From smallpox to mpox: the surprise cost of eradicating a virus
The demise of smallpox and rise of mpox are inextricably linked, highlighting the importance of surveillance after eradication.
- 4 November 2024
- 11 min read
- by Linda Geddes
In October 1977, a Somali hospital cook called Ali Maow Maalin fell ill with a headache and fever. Four days later, he developed an ominous rash on his body. It was smallpox; a disease that humans had lived in fear of for millennia.
Yet, Ali’s infection marked the end of this reign of terror. He is the last known person to have been infected with naturally-occurring smallpox.
Two years later, the disease was officially declared eradicated – the only human disease ever to have achieved this status, and a massive victory for public health and vaccines.
But this isn’t the end of the smallpox story. As the variola virus that causes it was being purged from the face of the earth, another virus was emerging in remote forested regions of Central West Africa, and the vacuum left by smallpox may have created conditions for it to flourish.
Caused by a close relative of variola, and with similar – albeit less deadly – symptoms, an early observation was that monkeypox (now known as mpox) predominantly struck individuals who hadn’t been vaccinated against smallpox – prompting experts to speculate that it might become a bigger problem once mass smallpox vaccination ended.
Today, mpox is a major problem for global health. Although scientists still believe that stopping smallpox vaccination was the right thing to do, because the first and second-generation vaccines have an unacceptable side-effect profile in the absence of smallpox, they argue that the rise of mpox could provide valuable lessons both on the importance of surveillance and on ensuring valuable skills and infrastructure aren’t lost once a disease no longer poses an imminent threat.
Viral relatives
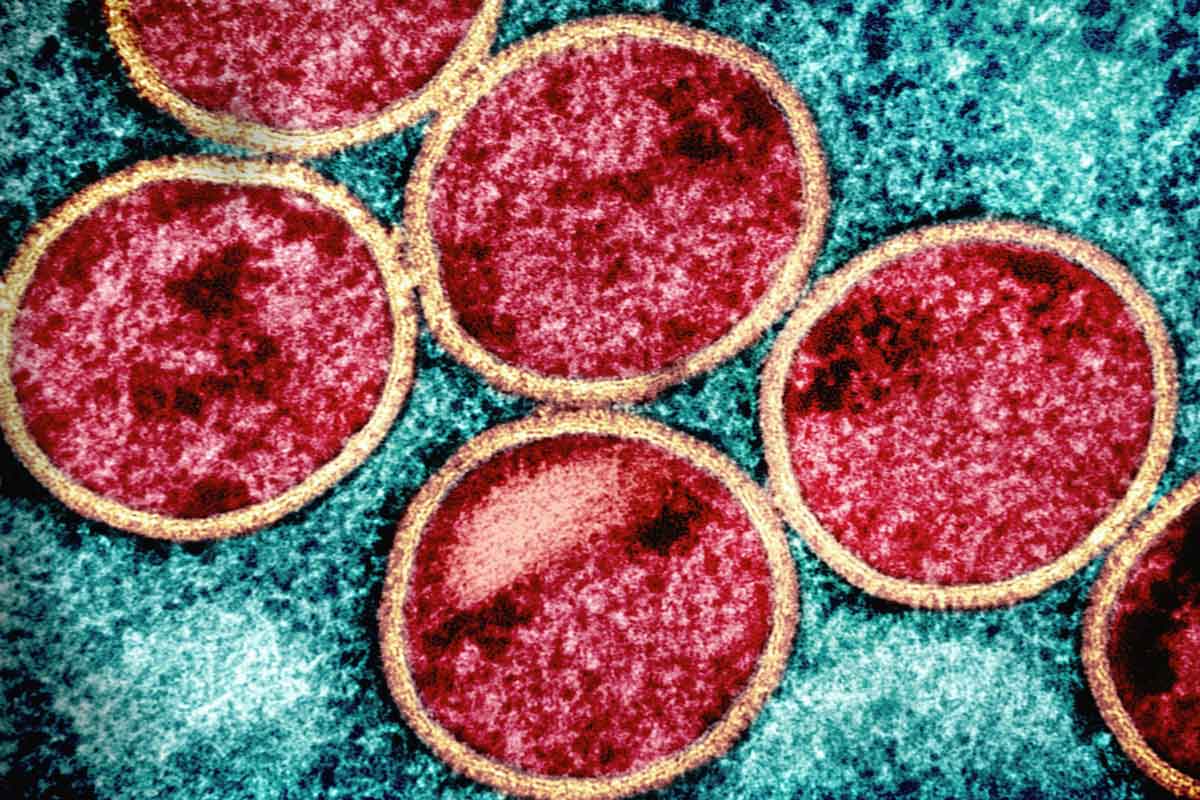
Both smallpox and mpox are caused by orthopoxviruses – brick-shaped DNA-viruses that cause a number of different human and animal diseases.
