Why some people might be immune to certain COVID-19 vaccines
Vaccines based on the common cold virus are at the forefront of the COVID-19 vaccine race, but they may be less effective in people who have previously been infected by these common pathogens. So how could we overcome this challenge?
- 16 October 2020
- 4 min read
- by Linda Geddes
Of the many COVID-19 vaccines currently in development, those based on a modified version of the adenovirus, or the common cold virus, were among the first to reach human trials.
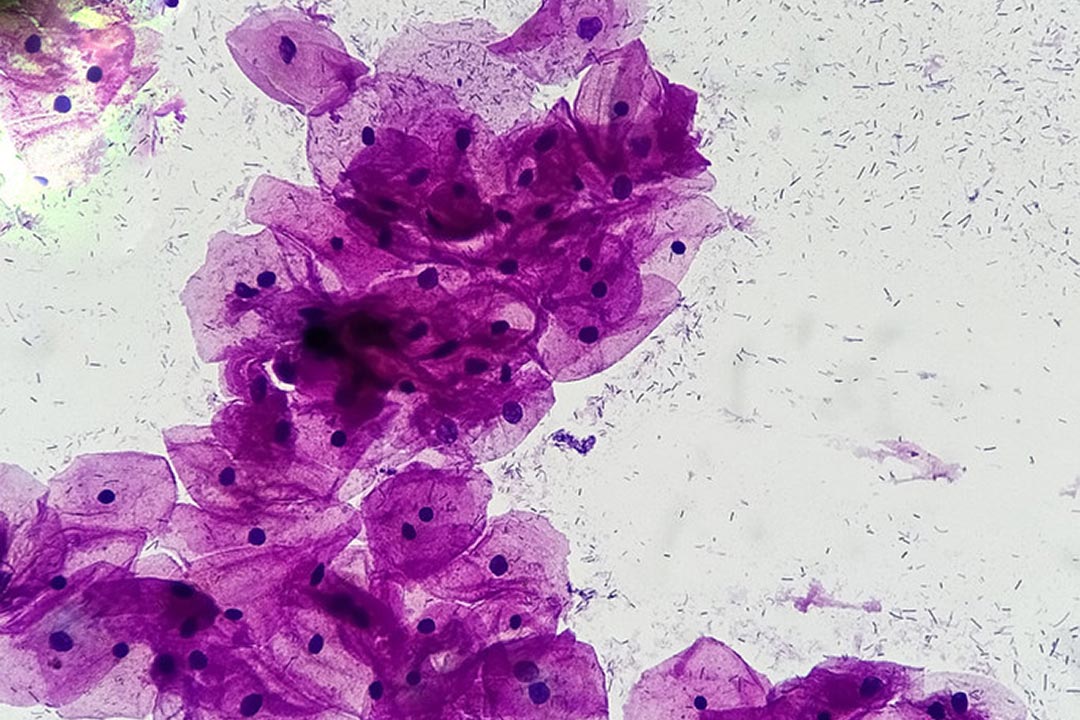
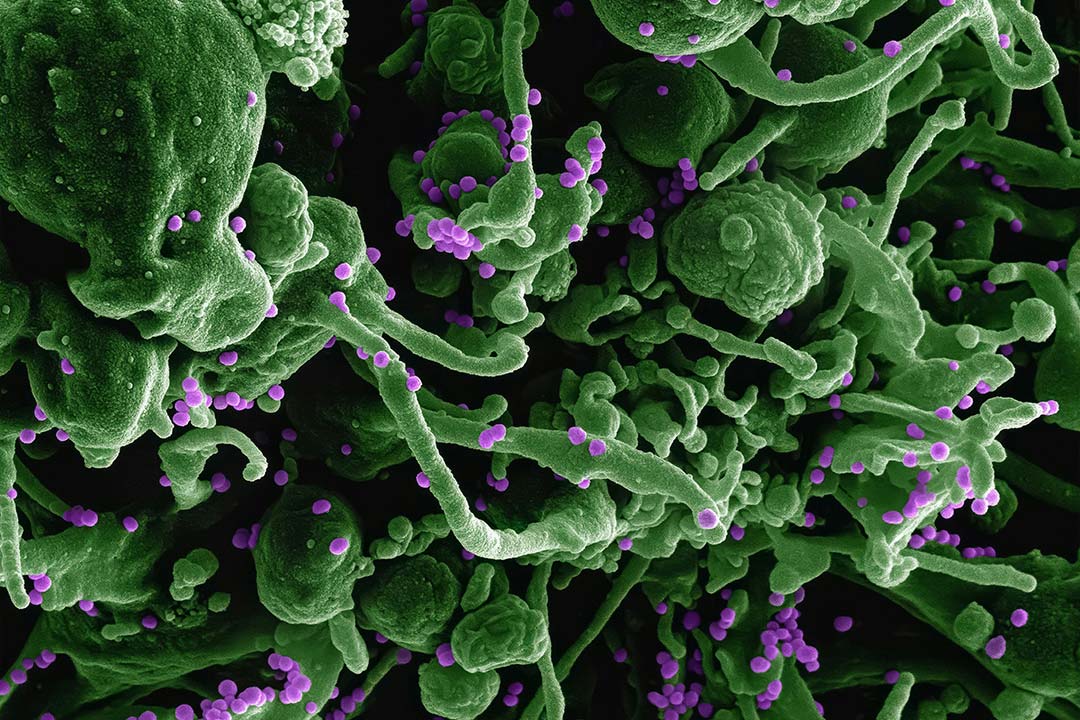
Unlike conventional vaccines, which use a killed or weakened form of the pathogen (or a protein from it) to trigger an immune response, vector vaccines employ a different virus to deliver antigens from the pathogen into our cells. Often, the virus used as a delivery system is an adenovirus, a group of viruses responsible for causing mild infections in humans, associated with symptoms like a runny or blocked nose, cough or conjunctivitis. The vector is stripped of any disease-causing genes, and often those which enable it to replicate as well, and modified to carry a gene for the antigen of interest – such as the spike protein that SARS-CoV-2 uses to gain entry to cells. This virus is then injected into healthy people, where it sets about infecting cells, just as it would do naturally – but rather than churning out new virus, the infected cells make antigen instead.
If someone has been exposed to a version of the virus, their immune system may destroy it before it delivers its payload – meaning the vaccine may not work.
