Leprosy, scabies and yaws - Togo’s neglected tropical skin diseases need attention
Neglected tropical diseases of the skin are stigmatised, and may affect an individual’s quality of life
- 28 March 2023
- 5 min read
- by The Conversation

Neglected tropical diseases are a group of 20 diseases found mostly in tropical regions that are strongly associated with poverty. Among them are skin diseases like scabies, leprosy and yaws. They are caused by some bacteria, viruses, mosquitoes or mites and, according to the World Health Organization (WHO), they affect more than one billion people worldwide, mainly in lower-income settings.
These skin diseases are particularly common in most African countries. For example the estimated at-risk population on the continent requiring intervention for lymphatic filariasis (an abnormal enlargement of body parts, causing pain, severe disability) was 341 million in 2020. And 99 percent cases of onchoerciasis also known as river blindness occur on the continent.
Children are usually more affected than adults, and risk factors include poverty, overcrowding, malnutrition, and humidity.
Neglected tropical diseases of the skin are stigmatised, and may affect an individual’s quality of life or psychological well-being. They can be difficult to diagnose and there are typically few, if any, dermatologists in areas where they are common.
Our team led a study in Togo, in west Africa, to assess the burden of these diseases. We found a high prevalence of several skin infections and evidence of social impact experienced by the patients. We suggest that local and national health authorities, in Togo and more widely across Africa, consider an approach that integrates skin management along with general public educational programmes to encourage early reporting of cases to the health service.
What we found
The study population was two schools in Lomé, the Togo capital city, and one rural community setting, the village of Ndjéi, Ndjéi has a population of about 3,000 and is 400km north-east of Lomé.
Mobile clinics were set up in the schools and community sites, between June and October 2021. Medicines were provided free of charge to participants. Where necessary, individuals were referred to the appropriate service in the healthcare system. The team looked to record the skin infections listed by the WHO, and as well as diagnoses of other fungal diseases.
Have you read?
Skin examinations were carried out on a total of 1,401 people. This included 954 in Ndjéi – 68.1% of the total. In the Lomé school setting, 447 children (31.9% of the total sample) were examined out of 782 regularly enrolled children.
Overall, we found a large number of skin infections. There were 105 observed cases of skin diseases classified as neglected tropical diseases (7.5% of all the people we examined had one of these diseases). And there were 333 cases of fungal disease (23.8% of all the people we examined had a fungal disease). Where data are available, these numbers are perhaps comparable with other studies though rates can vary greatly. For example, an Ethiopian study found fungal disease prevalence of 21%, similar to the 23.8% we found here. However, another study in Benin reported a prevalence of 49%.
