Everything you need to know about the latest weapon against cancer
mRNA-based vaccines are increasingly being used to help the immune system fight cancer.
- 2 September 2024
- 4 min read
- by Linda Geddes

An “off-the-shelf” mRNA vaccine has entered early-stage clinical trials in lung cancer patients.
Unlike personalised cancer vaccines, which teach the immune system to recognise unique antigens found on individuals’ cancer cells, BNT116 targets six proteins commonly associated with tumours in people with certain types of lung cancer.
Assuming they can be made to work, both approaches have the potential to revolutionise cancer treatment by enhancing the immune system’s ability to destroy cancer cells.
Although it is still early days, the hope is that such vaccines could provide the boost the immune system needs to eliminate cancer from the body, while leaving healthy cells untouched.
Cancer vaccines
Although our immune systems have a natural ability to detect abnormal cells, including cancer cells, these responses aren’t always strong enough to eliminate tumours from our bodies.
This is because cancer cells have evolved mechanisms to evade detection by the immune system and suppress immune responses.
Immunotherapies are a broad category of treatments designed to tweak the activity of immune cells and have become a standard treatment for certain types of cancer.
Cancer vaccines are a subtype of immunotherapy, based on the same underpinning principle as vaccines against infectious disease. The idea is that by showing the immune system what an invading pathogen or cancer cell looks like, you can teach it to quickly recognise and destroy them if it encounters them again.
In both cases, this is achieved by exposing immune cells to antigens – harmless fragments of the pathogen or cancer cell – which stimulate an immune response.
There are two main types of cancer vaccine, some of which are already approved for use in patients:
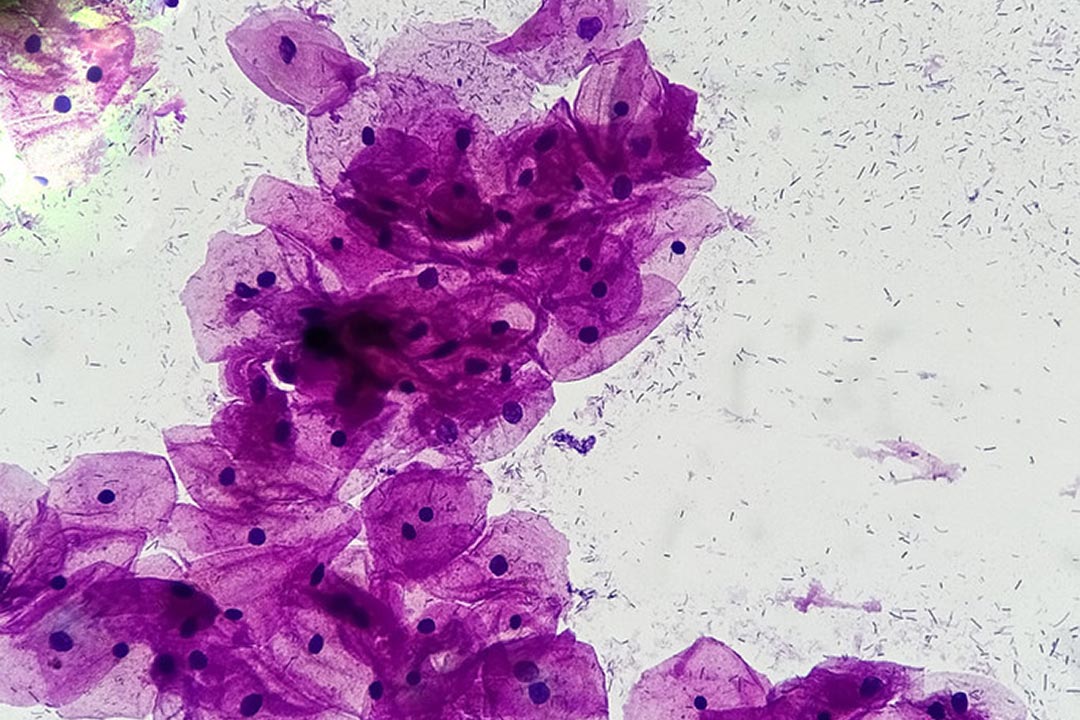
- Preventive cancer vaccines are designed to stop cancers from developing in the first place. These usually work by training the immune system to recognise and destroy cancer-causing viruses, such as the human papillomavirus (HPV) that causes cervical cancer and the hepatitis B virus that causes liver cancer.
