Sex and the cervix: the hidden toll of treatment for cervical pre-cancer
The removal of abnormal cells from the cervix undoubtably saves lives, but more research is needed to understand the physical and emotional consequences.
- 11 October 2024
- 11 min read
- by Linda Geddes

Five and a half years ago, I received news that my routine smear test had produced an abnormal result, and that I’d tested positive for human papillomavirus (HPV). My initial instinct was to shrug; I’d experienced scares like this before when my cervical sample had been contaminated with blood. But I agreed to further tests, including a colposcopy – where a specialist inspected my cervix with a magnifying lens and removed a small chunk of tissue to see if it contained precancerous or cancerous cells.
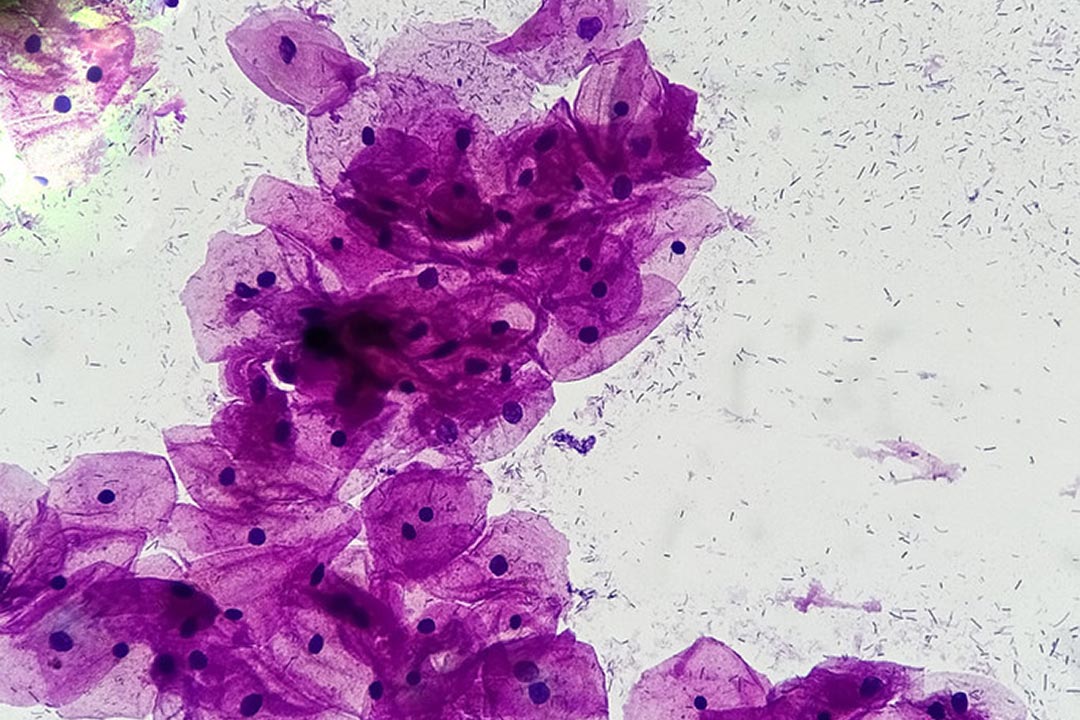
The good news was that I didn't have cancer – yet. The bad news was that I had cervical intraepithelial neoplasia 3 (CIN3), meaning that the full depth of the outer surface of my cervix contained abnormal cells. Although CIN isn’t cancer, if the abnormal cells aren’t removed, then over time they may develop into cervical cancer.
The recommended treatment was a procedure called LLETZ (large loop excision of the transformation zone), in which a thin wire loop with an electrical current is used to remove the affected area of the cervix.
Although health care professionals generally counsel women about common side-effects and the potential impact on future pregnancies, these conversations don’t usually extend to sexual functioning.
I was asked if I planned to have any more children, as the procedure slightly increases the risk of late miscarriage or premature birth in subsequent pregnancies. I was also informed about a rare complication in which the passage into the uterus can become narrowed or blocked, as well as common side-effects such as short-term pain and bleeding.
What no one raised was the longer-term pain and altered sensations I might experience because of treatment, and the impact this might have on my sex life.
Cancer prevention
The HPV vaccine is a highly effective way of preventing such abnormalities from developing in the first place, but not every woman can be vaccinated, and there are millions of older women who are already infected with HPV for whom the vaccine isn’t currently recommended.
For them, LLETZ and similar procedures that remove abnormal cells are a highly effective means of nipping cervical cancer in the bud. In more than 90% of cases, no further treatment is needed once the cells are removed, and women can carry on with their everyday lives.
Yet, this life-saving procedure isn’t entirely without risk, and although health care professionals generally counsel women about common side-effects and the potential impact on future pregnancies, these conversations don’t usually extend to sexual functioning.
Some believe that they should. Increasingly, evidence suggests that the cervix may not be merely an inert cylinder sitting at the top of the vagina, but a sensitive organ that plays an important role in some women’s pleasure.
