Why drug resistance is becoming one of our biggest global health security blind-spots
The growth of bacteria that show drug resistance means outbreaks of previously treatable infections are becoming a major global health security problem.
- 29 January 2024
- 5 min read
- by World Economic Forum

A recent wave of increased hospitalizations for respiratory infections in Northern China is the result of Mycoplasma pneumoniae, a bacterial infection that is usually mild and affects children and young adults causing respiratory symptoms or, in some cases, mild pneumonia.
But this shouldn't come as a surprise. Not just because a surge of respiratory infections had been anticipated in China following the relaxing of strict COVID-19-related restrictions but also because previous levels of drug resistance to M. pneumonia, as high as 90%, have been reported in Beijing.
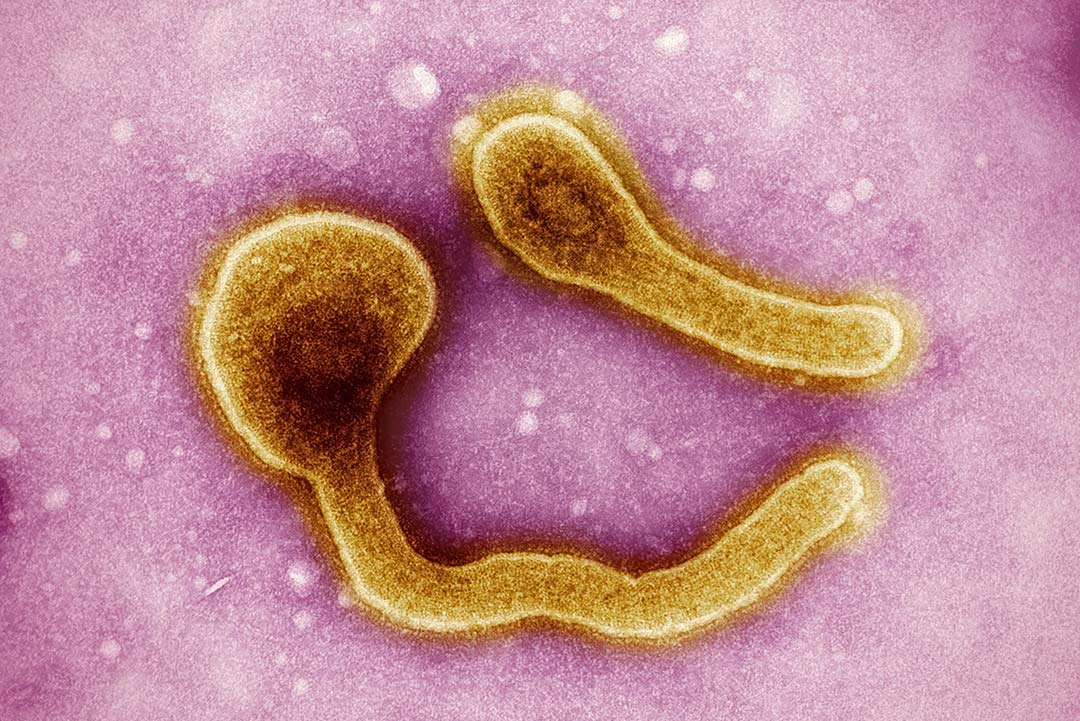
The fact is, given the rise and spread of drug-resistant bacteria, outbreaks of previously treatable infections are increasingly becoming one of our biggest global health security blind spots.
In the case of M. pneumoniae, outbreaks have since been reported in Denmark, France, Hong Kong, Indonesia and most recently in the US. In most cases, infection is mild and more serious cases can be treated with a class of antibiotics called macrolides. So, the sudden spike in children being hospitalized has been attributed possibly to increases in resistance to these drugs.
Luckily, there are other antibiotics that remain effective against this particular bacterium, but that is not always the case. With a growing number of other infections, there is increasing resistance to even the last remaining effective antibiotics. And, until the world starts to wake up to the scale of this problem, that is a trend that is set to continue.
Antimicrobial resistance (AMR) is already one of the biggest global killers, with nearly 5 million deaths a year. Yet, few people know what it is, let alone the threat it poses to them. One reason for this is its insidious nature. AMR likely won't hit us hard and fast like a pandemic; instead we'll see a steady rise in cases of treatable infections becoming once again untreatable, with even minor infections or medical procedures becoming life-threatening.
In time, the 23-year global increase in life expectancy we have experienced thanks to antibiotics could be steadily reversed. Given that all this could be prevented, perhaps one of the things that makes drug resistance now one of our greatest global health security threats is the very fact that too few people view it as one.
United Nations High-Level Meeting on AMR
In the run-up to the 2024 United Nations High-Level Meeting on AMR, we have an opportunity to change that and, in doing so, change course. Ostensibly, this will be a chance to bring the international community together to set global targets and practical steps towards addressing this escalating global health crisis.
At the same time, the hope is that Italy will continue to carry the torch in making AMR a global priority as it takes over the G7 Presidency from Japan. But a step change is also needed to shift the widespread perception that drug resistance is rare and only affects older and vulnerable people in hospitals and the belief that all it will take to solve this is the discovery of new drugs. Until that changes, we risk sleepwalking into the next global health crisis.
