What happens if COVID-19 mutates?
Reports of a potentially more infectious form of the coronavirus have fed fears that a "mutant” version of the virus could arise. But what does mutation actually mean and is it really a cause for concern?
- 22 July 2020
- 5 min read
- by Ciara McCarthy
Thanks to science fiction, the word “mutant” has become associated in popular culture with something that is abnormal and dangerous. Yet in reality, viruses like SARS-CoV-2, the virus that causes COVID-19, are mutating all the time and often this process does not have any impact on the risk the virus poses to humans.
A mutation is simply a change in the virus’ genome: the set of genetic instructions that contain all the information that the virus needs to function. When the virus replicates, this set of instructions needs to be copied, but errors can creep in during this process. Depending on where in the genome mistakes occur, they can have a negative or positive impact on the virus’ ability to survive and replicate. Or, as is the case the majority of the time, they may have no impact at all.
Mutations can show how the virus is evolving
These so-called neutral mutations may not be useful for the virus, but they can be useful to the scientists who are investigating it. They can act as a trail of breadcrumbs that provide information about how the virus originated and how it is spreading on a global and local level.
Mutation analysis has suggested that the first introduction of COVID-19 into Italy may have been linked to an infection in Germany, and further cases from Italy may have come from Singapore. Sufficient difference between genome sequences can rule out suspected transmission routes, whilst similarities can suggest (although not confirm) that transmission has occurred.
However, it is possible that mutations could occur that make the virus more dangerous to humans. A mutation was recently identified in the SARS-CoV-2 spike protein, which is on the surface of the virus and plays an important role in helping viral particles enter human cells. The G614 variant is thought to have arisen in Europe in about February and has since become the most dominant strain worldwide. Evidence from the lab suggested that this mutation could make SARS-CoV-2 more infectious, and the rapid spread of the G614 variant seems to lend weight to that theory.