Though removing part of it may be necessary to prevent cancer, a subgroup of women may experience ongoing pain, or a reduction in vaginal or clitoral sensation as a result. Scientists who study sexual function are calling for further research to quantify the scale of the problem, and what to do about it. Work is also underway to identify biomarkers that could eventually predict which women with abnormal cervical cells are the most likely to develop cancer, and which may get better without needing treatment.
“One of the patients we worked with said that they felt violated during sexual intercourse, because they couldn’t feel anything.”
- Dr Olivia Giovannetti, an assistant professor at Queen’s University in Kingston, Canada
Cervical cancer is the third most common cancer in women, and the HPV virus that causes it is extremely prevalent, with around four fifths of men and women having experienced at least one HPV infection by the age of 45. In 90% of cases, the body naturally clears the infection, but if the virus continues to linger in the cells lining the cervix, it begins to disrupt their function, and they start growing abnormally.
Cervical intraepithelial neoplasia (CIN) (also known as cervical dysplasia) is the term used to describe these changes, and is what health professionals are looking for when they do a smear test. It is graded on a scale of 1–3. CIN 1 means one third of the thickness of the outer surface of the cervix is affected by abnormal cells; CIN2 means two thirds of the thickness is affected; while CIN3 means the full thickness is affected.
Weighing the risks
CIN doesn’t cause any symptoms, and can only be detected through cervical screening, which is why this is so important for cervical cancer prevention. Yet not everyone with CIN will develop cancer, and in some, the abnormal cells will go back to normal by themselves. This is most likely if you have CIN1, but up to 47% of people with CIN3 will also get better without treatment. The problem is that up to a further 40% of them will develop cervical cancer if left untreated, and it is currently impossible to predict which outcome will apply to an individual patient.
Also, while watchful waiting may be an option for people with lower-grade CIN in high-income countries, this may not be an option in those where resources for screening are limited, or there’s a higher baseline risk of cervical cancer progression, e.g. due to a high prevalence of HIV or high-risk HPV types.
“Because the cervix is a relatively inaccessible body part, it is not something that you can monitor for yourself, e.g. to see if it starts changing colour, so you are reliant on regular internal examinations and laboratory tests” says Dr Olivia Giovannetti, an assistant professor at Queen’s University in Kingston, Canada, who studies the anatomy of the cervix and other female pelvic tissues. “For CIN3, the risk of progression is considered so high, that treatment is almost always recommended.”
Informed consent
Millions of women around the world are treated for CIN each year – usually at an outpatient clinic, using local anaesthetic – and most recover without incident. However, according to research by UK charity, Jo’s Cervical Cancer Trust, many patients do not feel prepared for what happens to them during and after treatment. Of the 1,622 people they interviewed who had undergone treatment, 20% reported not having been told about any potential side-effects, and only 9% had potential impacts on their sex life explained to them.
“They acted like it was a wart removal. Not the fact that they’re removing the end of your cervix. It was just sort of a, this is no big deal, and it’s like, actually, this is a big deal. And so why are we not having a little more education around this?”
- A patient interviewed after LEEP/LLETZ treatment
Although it sounds trivial now, I remember my biggest concern before undergoing treatment was not being allowed to go swimming for a month afterwards, when it was the middle of summer, and I had just acquired membership of the local swimming lake.
Large numbers of those interviewed experienced known and common side-effects following treatment, including bleeding or spotting for up to six weeks (86%); infection (20%); and changes to vaginal discharge (25%).
The research also found that the psychological impact of diagnosis and treatment was profound, with more than three quarters experiencing anxiety and/or fears about cancer, and 24% experiencing depression. Many hadn’t received any support to help them cope with the emotional impact of what was happening to them.
Sexual problems
Also, like me, about a third of respondents reported experiencing pain during or after sex, and, although in many cases this lasted for less than three months, around half of these women reported longer-term pain, with 5% still experiencing it after five or more years.
Giovannetti has also conducted in-depth interviews with 60 patients who experienced negative outcomes after LLETZ or a related procedure called LEEP (loop electrosurgical excision procedure). Many described similar experiences of pain and numbness; altered lubrication or vaginal discharge; a drastic loss in arousal, desire, and interest in sex; and a muted experience of, or ability to reach orgasm.
“One of the patients we worked with said that they felt violated during sexual intercourse, because they couldn’t feel anything,” Giovannetti says.
“There’s also the emotional discomfort that inherently comes with the other symptoms. Some patients describe it as like a car that won't start.”
She also interviewed 18 North American and Canadian providers of LLETZ and LEEP, to better understand their perspectives. A prevalent attitude was that any symptoms of sexual dysfunction were likely to be psychological rather than physical, and some struggled to imagine how the procedure might cause sexual dysfunction, as it doesn’t remove tissues traditionally associated with sexual responses, such as the clitoris.
However, a minority of providers were receptive to this possibility, and keen to study it and address it with patients.
