Routine vaccinations during a pandemic – benefit or risk?
Some countries may stop their vaccination programs for a while to reduce the risk of spreading COVID-19. But which is better: fewer coronavirus infections or making sure children get all their usual vaccinations?
- 7 December 2020
- 9 min read
- by Science Journal for Kids and Teens

Authors: Kaja Abbas, Simon R Procter, Stefan Flasche and others
Associate Editors: Elitsa Panayotova and Madeleine Corcoran
Did you have your routine vaccinations as a kid? Vaccines help prevent millions of deaths each year. But now that the new coronavirus is here, some countries may stop their vaccination programs for a while. The idea is to reduce the risk of spreading the SARS-CoV-2 coronavirus, which causes the COVID-19 disease.
But which is better: fewer coronavirus infections or making sure children get all their usual vaccinations? To find out, we used a mathematical model. We worked out the risks and benefits if health systems in Africa continue with their vaccination programs as usual. We found that if African countries give vaccinations as usual, they will prevent many children from dying. The benefits are far greater than the risk of extra deaths due to COVID-19.
Introduction
The new coronavirus has caused many difficulties all over the world. Lots of people have become sick, and many have died. Many countries have taken measures to try to prevent the spread of SARS-CoV-2 coronavirus. A lot of us are in lockdown and some can't even go to the doctor unless it's urgent. But how far should these kinds of restrictions go?
For many years, we have defeated dangerous infectious diseases using vaccinations. (Unfortunately, as of November 2020 there is no licensed vaccine for COVID-19 yet as it's a new disease.) Since children are at high risk of falling sick from many infectious diseases, we usually receive vaccinations when we are children. Also, we are most likely to build up a good resistance to each disease in childhood. Vaccinations save lives and prevent the health complications that would come from catching the real diseases.
But what about during an epidemic? Going to the hospital or vaccination clinic poses many risks. Children or their carers could get infected with the SARS-CoV-2 coronavirus when they are in the clinic. They could then infect the entire household. Should we continue to give vaccines as usual? Or would everyone be better off staying at home? Which course of action will save the most lives? We wanted to find answers to these important questions.

A clinician gives a dose of pneumococcal vaccine at Basse Hospital in Gambia, Africa. Source: The London School of Hygiene & Tropical Medicine.
Methods
We looked at all 54 African countries. We used a mathematical model to work out the benefits and risks if they carry on with vaccinations as usual. In our model we made some assumptions:
- The measures against COVID-19 include social distancing
- If a vaccine against COVID-19 is not discovered, the virus will eventually infect around 60% of the population
- The risk from COVID-19 lasts for six months
To work out the benefits of continued vaccination...
We estimated how many children would die from the time of the missed vaccinations until age five, if there were no routine vaccinations for 6 months.
To make a better assessment, we considered two extreme scenarios:
- Worst scenario: The risk from these diseases will be high until the children reach 5 years of age. Herd immunity doesn't protect the children. There will be no catch-up vaccination programs after the COVID-19 epidemic.
- Better scenario: Herd immunity will protect the unvaccinated children from the diseases – except for measles. There will be catch-up vaccination programs afterward.
To work out the risks of continued vaccination...
We calculated the extra exposure to the SARS-CoV-2 coronavirus that giving the vaccines could cause. We worked out the extra risk to the child, their caregiver, and their household members. We took into account the average household size and age composition in each country. This helped us to estimate the extra deaths among household members of vaccinated children, especially among the elderly people who are more likely to die from COVID-19.
Results
Risks of continued vaccinations:
Visits to vaccination clinics could cause an extra 8300 deaths from COVID-19. Very few of these deaths would be among the children and other young members of the households. Most of them would be among the oldest adults.
In our 'worst' scenario, we found that giving vaccinations as usual will prevent around 700,000 deaths in children. Measles and pertussis would have caused most of these deaths.
For every extra death due to COVID-19, vaccination will have prevented 84 deaths in children under five. This means the benefit-risk ratio is 84 (Fig. 1). If we focus only on the vaccinated children, for every extra child that would die from COVID-19, 85,000 other children will have been saved from death due to vaccine-preventable diseases.
In our 'better' scenario, the benefit-risk ratio of a sustained vaccination program is 3. For every extra death due to COVID-19, vaccination will have prevented three deaths in children under five. If we focus only on the vaccinated children, for every child that would die from the extra exposure to the SARS-CoV-2 coronavirus in the clinic, 3000 more will have been saved by vaccination.