“Besides variola (smallpox), there are probably about a dozen highly related orthopoxviruses,” says Raina MacIntyre, Professor of Global Biosecurity at the University of New South Wales in Sydney, Australia. “These include mpox; vaccinia, or cowpox, which is what most smallpox and mpox vaccines are based on; Ectromelia virus, which causes mousepox; and borealpox – initially known as Alaskapox.”
Because they’re very closely related, smallpox vaccination and exposure to variola likely conferred protection against all of them, to some extent.
The rise of mpox could provide valuable lessons both on the importance of surveillance and on ensuring valuable skills and infrastructure aren’t lost once a disease no longer poses an imminent threat.
But with mass vaccination having ended five decades or more ago, and no more smallpox, the global population has become increasingly susceptible to these other viruses
“That combination of mass vaccination and exposure gave a level of immunity in the population that just isn’t there today,” says MacIntyre. “The vaccine wanes, so more than 40 years after the last smallpox vaccine programmes ended, even people vaccinated in the past will have minimal immunity.”
Global victory
The decision to eradicate smallpox marked a turning point in our relationship with pathogens. Although previous efforts to eradicate hookworm, malaria and yellow fever had failed, smallpox was different because the virus that causes it only has one host – humans – and there was an effective vaccine against it.
In 1959, the World Health Organization launched the smallpox eradication programme, which aimed to permanently reduce the number of smallpox cases to zero. Thanks to the combined efforts of health agencies around the world, not to mention legions of vaccinators, the disease was rapidly eliminated from country upon country.
Lessons from smallpox eradication continue to shape the way that we respond to other infectious disease threats today. For instance, ring vaccination, which involves vaccinating the contacts of infected people, and people who are in close contact with those contacts, has been used extensively during recent outbreaks of Ebola, but was first deployed with great success during the eradication of smallpox.
By the early 1970s, various nations including the United Kingdom and United States, had stopped routinely vaccinating children against the disease; by the late 1970s, all routine smallpox vaccination had ceased, apart from US military personnel.
“The eradication of smallpox is one of the greatest achievements of public health, and the natural next step was to move resources that had been dedicated to vaccinating against smallpox, to other pathogens,” says Anne Rimoin, Professor of Epidemiology at the UCLA Fielding School of Public Health in Los Angeles, US.
The smallpox vaccines that were in use at the time also weren’t entirely risk-free, with between 14 and 52 people out of every 1 million people vaccinated for the first time experiencing potentially life-threatening reactions that required immediate medical attention. But they were extremely effective, protecting against smallpox infection in around 95% of those vaccinated. Compared to the risks of catching smallpox, which killed approximately three in every ten people and left many survivors with severe scarring or blindness, vaccination was a no-brainer. “Once there was no more smallpox, the risk of death from vaccine was greater than the risk of death from smallpox, and so vaccination stopped,” says David Heymann, Professor of Infectious Disease Epidemiology at the London School of Hygiene and Tropical Medicine.