Part of the problem is that AMR is so drastically misunderstood and it's easy to see why. On the one hand, the common belief is that overuse of antibiotics is one of the main causes of drug resistance, as is the case with macrolides and M. pneumoniae.
Have you read?
Yet, while it is true that the consumption of antibiotics has significantly increased, by as much as 46% between 2000 and 2020, and that this has helped to drive drug resistance, it is also true that shortages are a major factor.
In many parts of the world, particularly lower-income countries, limited access to the most effective drugs is also fuelling AMR, either by allowing infections to continue to circulate or by leaving clinicians little choice but to use less appropriate antibiotics, which can accelerate the emergence of drug-resistant strains.
Global solutions are required
Clearly, global solutions are needed to address this public health failure; and, when it comes to innovation, we need to develop not just new antibiotics, but those that protect against priority pathogens, multidrug-resistant bacteria that pose the greatest public health threat.
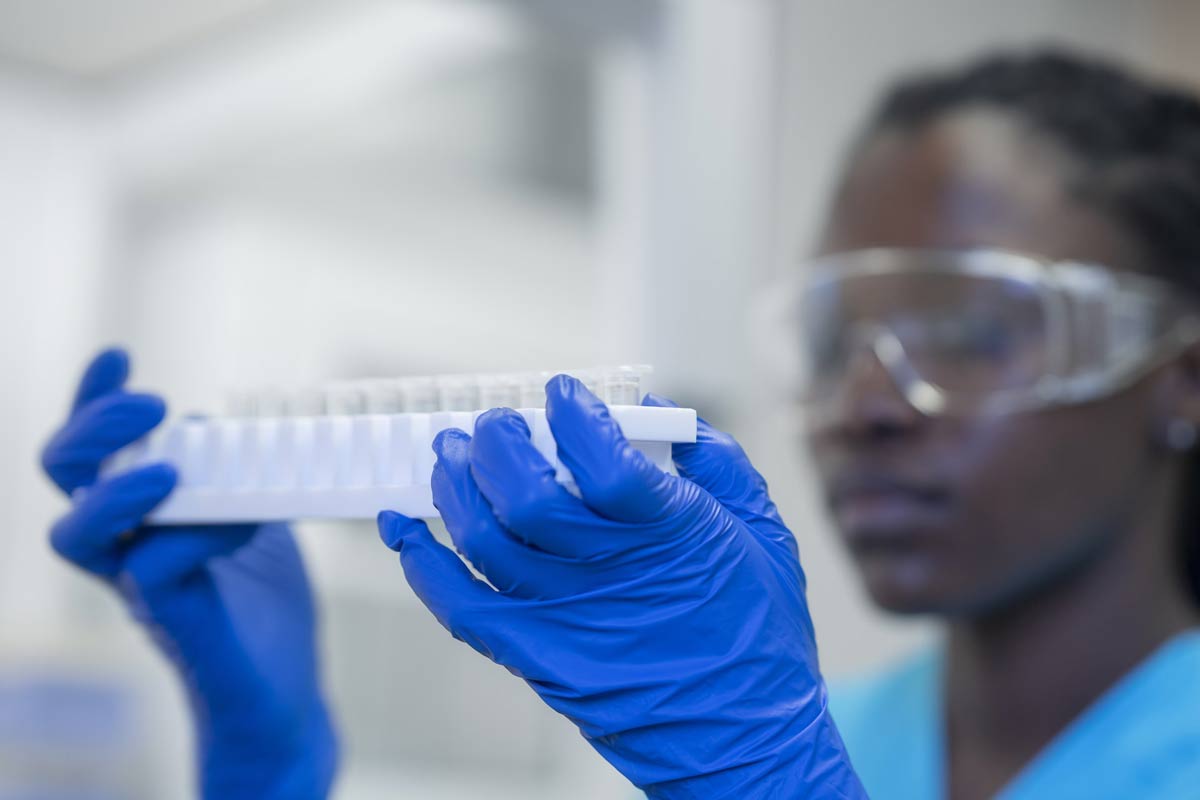
Also, crucially, we don't just need scientific solutions but also ones that people all over the world can get access to. That is precisely what organizations like mine, the Global Antibiotic Research & Development Partnership, are working on, with the aim of developing five new antibiotic treatments by 2025.
But given the worrying spike in cases of M. pneumoniae that we are now seeing beyond China, in countries which historically have had much lower levels of drug resistance, it is also clear that we need to make better use of the antibiotics we currently have.
That is unlikely to happen on the scale needed until there is greater global awareness of AMR. That means we need a radical shift in the way the world views AMR, recognizing it as a global crisis to begin with and a better understanding of the solutions needed. AMR is a slow burner. It currently kills more people than HIV/AIDS and malaria combined. If we wait until it reaches the point where it is killing more people than cancer, then effectively we have lost the fight.
Written by
Manica Balasegaram, Executive Director, Global Antibiotic R&D Partnership (GARDP)
Website
This article was originally published by the World Economic Forum on 24 January 2024.