A key benefit of this approach is that the antigen is produced within cells, rather than merely circulating in the blood. This means that as well as being detected by antibody-producing B cells, it is also picked up by T cells, which seek out and destroy any cells that are infected with the pathogen. By triggering both of these types of immune response, the hope is that the vaccine will be more effective.
However, using a common virus to deliver the antigen also creates challenges. If someone has previously been exposed to a version of the virus, their immune system may recognise the modified version and destroy it, before it manages to deliver its payload – meaning the vaccine may not work. This so-called “anti-vector immunity” also makes giving people booster shots of an adenoviral vector vaccine difficult, if it involves injecting the same viral vector for a second or third time.
How many adenovirus-based vaccines are there?
Adenoviral vaccines have previously been developed for HIV, tuberculosis, malaria and Ebola – although Ebola is the only disease for which such a vaccine, produced by Johnson & Johnson, has been approved for human use. A different adenoviral vaccine is also used to immunise wild animals against rabies.
Of the COVID-19 vaccines currently in development, four of those in phase 2 or 3 trials use an adenovirus as the vector, with other adenovirus-based vaccines at earlier stages of clinical development. Of these vaccines, the most common vector is adenovirus 5.
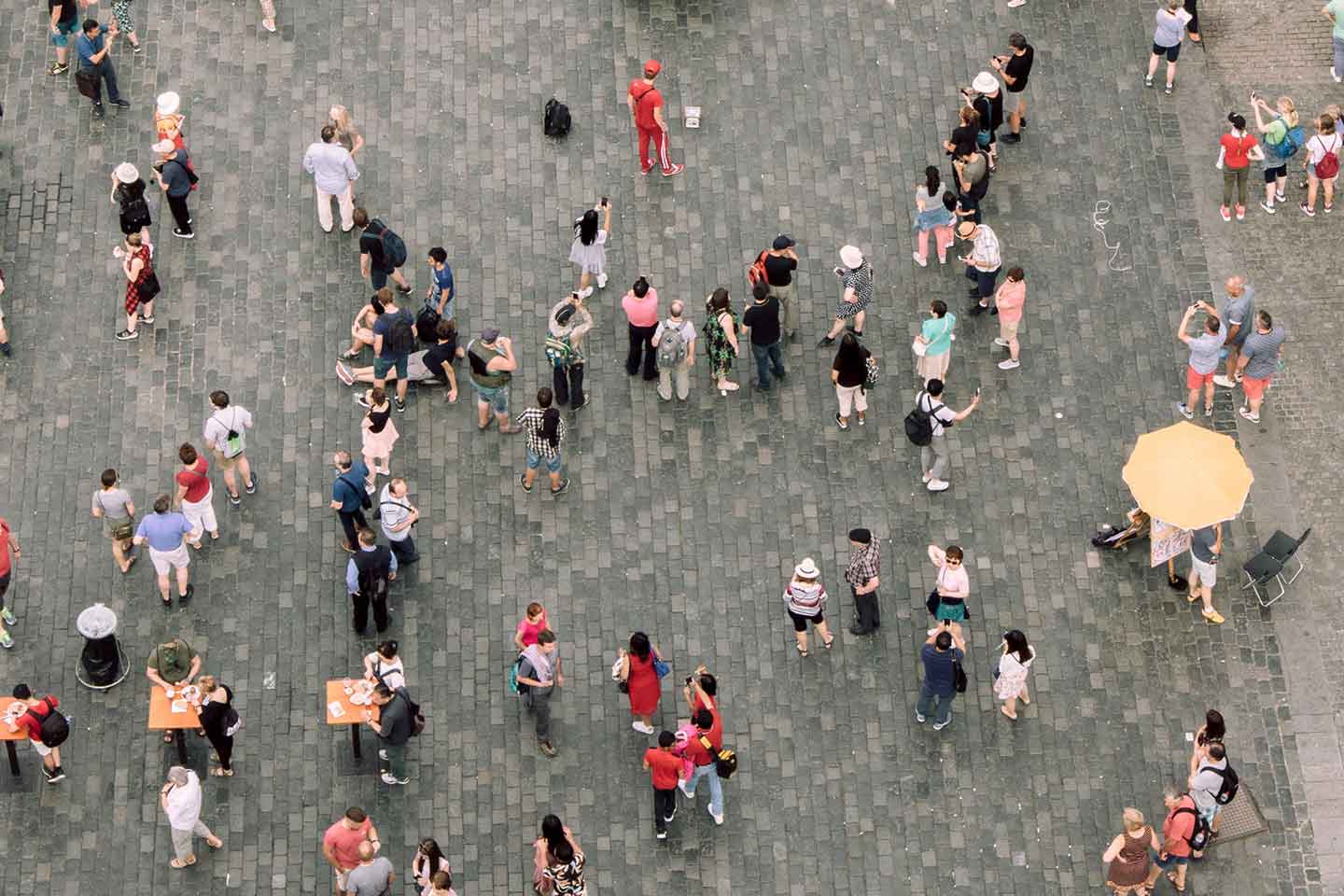
Adenovirus 5 (Ad5) is one of many viruses responsible for causing the common cold. In the United States of America, approximately 40% of the population is thought to have antibodies to it, whereas in sub-Saharan-Africa and West Africa, as many as 80–90% of people do.
Will a COVID-19 vaccine based on Adenovirus 5 work?