Even so, he and others predicted that there might be a cost.
“Everything has a cost. And with smallpox eradicated essentially from the planet, I think it made good sense to stop vaccination. The greater issue has been the lack of investment in surveillance and surveillance systems to be able to identify cases and get in front of outbreaks, rather than chasing behind them.” ”
- Anne Rimoin, Professor of Epidemiology at the UCLA Fielding School of Public Health in Los Angeles, US
A new pox virus
The first human case of monkeypox (now known as mpox) was reported in 1970, in a nine-month-old child, who had just returned from a trip to visit their grandmother in a village just south of the Congo river, in what is now the Democratic Republic of the Congo (DRC). It was followed by sporadic cases in five central and west African countries throughout the 1970s.
Researchers who had studied this new virus were aware of its similarities to variola virus, and worried that the discontinuation of routine smallpox vaccination might leave populations more susceptible to this and other orthopoxviruses.
“There has always been a fear that mpox would replace the epidemiological niche left by smallpox as vaccination decreased,” says Heymann, who spent several years in DRC investigating whether mpox infection was more common among unvaccinated children.
On the other hand, mpox was still relatively rare, with most cases occurring only after close contact with wild animals. Also, when infected people did pass the virus to other people, these transmission chains tended to be short and limited to other unvaccinated family members.
Even so, WHO took these concerns seriously enough to support an active surveillance programme for human mpox between 1981 and 1986, and the data was used to model the epidemic potential of the disease. Based on such studies, scientists concluded that, while the magnitude and duration of mpox epidemics would probably increase as vaccine-derived protection declined, mpox virus was unlikely to persist in human populations.
What these modelling studies couldn’t predict, however, was how the world and the mpox virus might change in subsequent decades. For instance, one assumption in the 1980s was that there would be a growing population shift from rural to urban areas in countries such as DRC, where mpox was endemic, meaning people would be less likely to encounter animals carrying the virus.
Instead, the eruption of civil war in the late 1990s, followed by decades of localised conflict, has pushed people deeper into the forest and made them more dependent on bushmeat and the harvesting of fuelwood for survival.
Malnourishment, poor access to medical care and conditions such as HIV that weaken the immune system have further also increased people’s vulnerability to infection. Meanwhile, mpox viruses have evolved to become more contagious and to transmit in different ways – including through sexual contact.
Combined with reduced population immunity to orthopoxviruses, “these factors are creating a perfect storm where you have populations that are highly exposed and still reliant on bushmeat as a primary source of nutrition,” says Rimoin, who has been running a research programme in DRC since 2002.
Residual protection
After active surveillance for mpox ended in 1986, there was a long period during which the burden and geographic range of human mpox was largely unknown. So, in the mid-2000s, Rimoin initiated a study to try and fill this gap. After training health care workers in how to identify suspected mpox cases and refer them for testing, she and her colleagues conducted active surveillance for mpox in areas of DRC where the virus was known to circulate.
Compared to data collected in the same areas during the 1980s, they identified a 20-fold increase in the incidence of mpox and found that people who had previously been vaccinated against smallpox were around five times less likely to catch the disease than unvaccinated individuals.
“Our data suggest that 30 years after the eradication of smallpox, the incidence of human monkeypox has dramatically increased in the DRC,” they wrote in The Proceedings of the National Academy of Sciences in 2010.
Rimoin and her colleagues called for improved surveillance and epidemiological analysis to better understand these patterns and reduce the risk of wider spread, warning not only of the potentially serious risk to people in DRC, but the possibility of mpox becoming a “global health concern”.
Fourteen years later, those concerns have become an alarming reality. In August 2024, WHO declared mpox a public health emergency of international concern (PHEIC) following the emergence of a new clade of mpox virus, its rapid spread in eastern DRC and the reporting of cases in several neighbouring countries.
