Nearly a third of hospitalised COVID-19 patients show signs of organ damage
Study highlights the need to follow up COVID-19 patients after hospital discharge, especially if they have ongoing symptoms.
- 25 September 2023
- 4 min read
- by Linda Geddes

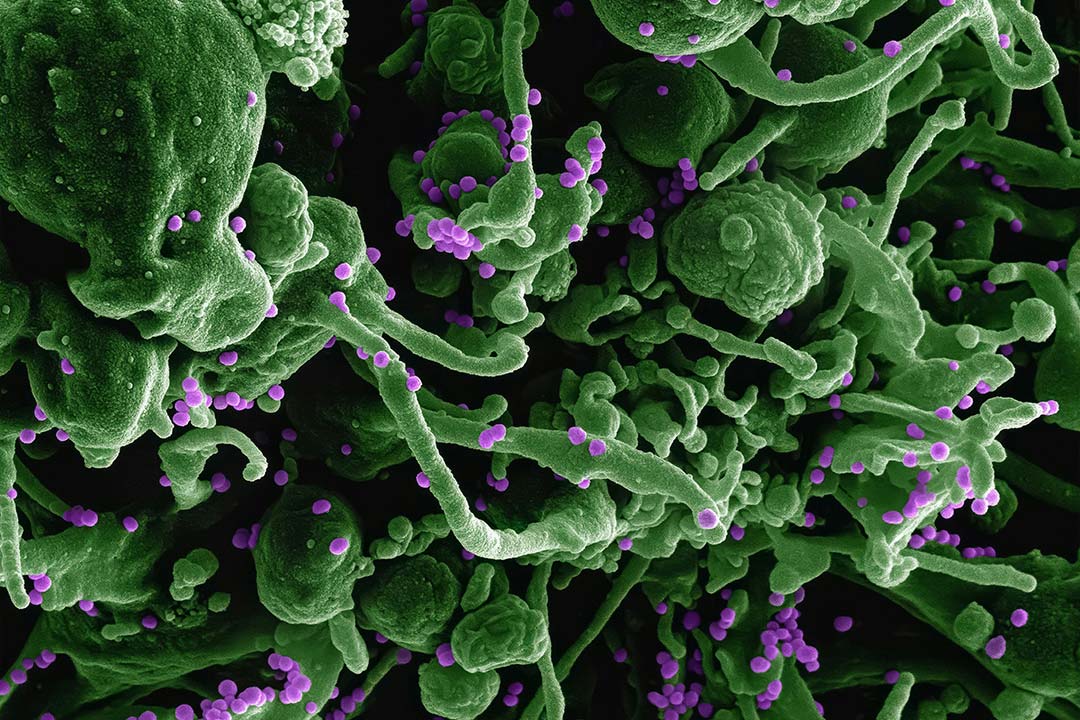
Brain and body scans of people who were hospitalised with COVID-19 suggest that longer-term organ damage may be relatively common – with nearly a third of patients displaying abnormalities in multiple organs five months after infection.
The study – the most comprehensive of its kind to date – also confirmed that such abnormalities were more common among patients who reported severely impaired physical and mental health after catching COVID-19.
"These results suggest that Long COVID is not explained by severe deficits concentrated in any one organ. Rather, the interaction of two or more abnormalities in organs might have an additive or multiplicative effect in creating physiological deficits that result in Long COVID symptoms."
– Prof Matthew R Baldwin, Columbia University Medical Centre
The findings underscore the importance of preventing infection and the need for comprehensive follow-up of hospitalised patients, with "meticulous attention to multi-system health – and an emphasis and focus on brain, lung and kidney health," said Betty Raman, Associate Professor of Cardiovascular Medicine at the University of Oxford, UK, who led the study. "It also suggests that we need to [identify ways to] reduce the multi-system damage that is caused by COVID-19," she said.
While previous studies have identified common yet mild abnormalities in the hearts or lungs of people who have recovered from COVID-19, only a few have investigated multiple organs within the same patient, and these predominantly focused on non-hospitalised patients.
