Different types of immunity and why they matter to COVID-19
Antibodies are one route to immunity against disease, but T cells and innate immunity also play a crucial role in protecting us. So, how could these different types of immunity be mobilised against COVID-19
- 4 September 2020
- 5 min read
- by Linda Geddes

What is immunity?
Immunity is the ability to resist a specific infectious disease, meaning you can be exposed to the pathogen that causes it without becoming infected or falling seriously ill. It develops when the cells of your immune system encounter a harmful pathogen - such as a virus or bacterium - mount an immune response, and successfully fight it off. This can happen through infection with the actual disease (natural immunity), or through the introduction of a killed or weakened form of the disease-causing pathogen, or fragment of it, in the case of immunisation (vaccine-induced immunity). This immunity persists because even after the pathogen is eliminated from your body, specialised ‘memory cells’ linger, ready to spring into action and launch an enhanced response against that pathogen if you encounter it again.
Immunity is the ability to resist a specific infectious disease, meaning you can be exposed to the pathogen that causes it without becoming infected or falling seriously ill.
There are two broad types of immune response:
Innate responses kick in from the moment of infection and are the same for all potential invaders. They include physical barriers, such as the skin, as well as the activities of immune cells, such as macrophages and natural killer cells, which work to contain invaders while a more targeted ‘adaptive’ immune response develops, and alert other immune cells to their presence. In some cases, a strong innate response is enough to contain and eliminate an invading pathogen, such as a virus, before these adaptive responses kick in.
Adaptive responses target specific pathogens or foreign substances and can take several days to develop. They involve two types of cells:
- immune B cells, which help to hunt down invaders circulating in the bloodstream by producing antibodies - proteins which can bind to e.g. viral particles and either neutralise or mark them for destruction by other immune cells.
- T cells, which seek out and destroy cells that have been infected by the invading pathogen by recognising tell-tale proteins on their surface. T cells also support B cells, helping to control the antibody response.
Have you read?
How do I know if I’ve developed immunity to a virus like SARS-CoV-2?
Detecting antibodies in the blood is the most straightforward method. It implies some level of immunity, although levels of antibodies in people who have recovered from COVID-19 can tend to dwindle over time, raising concerns about how long immunity to SARS-CoV-2 lasts for. There are also concerns about the validity of some antibody tests and how much they can actually tell us, since a positive test result is no guarantee of immunity.
Even when antibody levels have dropped, or never developed at all, T cells can offer immunity. These can remain in circulation once the infection is cleared, helping maintain immunity to pathogens we have encountered before. One recent study of 36 people recovering from COVID-19 found T cells that recognise SARS-CoV-2 in all of them. Detecting T cells is a more complex process than testing for antibodies, so we shouldn’t expect a T cell test to be widely available anytime soon. However, there are hints that this kind of immunity may be longer-lasting. A recent study involving 23 patients who recovered from severe acute respiratory syndrome (SARS) in 2003, found that they still had robust T cell responses to the coronavirus 17 years later.
How could we boost our immunity against SARS CoV-2?
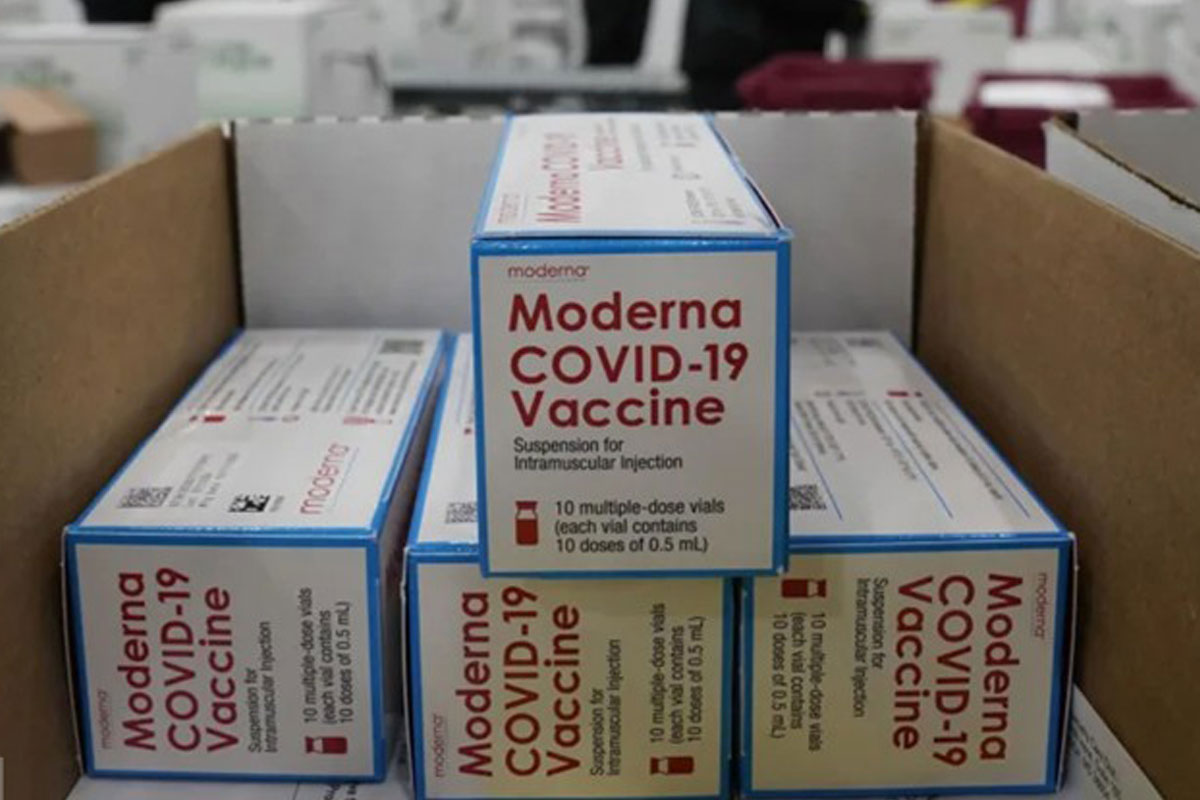
Vaccination is an obvious strategy. Most vaccines aim to stimulate the development of antibody-producing B cells and the helper T cells which support antibody production, but they can also promote development of killer T cells which target infected cells. Encouragingly, some of the COVID-19 vaccines which have already entered human trials appear to stimulate both B and T cell activity, including the RNA-based vaccine being developed by Pfizer.
Another strategy undergoing human trials is the injection of plasma from people who have already recovered from COVID-19. Plasma is the yellow-ish liquid portion of blood which remains once all the red and white blood cells, and platelets have been taken out. In the aftermath of infection, it is often rich in antibodies against the pathogen which caused it. Careful screening can help make sure the plasma is free of other infectious germs. By transfusing plasma from people who have had COVID-19, the hope is that their antibodies will hasten the recovery of those who are currently suffering from the disease.
It may also be possible to bolster innate immune responses to SARS-CoV-2. Emerging research suggests that one way in which the virus evades our immune systems is by disabling small but powerful proteins called interferons, which are unleashed by cells of the innate immune system during the early stages of infection. Interferons provoke an intense and local response when a virus invades a cell, unleashing various other proteins which inhibit viral replication and the invasion of neighbouring cells. They also help to recruit and activate other immune cells. Trials of interferons - which are already used to treat various cancers, hepatitis, and multiple sclerosis - in patients with COVID-19 are ongoing.