The PHEIC is the second in two years relating to mpox, with a separate one having been declared in 2022 for the 2022–23 multi-country outbreak that resulted in at least 99,176 cases worldwide and 208 deaths. MacIntyre points out that epidemics of clade 1 mpox were also occurring in DRC during 2022, “but the attention of the world was focused on clade IIb in high income countries” at that time.
Future threats
Even with hindsight, no one is suggesting that ending routine smallpox immunisation was a mistake – but given the warning signs, many believe that more could have been done sooner to try and head off the threat.
“Everything has a cost. And with smallpox eradicated essentially from the planet, I think it made good sense to stop vaccination,” Rimoin says.
“The greater issue has been the lack of investment in surveillance and surveillance systems to be able to identify cases and get in front of outbreaks, rather than chasing behind them.”
For MacIntyre, a crucial turning point came in 2017, when large numbers ofclade 2 mpox cases started to be reported in Nigeria, followed by a handful of cases in the UK, Israel and Singapore. Unlike previous outbreaks, those affected were predominantly young men with evidence of ready human-to-human transmission.
MacIntyre says: “When unprecedented, large epidemics of mpox began in Nigeria and DRC in 2017, and when travel imported cases occurred in 2018 and 2019 in the UK, Israel and Singapore, no one heeded the warning. Our research showed that 2017 marked the year when the critical threshold of protection against vaccinia/variola fell below 2%, and this corresponded with the surge in mpox ever since.”
As further time passes, the proportion of the global population with residual immunity to pox viruses will continue to wane. Even those who received the smallpox vaccine before mass vaccination ended are unlikely to be well protected today.
“Immunity does wane, with data from the literature suggesting a rate of around 1.4% a year. So, if you were vaccinated in the 1960s, you’ve really got very little immunity left – although you will have immunological memory, which means that if you get vaccinated again, you will respond faster and with a higher level of protection,” MacIntyre says.
So, what to do about it. Although the third-generation smallpox vaccines currently being deployed against mpox in DRC are based on attenuated virus strains and associated with fewer side effects than earlier vaccines, their availability remains limited – as are the resources, training and infrastructure to deliver them.
Experience delivering vaccines using bifurcated needles – two-pronged devices that only pierce the top-most layer of the skin – has also been lost. These were widely used during smallpox eradication campaigns, and some current smallpox vaccines that are now being considered for mpox are delivered this way – but doing so will require health care staff to reacquire these skills.
Have you read?
A return to mass vaccination against smallpox seems unlikely for now – although circumstances could change. One scenario that keeps MacIntyre awake at night is the possibility of a bioterror attack involving the release of a laboratory-synthesised orthopoxvirus, including reconstructed smallpox virus. Given our current lack of immunity to pox viruses, this could be calamitous.
Heymann believes that this is something we should keep in mind as the global health community considers eradicating other diseases, such as polio. He says: “Poliovirus has already been constructed [from scratch] in a US laboratory. I believe that if polio is ever completely eradicated, we should be wary of stopping vaccinating against it, because of the threat of bioterrorism.”
Even without these doomsday scenarios, Rimoin says we should anticipate more cases of pox infections in humans as immunity continues to wane. “This means we need to do better at monitoring for potential threats, and then deploying the targeted use of vaccines, therapeutics, and other modes of prevention.”
A major lesson from the cessation of smallpox vaccination and the rise of mpox is the need for continued surveillance, even once the immediate threat appears to have passed. Ongoing surveillance also means there is a skeleton crew of individuals with the experience and expertise to identify, test for and deploy resources against the pathogen of interest, if it does begin to reemerge, rather than having to retrain everyone from scratch.
“The key is that when you eradicate a pathogen and you no longer are vaccinating against it, you no longer have any kind of natural or vaccine-induced immunity to it. And so, you have to think about other pathogens that could fill that niche that may previously have been held at bay because of cross-protective immunity,” says Rimoin. “Nothing happens in a vacuum. That’s why surveillance is so critical.”
More from Linda Geddes
Recommended for you