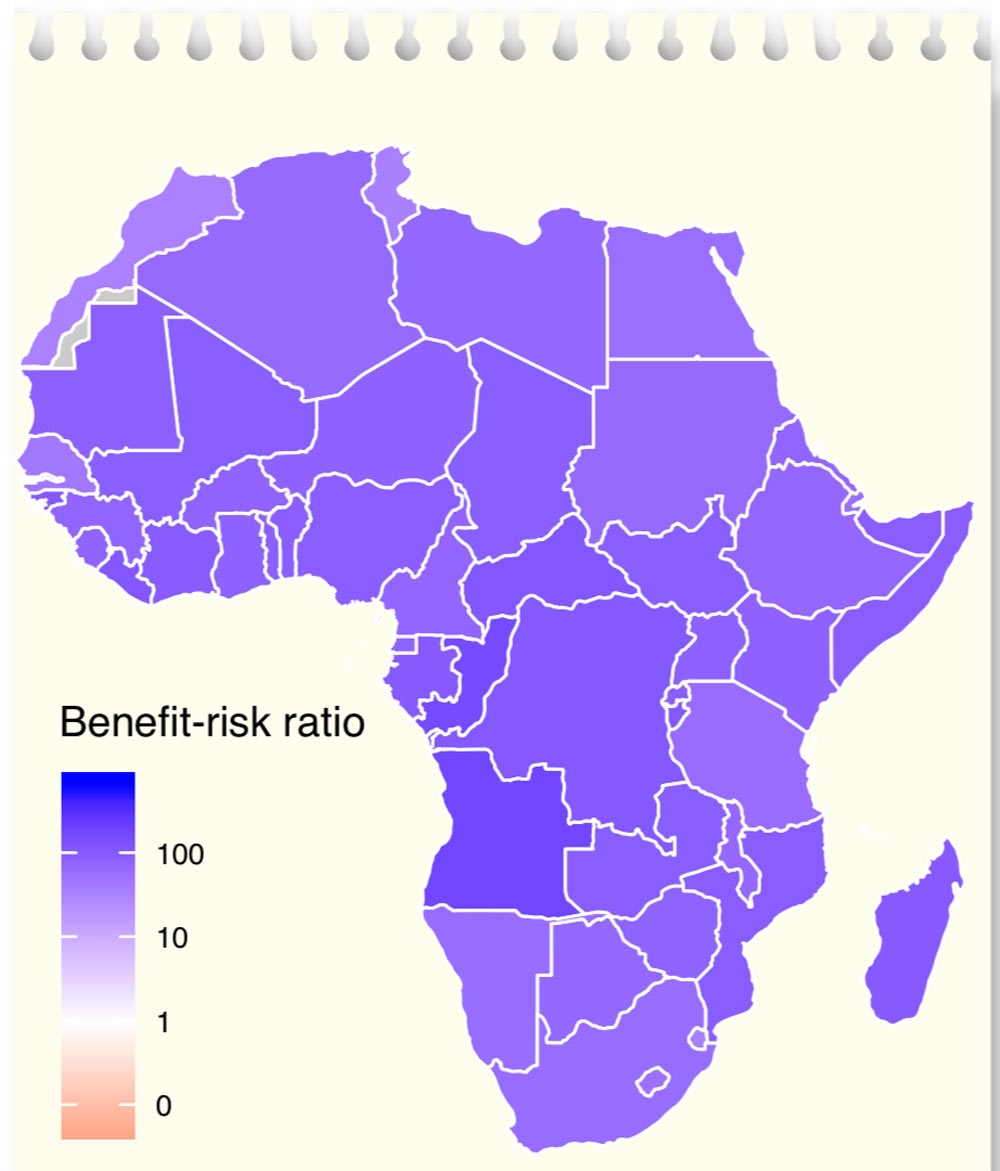
Figure 1:
Benefit–risk ratios if vaccinations for children continue as usual in Africa during the COVID-19 pandemic. This is under our ‘worst’ scenario – when the other diseases have a high impact. Grey = missing data.
Discussion
The benefits of carrying on with vaccinations as normal among children in Africa are far greater than the risk of extra deaths from COVID-19.
Many more lives will be saved by continuing with vaccination programs, despite COVID-19. This is true even if those other diseases have a lower impact (our ‘better’ scenario).
Furthermore, the extra exposure to the SARS-CoV-2 coronavirus in the vaccination clinic is mainly a risk to the older adults in the child’s household. Protecting the elderly is of great importance and may reduce these extra deaths.
Africa has one of the youngest populations in the world, which makes COVID-19 less severe there. On the other hand, there are risk factors in African countries which could make COVID-19 worse for people. For example, HIV, TB, and malnutrition can mean that people get sicker.