I wish I’d had access to the HPV vaccine when I was a teenager, and when my daughter was recently offered it, I immediately explained the importance of it and, with her agreement, signed the consent form.
Historic attitudes
Part of the problem may lie with outdated assumptions about what the cervix can and can’t feel. For instance, the “Kinsey Report”, a landmark study of human sexuality published in 1953, stated that “the surface of the cervix is the most completely insensitive part of the female genital anatomy”.
Dr Barry Komisaruk, a Distinguished Professor of Psychology at Rutgers University in New Jersey, US, who studies the neural basis of sexual responses, believes this statement has led health care providers to erroneously conclude that the cervix cannot feel, and can be cut or removed without consequence.
Yet, as anyone who has undergone a smear test or had an IUD inserted will attest, the cervix definitely has feelings.
Also, when Komisaruk and his colleagues put women into a brain scanner and asked them to stimulate their cervix, they found that the same parts of the brain lit up as when they stimulated their vagina or clitoris. They also reported being able to distinguish between different regions of the cervix. Anecdotally, it is also clear that the cervix plays a role in sexual functioning and pleasure for some women, and nerves in the cervix are likely to play a role in those sensations, says Giovannetti. “When they are removed, that could relate to the symptoms of pain or numbness that some patients experience.”
It is also possible that inflammation triggered by the procedure could affect nearby muscles, nerves and blood vessels, leading to altered arousal and sexual responses - but this is an understudied area of research and more work needs to be done, she adds.
Important procedure
Many of the patients she interviewed reported feeling that they hadn’t been adequately counselled about the procedure in advance, with discussions largely focusing on how LLETZ or LEEP was the “best option” for them.
As one patient put it: “They acted like it was a wart removal. Not the fact that they’re removing the end of your cervix. It was just sort of a, this is no big deal, and it’s like, actually, this is a big deal. And so why are we not having a little more education around this?”
Even so, no-one said they wouldn’t have elected to have the procedure. “They all valued the clinical outcome of removing harmful cervical dysplasia,” says Giovannetti. “Yet, they felt like their autonomy was stripped from them with respect to making medical decisions and that they were left alone navigating the negative effects of the procedure.”
Dr Linda Eckert, a professor of obstetrics and gynaecology and adjunct professor of global health at The University of Washington in Seattle, US, notes that the study only interviewed individuals who had self-identified with problems, which makes it hard to know how generalisable these findings are. She also stressed that the community of gynaecologists she works with care deeply about women’s sexual function.
However, she agreed that further research would be helpful, as would better counselling for those undergoing treatment: “So much of women’s health, especially sexual function, has a dearth of research [associated with it],” Eckert says.
“I am also glad that people appreciated treatment. As a person who has told too many people that they have cervical cancer, my bias is that LEEP is an important tool to prevent it.”
Giovannetti also emphasised the importance of LLETZ/LEEP for cancer prevention: “One hundred percent, the priority should be medical care to prevent cancers forming. My issue is that the procedure has never once been reviewed or updated since its inception. It has never been improved, in comparison to prostatectomy [to treat prostate cancer], where surgery has been reviewed and updated countless times, because there was the possibility of nerve damage to the prostate.”
She believes that an immediate improvement would be for health care providers to routinely start assessing sexual function in women and initiating conversations about it, so that women feel comfortable discussing any issues that they might be experiencing.
Improved screening
A further improvement would be the development of tools to better predict which women with CIN2 or 3 are most likely to develop cervical cancer, and which might be spared surgery. Increasingly, it looks as though patients infected with HPV types 16 and 18, which HPV vaccines protect against, may be at greatest risk, but “currently a biopsy of the cervix can be the best way to know who to worry about, and unfortunately, biopsies of the cervix can cause pain,” Eckert says.
Other biomarkers are being investigated, including two proteins called HPV E4 and p16ink, which could indicate the presence of HPV, and the stage of such infections.
Have you read?
“Previous studies have suggested that p16 negative/E4 positive CIN2 likely resembles CIN1, and so, will likely disappear without treatment. In contrast p16 positive/E4 negative cases may be CIN3-like lesions with higher risk of disease progression,” says Dr Anne Hammer, clinical professor of gynaecology at Aarhus University in Denmark, who is studying them.
These and other markers could eventually be used to help strengthen a diagnosis of CIN2 or 3 and help guide treatment options. “There is nothing wrong with active surveillance or excisional treatment, but women need better information on potential risk with both approaches to make an informed choice regarding treatment,” Hammer says.
As for me, my cervical pain has gradually subsided, but I still feel as though my vagina and cervix are wired slightly differently to the way they were before. I don’t regret having the procedure, and follow-up tests have revealed that I am now, mercifully, HPV-free. But I wish I’d had access to the HPV vaccine when I was a teenager, and when my daughter was recently offered it, I immediately explained the importance of it and, with her agreement, signed the consent form.
Prevention is better than treatment. But there are still several generations of women for whom screening and early treatment remains the only sensible option. We need to ensure that such treatments not only save lives but maintain the quality of people’s lives.