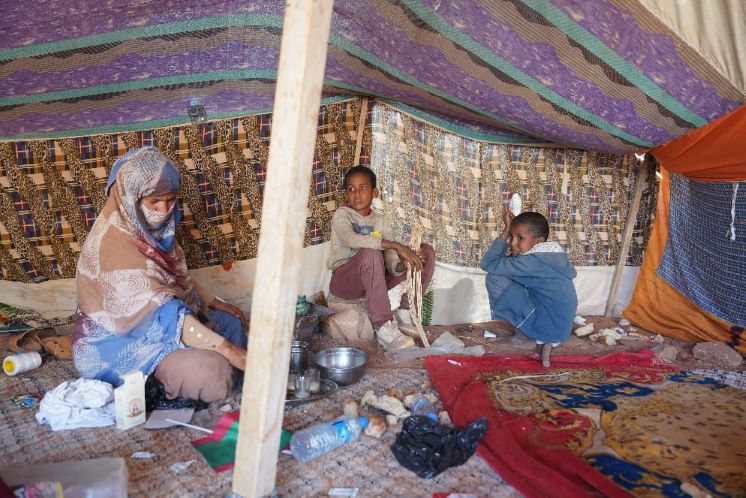
Most HIV prevention and treatment programmes and policies in South Africa remain focused on adolescents and young adults. A growing group of middle-aged and older adults with HIV, or at high risk, are being left behind.
To date, there has been little research about sexual behaviour, risk of HIV transmission, HIV stigma and HIV prevention for adults over 40 years old.
The Health and Aging in Africa: Longitudinal Studies in South Africa study – or Haalsa as it is commonly known – is an exception to this trend. It seeks to better understand both the risk of getting HIV and the health of ageing adults with HIV in South Africa.
This project, a collaboration between the University of the Witwatersrand and Harvard University, has followed a cohort of over 5,000 adults older than 40 in the Agincourt region in north-east South Africa for more than 10 years.
Throughout this decade of research, the team has been gaining a deeper understanding of this “greying” HIV epidemic. Numerous important insights about HIV in older populations have already been achieved. Here we present some of the findings.
Sexual activity is common
Research conducted in 2017 uncovered a high prevalence of HIV in this older population. Nearly 1 in 4 people over 40 years old were living with HIV.
The study found that 56% of respondents, across all HIV status categories, had had sexual activity in the past 24 months. Condom use was low among HIV-negative adults (15%), higher among HIV-positive adults who were unaware of their HIV status (27%), and dramatically higher among HIV-positive adults who were aware of their status (75%).
In another investigation in this cohort, the team found that over the period from 2010 to 2016 the incidence rate of HIV for women was double that of men.
Feeling the stigma
There are relatively few studies of HIV-related stigma among older adults, despite the increasing number of older adults living with HIV.
The majority of research excludes, or ignores, age as a variable. Understanding HIV-related stigma in older adults remains crucial and can inform interventions to support their mental health and overall well-being.
Our research suggests that social stigma poses a significant barrier to testing behaviour among older adults. A quarter of our respondents reported social stigma related to HIV infection.
Have you read?
This stigma was found to have important implications for HIV care: those experiencing high social stigma were less likely to engage in HIV testing and less likely to be linked to treatment.
A recent pilot study examined home-based HIV testing options for older adults and showed a preference for self-testing. More privacy may encourage more adults to establish their HIV status.
Treatment targets
Haalsa is uniquely positioned to understand how older adults with HIV are faring in terms of achieving HIV treatment targets, including viral suppression.
In 2014-2015, 63% of older adults with HIV in the study were taking antiretroviral therapy and 72% of those on therapy were virally suppressed. More recent updates have suggested that as of 2018-2019, many more older adults with HIV were virally suppressed.
To further highlight the critical importance of viral suppression for healthy ageing, the Haalsa team explored the impact of viral suppression on life expectancy in older adults.
Here, they found large gaps in life expectancy based on viral suppression status: a 45-year-old man without HIV could expect to live about another 27 years; a man with virally suppressed HIV could expect to live 24 years. One with unsuppressed HIV could expect to live 17 years.
Similarly, a woman aged 45 without HIV could expect to live another 33.2 years compared with 31.6 years longer for a woman with virally suppressed HIV. A woman with unsuppressed HIV could expect to live a further 26.4 years.
Looking to the future
Taken together, these new insights are critically important to inform the design of interventions and policies to ensure healthy ageing in South African society, and particularly among those with or at high risk of HIV.
Tailored strategies to prevent new HIV infections, awareness programmes and support to ensure that more people living with HIV in older age groups achieve and maintain viral suppression are urgently needed to reduce HIV risk in this and similar communities in sub-Saharan Africa.
Authors
Jen Manne-Goehler, Physician-scientist, Harvard T.H. Chan School of Public Health
Francesc Xavier Gomez-Olive Casas, Research Manager at MRC/Wits Agincourt Research Unit, University of the Witwatersrand
Julia Rohr, Research Scientist, Harvard University
Kathleen Kahn, Professor: Health and Population Division, School of Public Health, University of the Witwatersrand
Nomsa Mahlalela, Researcher, University of the Witwatersrand
Till Bärnighausen, Professor, University of Heidelberg

This article is republished from The Conversation under a Creative Commons license. Read the original article.
Disclosure statement
Jen Manne-Goehler receives funding from the US National Institutes of Health.
Julia Rohr receives funding from National Institute on Aging of the National Institutes of Health (NIH).
Till Bärnighausen for this work my institution has received a grant from the National Institutes of Health/National Institute of Aging (NIH/NIA), which is the HIV component NIH/NIA of the overarching NIH/NIA HAALSI Unrelated to this work, I also receive funding from a wide range of public science funders, including the NIH (other institutes), the German National Research Foundation , the European Union (within the Horizon science funding programme, the Alexander von Humboldt Foundation, the Volkswagen Foundation, the German Federal Ministry of Education and Research, the German Federal Ministry of the Environment, Wellcome (the British Medical Research Foundation), and the Else Kröner Fresenius Foundation.
Francesc Xavier Gomez-Olive Casas, Kathleen Kahn, and Nomsa Mahlalela do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
Partners
University of the Witwatersrand provides support as a hosting partner of The Conversation AFRICA.