Since the benefits are far greater than the risks, we recommend that routine vaccinations should continue. At the same time, improved safety measures should be used to protect children, parents, and healthcare staff from the SARS-CoV-2 coronavirus. Safety measures in the vaccination clinics include patients keeping a distance of two meters apart, everyone wearing protective equipment (masks for patients and masks, gloves, and face shields for healthcare workers), and everyone washing their hands regularly.
Conclusion
When a lot of lives are on the line, it’s hard for health authorities to make decisions. This is where science can help. It may seem cold to assess lives as numbers, but it’s the best way to save as many people as possible – and keeping up with vaccination programs will do that.
The best way to help others right now is to keep a safe distance from each other. When you can’t keep your distance, you should wear a face mask. And remember to wash your hands regularly!
Check your understanding
1 How do routine vaccinations help prevent deaths?
2 Why do we consider going to the vaccination clinic a risk in terms of COVID-19?
3 In our research, we looked at benefit-risk ratios.
a) What does it mean if the ratio turns out to be less than 1?
b) What does it mean if the ratio turns out to be larger than 1?
4 How much social distancing do you and your family practice? Why?
5 What safety measures can protect the children, parents, and healthcare staff from coronavirus in the vaccination clinics?
Glossary of Key Terms
Assumption – something that we take as true in a mathematical model, based on current scientific understanding, when exact information or numbers aren’t available. Assumptions can help us find useful results with mathematics when there are some unknowns. For example, in our model we assume that for every person that contracts COVID-19, they will infect, on average, between 1.6 to 3.6 other people.
Benefit-risk ratio – the ratio of the benefits of an action to its risk. For example, if a drug is more likely to cure a certain patient than harm them, the benefit-risk ratio is above 1 – there is more benefit than risk.
Coronaviruses – a group of closely related viruses that usually cause respiratory infections in humans. Sometimes they cause symptoms and sometimes they do not. Symptoms can be mild to severe and can include pneumonia, coma, and death. Common coronaviruses cause mild to moderate illness like the common cold. Other coronaviruses are SARS-CoV (severe acute respiratory syndrome coronavirus), MERS-CoV (Middle East respiratory syndrome coronavirus), and SARS-CoV-2 (the virus causing the current pandemic) and can cause severe illness.
COVID-19 – coronavirus disease 2019, a disease caused by the SARS-CoV-2 virus. Symptoms may include fever and dry cough in milder cases and difficulty breathing in more severe cases.
Epidemic – A sudden increase in the number of disease cases in a particular population.
Herd immunity – As more and more people in a population become immune either through recovery from infection or through vaccination, the chance that a disease can spread decreases. Everyone benefits from extra protection thanks to people who are already immune. When enough people are immune, they act as a shield for vulnerable people, and so the opportunity for the disease to spread becomes so low that we say this population has herd immunity.
Mathematical model – a set of mathematical equations that attempts to simulate a system (for example an epidemic) and so to predict how the system would behave in the real world.
SARS-CoV-2 coronavirus – the name of the virus that causes COVID-19 in humans.
Social distancing – deliberately decreasing contact between people to avoid the spreading of illness.
Vaccination – a person receives parts of a virus or bacterium or weakened versions of the pathogen and develops antibodies against them without getting sick: the immune system now knows how to fight this type of infection. For instance, most children receive Measles, Mumps, and Rubella vaccine (MMR) to prevent them from getting these diseases in the future.
References
- Kaja Abbas, Simon R Procter, Kevin van Zandvoort, Andrew Clark, Sebastian Funk, Tewodaj Mengistu, Dan Hogan, Emily Dansereau, Mark Jit, Stefan Flasche, LSHTM CMMID COVID-19 Working Group. (2020). Routine childhood immunisation during the COVID-19 pandemic in Africa: a benefit-risk analysis of health benefits versus excess risk of SARS-CoV-2 infection. The Lancet Global Health.
https://doi.org/10.1016/S2214-109X(20)30308-9 - Gavi, the Vaccine Alliance: Should Countries Stop Vaccinations to Halt the Spread of COVID-19?
- The Guardian: Herd Immunity Visualisation
https://www.theguardian.com/society/ng-interactive/2015/feb/05/-sp-watch-how-measles-outbreak-spreads-when-kids-get-vaccinated - John Hopkins Medicine: Coronavirus, Social and Physical Distancing and Self-Quarantine
https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/coronavirus-social-distancing- and-self-quarantine