However, there are other factors that play into whether a particular variant is more successful than others. For example, there is evidence that of the lineages of SARS-CoV-2 that have become established in the US, most originated in Europe. It could be that this is because these variants were better at spreading in populations, but it could also just be due to the large amount of travel between the US and Europe that would still have been occurring early on in the pandemic. Many scientists have been cautious about drawing any conclusions with regard to the potential impact of the D614G mutation, of which G614 is a variant, before there is more data available.
The COVID-19 virus may mutate more slowly than flu
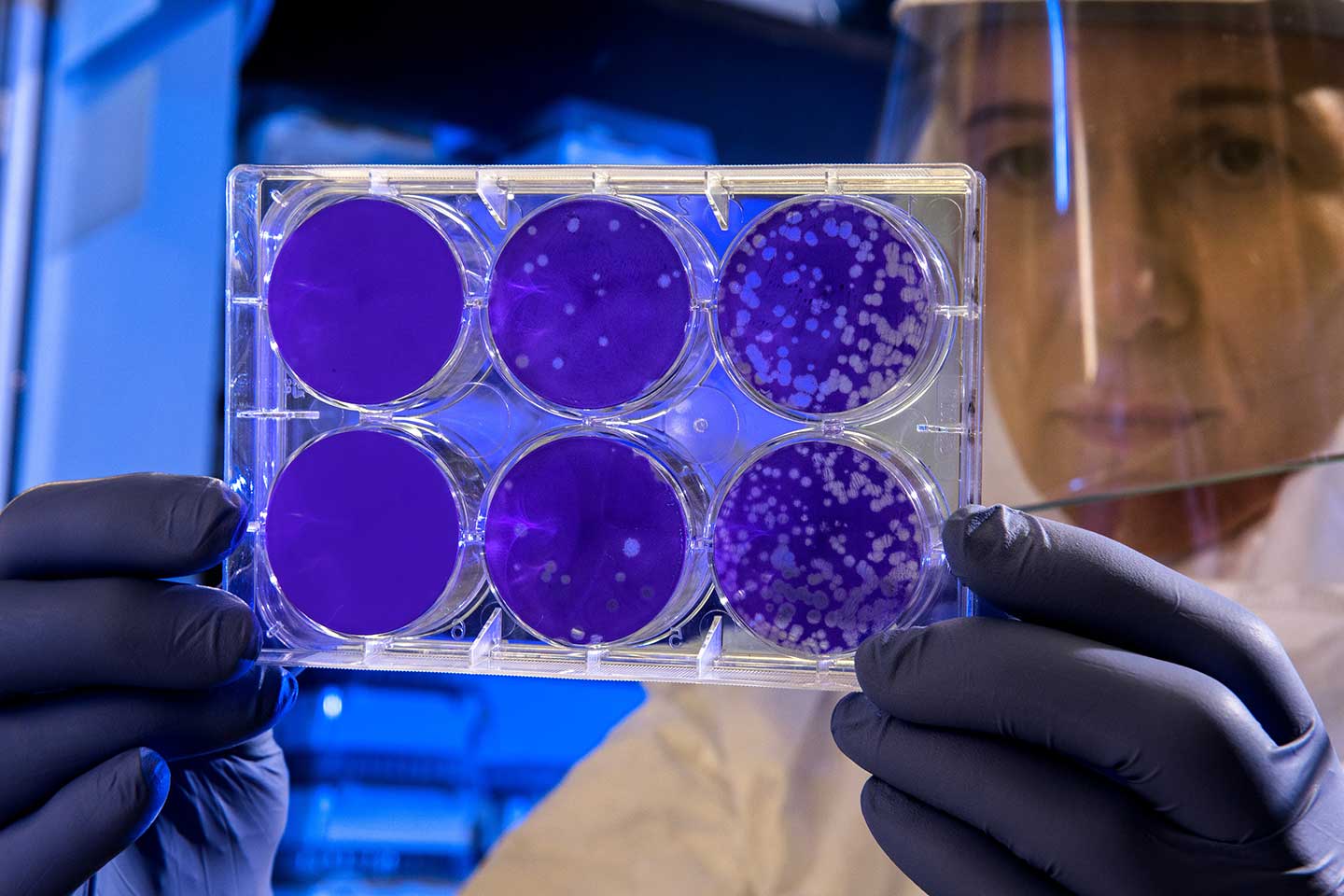
Evidence suggest that mutations arise at a slower rate in coronaviruses than in other viruses such as influenza. This is because coronaviruses proof-read after replication, helping to reduce the number of errors that accumulate. This is good news for scientists working to develop vaccines and pharmaceuticals in response to COVID-19, as mutations that lead to a change in the structure of the virus could reduce the effectiveness of these tools. Whilst in the case of flu, vaccines are often much less effective within a year or two or their development due to the rapidly-changing nature of the virus, this may be less of an issue with COVID-19.
Mutations are impossible to predict
In terms of how the virus could mutate in the future, it is often suggested that it is likely to become less harmful over the course of the pandemic. As the proportion of people who are immune to the virus increases, there are fewer and fewer opportunities for the virus to spread to a new host. Therefore, according to evolutionary theory, the variants of the virus that are less likely to kill their current host will be more successful. This is thought to have occurred with the virus that caused the Spanish flu pandemic in 1918-1919, which killed 50-100 million people at that time but continued to circulate for around 40 years as a less lethal strain.
However, this theory has also been disputed by those who argue that influenza viruses with both low and high lethality were able to cause pandemics in the 20th century, suggesting that how harmful the virus is to humans may not be a key determinant of whether it can successfully continue to spread in the population. Therefore, whether SARS-CoV-2 will evolve to become less lethal over time remains to be seen.
By their very nature mutations are a random event, and so predicting when and where they will occur and the impact this might have is a very difficult task. However, monitoring their spread is not just important for understanding how changes in the virus could alter its lethality or transmissibility, but also how they could affect the tools we are developing in response.