It’s 70 years since scientists first identified the Zika virus. Since then outbreaks have been recorded on three continents, with the largest epidemic to date beginning in Brazil in 2014. In early 2016 this outbreak, which rapidly spread across the Americas and into Asia, was declared a global public health emergency.
Despite this, there is no Zika vaccine. This reflects a trend in emerging infectious diseases: as the scale of such outbreaks is unpredictable, developing vaccines against them is risky for pharmaceutical companies as there is no guarantee of a return on their investment. As a result, vital vaccines for destructive diseases are often made too late, if at all. This problem only stands to get more serious as the risk of major disease outbreaks is amplified by climate change, mass migration and urbanisation.
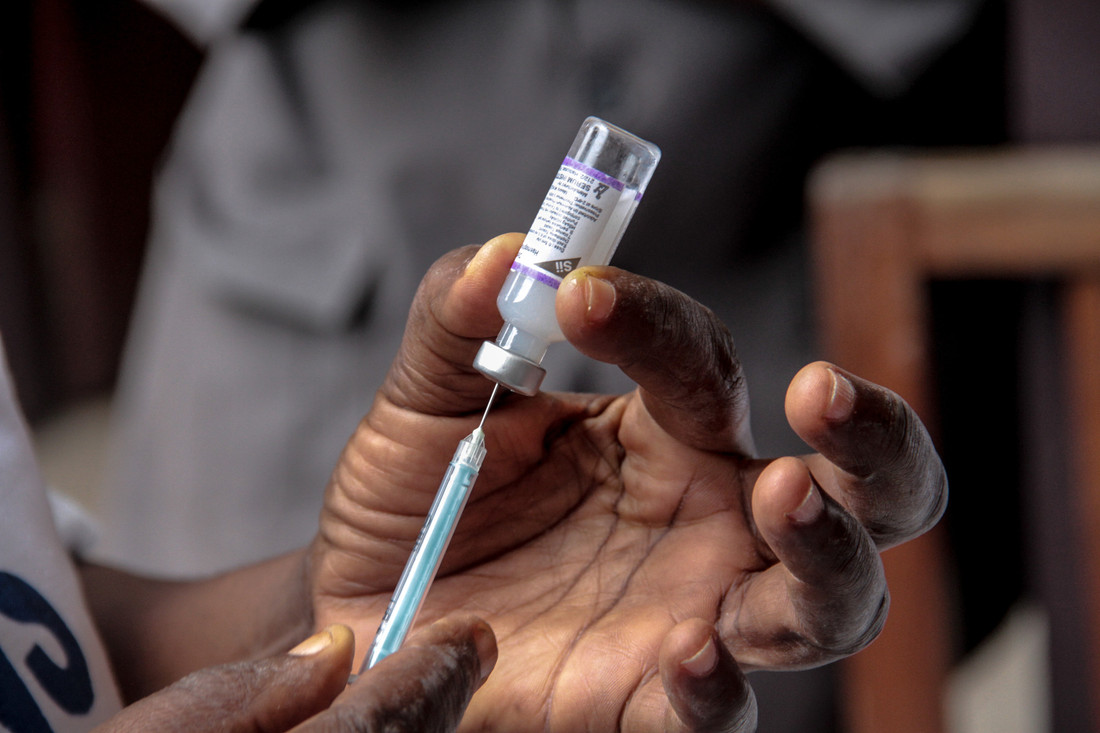
However, a new approach to development could help to make vaccines against such diseases more viable. This month a pharmaceutical company reported promising results from an early human trial of their DNA-based Zika vaccine. All volunteers in the study developed Zika-specific antibodies. This is a step forward not just in it the development of an effective Zika vaccine, but towards a novel approach to vaccine development.
Traditional vaccines consist of a killed or inactivated form of a virus or bacterium. This is injected into the patient and the body responds by producing antibodies. If the patient later becomes infected, the presence of these antibodies means that their immune system is primed to fight the infection.
Inovio’s DNA-based vaccine works differently. A DNA fragment is built in the lab to resemble a section of the Zika virus’ DNA. This is injected, enters the patient’s cells and instructs them to make viral proteins. These proteins trigger the production of Zika-specific antibodies.
This approach has several major advantages over traditional vaccines. DNA-based vaccines are cheaper and quicker to manufacture: traditional vaccines can take years to develop, whereas this Zika vaccine took only seven months from its first design to the start of clinical trials.
Crucially in the production of vaccines for viral diseases, these vaccines are very easy to modify if the virus mutates. Viruses are known for their fast mutation rate – this is why new seasonal flu vaccines have to be developed each year. The proteins targeted by antibodies can change so rapidly as result of mutation that antibodies against last year’s flu strain may no longer provide protection.
Mutation can reduce the incentive for pharmaceutical companies to invest in vaccines – it doesn’t make economic sense to invest huge amounts of money and resources in a vaccine that will only be effective for a short period of time.
However, DNA vaccines could mostly circumvent this problem. The DNA sequence produced in the lab can be modified to account for the mutations that have occurred, and vaccines against emerging strains could be produced in a matter of weeks. Combined with the lower costs of manufacture, this approach could incentivise companies to invest in vaccine development.
The development of the DNA-based Zika vaccine is at an early stage, with more work remaining to test efficacy and safety. However, if DNA-based vaccines prove effective, they could boost investment in vaccines against emerging infectious diseases and enable a much more rapid response to epidemics like Zika. That could prove crucial as the threat of major outbreaks intensifies.