- Therapeutic cancer vaccines target tumours that have already developed, with the goal or shrinking them or causing them to disappear. They could also be used to mop up residual cancer cells left behind after surgery and/or reduce the risk of the disease coming back. Although one such vaccine, called sipuleucel-T (Provenge), has been approved by US regulators, most therapeutic cancer vaccines are still being tested in clinical trials.
mRNA-based vaccines
Researchers are exploring the use of various platforms to develop cancer vaccines. These include whole cell vaccines, which use whole cancer cells to trigger an immune response, and protein- or peptide-based vaccines, which expose the immune system to specific proteins or fragments of proteins from cancer cells.
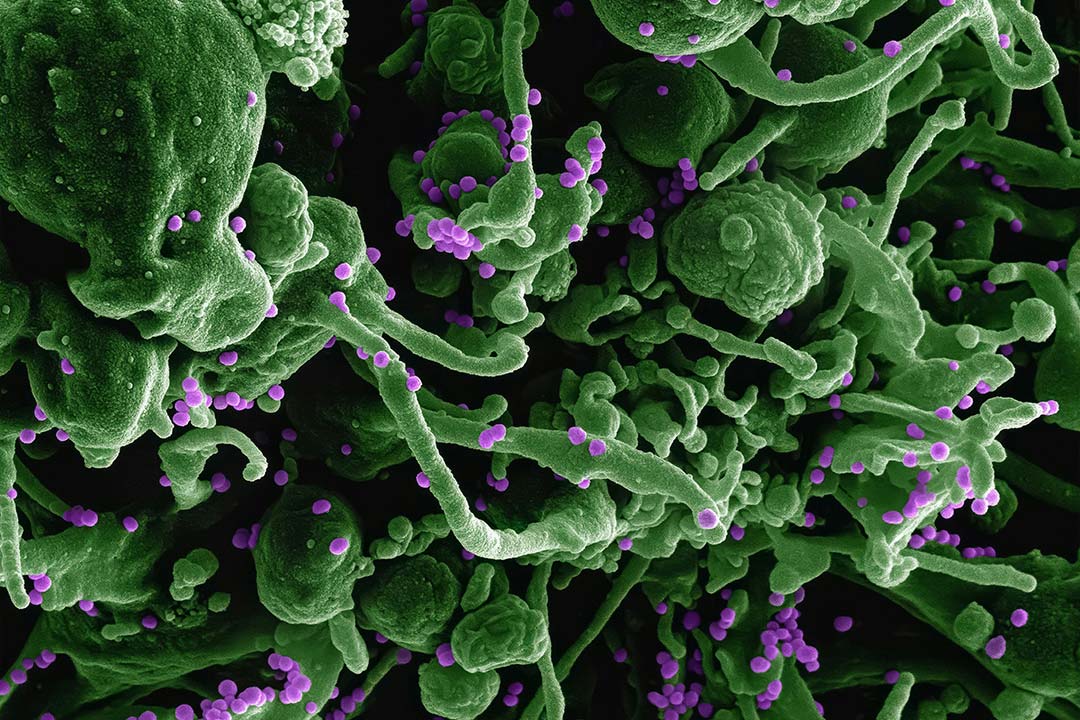
Another promising approach is the use of messenger RNA (mRNA), like the mRNA-based vaccines used to protect against COVID-19, except that rather than providing our cells with the molecular instructions for making fragments of viral protein, mRNA-based cancer vaccines instruct our cells to make harmless fragments of cancer-related proteins instead.
These capture the attention of immune cells, helping them to identify and destroy cancer cells that are also expressing these proteins.
Numerous mRNA-based cancer vaccines are currently in clinical trials for various types of cancer.
In most cases, these vaccines contain mRNA molecules tailored to individual patients. These are made by taking a biopsy of their tumour, genetically sequencing it to identify mutated proteins that may be driving its growth and are likely to stimulate an immune response, and then creating mRNA molecules that will provide the instructions for making these mutant proteins.
One such vaccine for the skin cancer melanoma is currently being tested in late-stage clinical trials. However, creating bespoke cancer vaccines is relatively expensive and time-consuming, potentially limiting their use.
Lung cancer vaccine
The BNT116 vaccine, which has just entered human trials at 34 research sites across the UK, US, Germany, Hungary, Poland, Spain, and Turkey, uses a slightly different approach.
It contains mRNA molecules for six antigens that are commonly expressed in cancer cells in patients with non-small cell lung cancer – one of two main types of lung cancer.
Have you read?
If successful, this could be a more practical way to give the vaccine to many more patients, because it doesn’t involve tailoring a vaccine to each individual patient. However, there is a risk that this may not work as well as a personalised cancer vaccine.
The trial will involve giving the vaccine to 130 lung cancer patients with different stages of disease, alongside a separate immunotherapy treatment, to determine whether BNT116 is safe and well-tolerated.
Although it is still early days, the hope is that such vaccines could provide the boost the immune system needs to eliminate cancer from the body, while leaving healthy cells untouched.