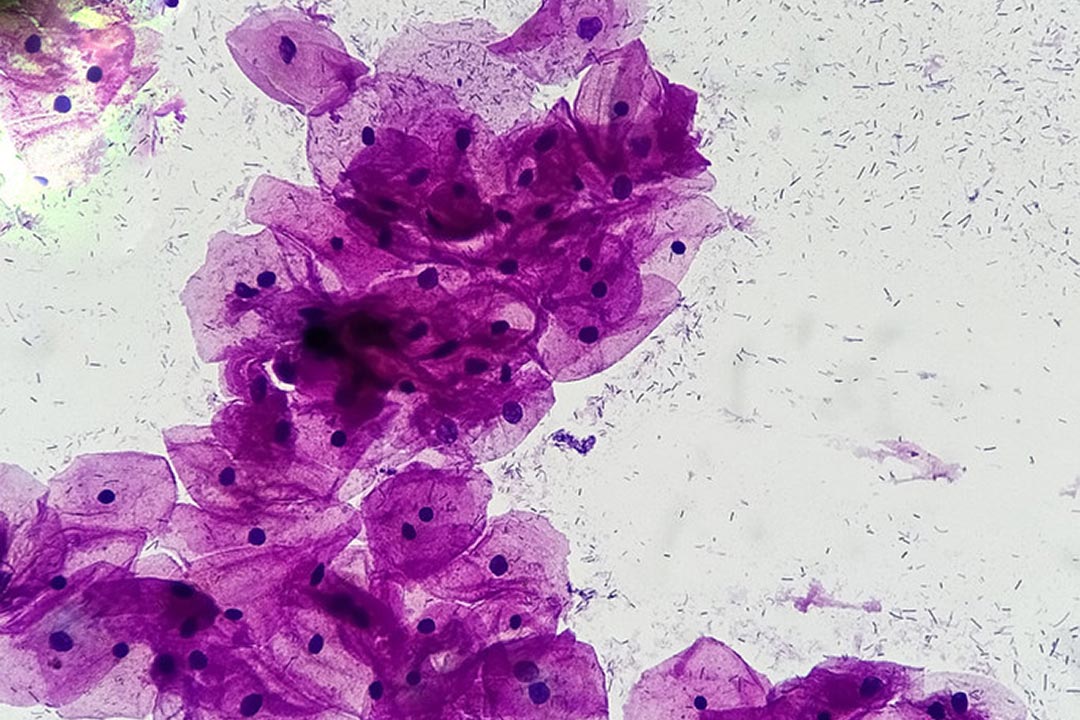
The C-MORE (Capturing the MultiORgan Effects of COVID-19) study is investigating the long-term effects of COVID-19 on hospitalised patients, through a combination of blood tests, questionnaires and magnetic resonance imaging (MRI) scans.
Have you read?
The latest results, published in The Lancet Respiratory Medicine, are an interim analysis of 259 patients who underwent blood tests and MRI scans covering the heart, brain, lungs, liver and kidneys an average of five months after discharge from hospital, plus 52 people who did not catch COVID-19.
Lung abnormalities were almost 14-fold higher, and brain and kidney abnormalities three- and two-fold higher among COVID-19 patients who had been discharged from hospital, compared to the control group.
While some organ-specific symptoms, such as cough or chest tightness, correlated with the abnormalities that were visible on the scans, not all symptoms did. However, people with more than two organs affected were four times more likely to report severe and very severe mental and physical impairment. Nearly one in three patients had evidence of multi-organ abnormalities on MRI.
"These results suggest that Long COVID is not explained by severe deficits concentrated in any one organ. Rather, the interaction of two or more abnormalities in organs might have an additive or multiplicative effect in creating physiological deficits that result in Long COVID symptoms," said Prof Matthew R Baldwin at Columbia University Medical Centre, New York. Studying these interactions could help to identify new therapeutic targets, he added.
Chris Brightling, a professor of respiratory medicine at the University of Leicester, UK, who was also involved in the research, said: "Although the numbers that are going into hospital and the severity of the disease have reduced as a consequence of vaccines and people having been exposed to COVID-19, there are a lot of people for whom these effects may have already occurred, and there is still a risk of people [being hospitalised] with severe infection."
While he stressed that only a minority of COVID-19 patients experience substantial ongoing symptoms. For them, "it is going to be really important to have this multidisciplinary care approach, and to be looking for underlying causes and better ways of diagnosing different types of Long COVID syndrome. Doing so will help us to identify what are the best tests to do in the clinic, and which treatments are likely to be most successful," he said.
Raman said the findings should also provide "some validation to patients – especially those who are severely crippled with symptoms – that perhaps there is something that we need to [physically investigate], to ensure they don't have organ [damage]."