The 105 cases of skin neglected tropical disease included 20 in schools and 85 in the rural community setting. Neglected tropical diseases are often more common in rural areas.
Across school and community data, there were 68 cases (6.7% of the total) of neglected tropical diseases in children, and 37 cases (9.7%) in adults.
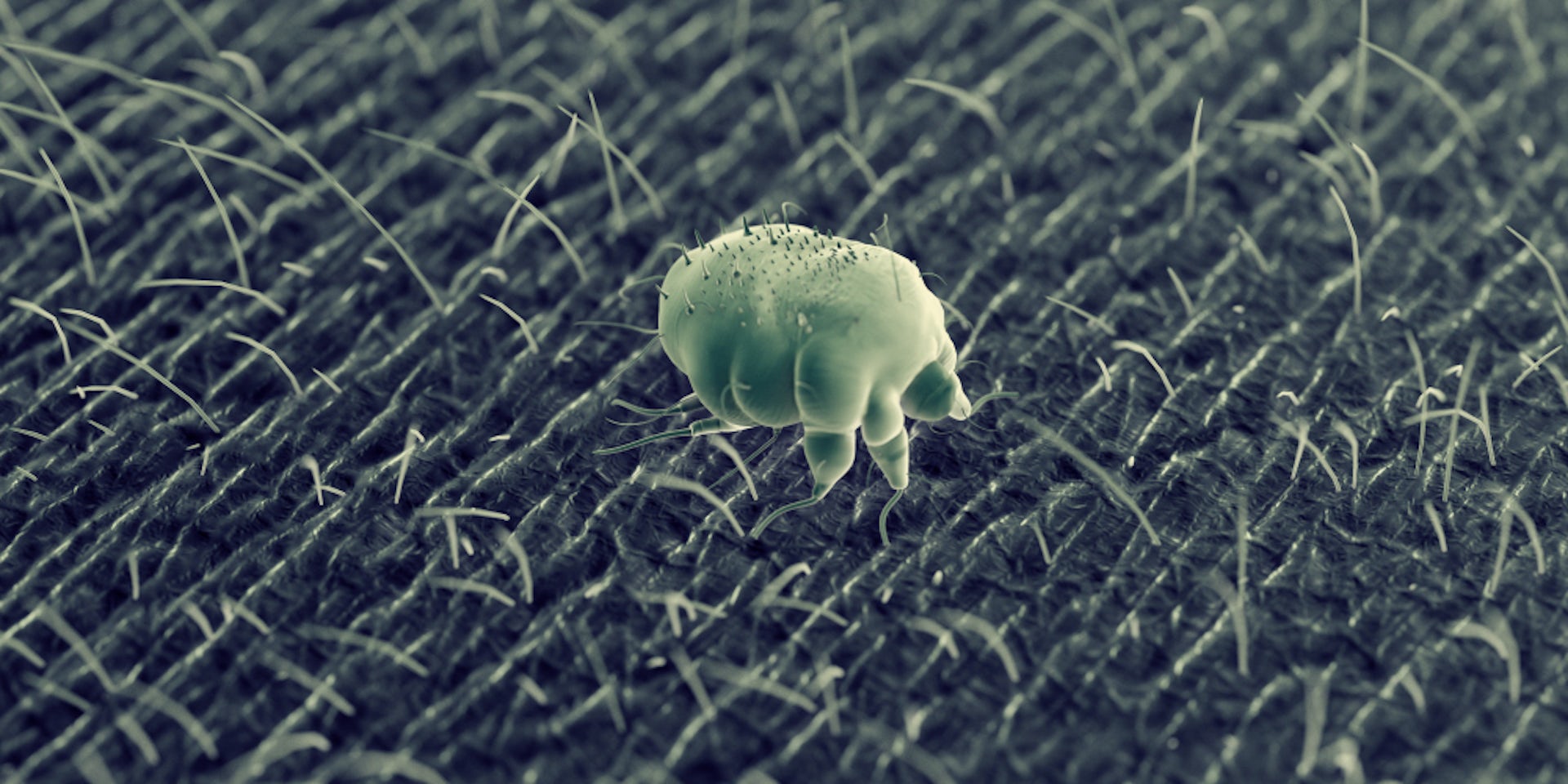
The most prevalent of the skin diseases (other than fungal diseases) was scabies, observed in 86 patients (6.1%). Scabies is an unpleasant infection transmitted by mites that burrow underneath the skin and lay eggs. It can be incredibly itchy and lead to secondary consequences, including other skin infections and kidney disease. Treatment in Africa is often a skin lotion called benzyl benzoate, and the oral medicine ivermectin, both of which are very effective at killing the scabies mites.
The effectiveness of traditional remedies such as herbal cataplasm (a home-made healing paste of different herbs and plants) to treat skin infections in different parts of Africa is uncertain. Their use could promote a secondary bacterial infection or cause eczema around the skin wounds.
Among other diseases observed in our study, the team also found cases of leprosy, yaws and Buruli ulcer.
A call to action
Although it was not the main motivation behind the study, we also asked questions about stigma. In the school setting, five (6%) children with cutaneous neglected tropical diseases reported being stigmatised, and four of them had refused to go to school for one or more days. In Ndjei, 44 (4.6%) participants reported having experienced stigma and 41 (93.2% of those) missed at least one day of school or work.
Stigma and the problem of absenteeism associated with skin diseases should encourage the health authorities to make the treatment of these diseases free of charge, including consultation fees and drugs. Health promotion and education is important. This can help to persuade the population to seek medical care. An integrated management approach as well as mass drug administration programmes may be effective in controlling the diseases, and are recommended as part of the WHO neglected tropical diseases roadmap.
This study has provided evidence around the numbers and types of skin neglected tropical disease and fungal infections found in school and rural communities in Togo. The data has been presented within Togo and to the relevant international groups such as the WHO.![]()
Authors
Michael Head, Senior Research Fellow in Global Health, University of Southampton
Bayaki Saka, Professor of Dermatology, University of Lome
Palokinam Pitche, Professor of Dermatology , University of Lome

This article is republished from The Conversation under a Creative Commons license. Read the original article.
Disclosure statement
Michael Head has previously received funding from the Bill & Melinda Gates Foundation and the UK Department for International Development.
Bayaki Saka and Palokinam Pitche do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
Partners
University of Southampton provides funding as a member of The Conversation UK.