Celina Hanson (Gavi), Paul Bloem (WHO) & Emily Loud (Gavi).
Women in developing countries disproportionately suffer from the burden of cervical cancer, yet often their countries do not have resources to establish screening programs that save women’s lives elsewhere. In these countries, human papillomavirus (HPV) vaccination provides an amazing opportunity to prevent cervical cancer and protect women’s health.
Vaccine delivery poses challenges, many of which are the same that we see for other vaccines. These may include not having enough fridges to keep the vaccines cold, or not enough health workers to vaccinate children, or children living in isolated rural areas where distance and unpaved roads make it harder for parents to reach facilities.
Other challenges are unique to the HPV vaccine. To start, most countries have experience vaccinating infants and these vaccinations are given when women visit clinics with their babies. The HPV vaccine, however, is not given to babies but to girls between 9 and 13 years old.
Here are some lessons from the experiences of introducing countries so far:
Learning by doing
Before introducing the HPV vaccine at a national level, many countries have started to learn by vaccinating girls in a small area to determine the best delivery strategy. Doing this in a Gavi supported pilot or demonstration also allows countries to secure the technical assistance they need, to develop training and monitoring materials, and to consider the integration of vaccination with other health services. This learning allows countries to develop solutions to challenges that were not anticipated.
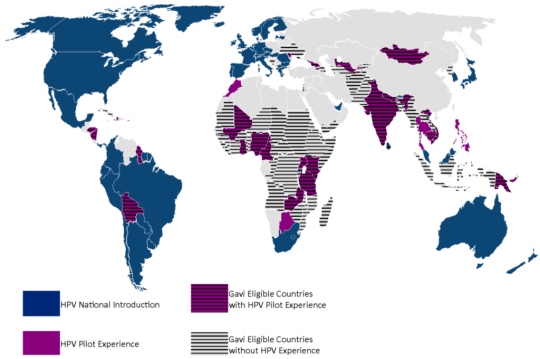
Map: from original article.
Health and education – achieving more together
Schools have been a popular place around which to centre much of the delivery of HPV vaccines in these countries. In order for this strategy to work well, strong co-ordination between health and education sectors is essential. From planning the vaccination dates, engaging schools in mobilization of parents and girls, to supporting implementation of vaccination sessions – schools and teachers make important contributions, which have translated in high acceptance levels of this new vaccine.

A venue for HPV vaccination in Ghana. Photo: Gavi/Evelyn Hockstein
How to reach all girls affordably?
In order to reach all girls with the vaccine, countries are testing other strategies to reach different populations as well, such as outreach and using alternative facilities. Delivering HPV vaccine with other health interventions like deworming, menstrual hygiene education or tetanus shots is also being explored.

A girl living in a rural Ethiopian community. Photo: Gavi/Niligun Aydogan.
HPV vaccination as a catalyst
HPV vaccination is a highly effective intervention – but it must be linked to effective screening and treatment programs to prevent cervical cancer. The demonstration programs assist countries to strengthen comprehensive cervical cancer prevention and control plans. Over time, it can also act as a catalyst for even wider health interventions that benefit all adolescents.

Kids pose together in the Pokhara region of Nepal. Photo: Gavi/Oscar Seykens.
This blog was based on a review of progress that was recently published in the journal Vaccines. Read it in full here.