At this stage, it is impossible to say, but the Chinese company CanSino Biologics is optimistic. It has already developed an Ebola vaccine based on Ad5, which the Chinese government has approved for emergency use and stockpiling. One of its COVID-19 candidate vaccines also uses Ad5 to deliver a chunk of the SARS-CoV-2 spike protein into cells.
Other companies are hoping to get around this issue by delivering their Ad5-based vaccines orally, or via a nasal spray, to give the vector a greater chance of infecting cells before encountering antibodies in the blood.
Ad5 isn’t the only adenoviral vector in the game. Johnson & Johnson’s candidate vaccine uses a different adenovirus, called adenovirus 26 (Ad26) to deliver its antigen payload into cells. Prior to the COVID-19 pandemic, the company was already using this approach to develop vaccines for HIV, Zika, Ebola and respiratory syncytial virus (RSV). However, Ad26 is another common virus, so vaccines based on this approach have the same challenge to overcome: approximately 40–70% of adults in Kenya, South Africa, Thailand and Uganda are thought to have antibodies to it, although in Europe and North America it’s more like 10–20% of individuals.
Overcoming anti-vector immunity
Some experts think that delivering larger amounts of vaccine will overcome this problem. The level of antibodies in people’s blood might also be important; even though many people have been exposed to Ad26, Johnson & Johnson found no anti-vector immunity to their Ebola vaccine, which also uses Ad26.
Yet other companies are using adenoviruses from great apes to reduce this risk. For instance, the University of Oxford/AstraZeneca vaccine uses a chimpanzee adenovirus vector called ChAdOx1, while the Italian biotechnology company ReiThera has opted for an adenovirus that was originally isolated from gorilla faeces.