The groundbreaking history of the world’s first malaria vaccine
Malaria occupies a unique place in human history. Our neolithic ancestors were afflicted by it; the fall of Rome has even been partially attributed to it. During the 20th Century alone, malaria is estimated to accounted for up to five percent of all human deaths. In this context, thirty years is a metaphorical blink of an eye. But for the researchers who have poured more than half of their careers into developing the world’s first vaccine against malaria it has felt like an eternity.
- 3 December 2021
- 10 min read
- by Linda Geddes

Now rolling out to a first generation of children, the malaria vaccine is set to usher in a new chapter in humanity's centuries-long fight against Plasmodium falciparum, the deadliest strain of the parasite. So, how did the vaccine come about, and are there lessons that could be applied to other vaccines in the future?
“I almost get emotional again when I when I think about it. It was the first time that a vaccine against a human parasite [managed] to reach that level of protection, so it was very exciting.”
Malaria is caused by Plasmodium parasites, which are spread to people through the bites of infected female Anopheles mosquitoes. The first symptoms usually appear within 15 days and, if malaria is treated promptly, most people make a full recovery. However, because these early symptoms – headache, fever and chills – may be mild or confused with other illnesses, people often aren’t diagnosed with malaria until it is too late. Left untreated, P. falciparum malaria can progress to severe illness and death within 24 hours.
According to the WHO, there were roughly 229 million cases of malaria globally in 2019 and 409,000 deaths, with children aged under 5 years accounting for two thirds of these fatalities. Most of these deaths happen in sub-Saharan Africa. P. falciparum is the predominant species, responsible for more than 90% of malaria deaths, but there are four additional species, of which P. vivax poses the greatest threat. It is the dominant species in most countries outside Africa.
Vaccines vs parasites
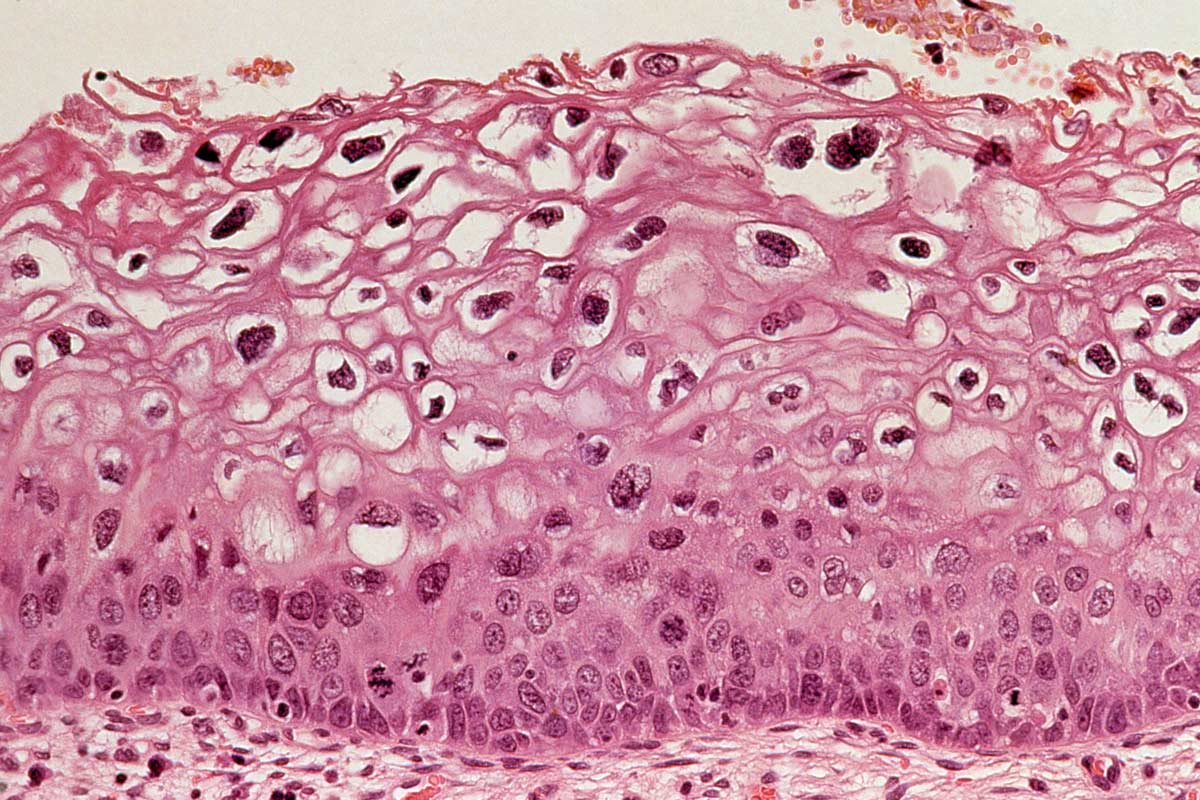
Although the link between Plasmodium parasites and malaria was made in 1880, developing an effective vaccine against them has proved extremely tricky. Vaccines work by training the immune system to recognise antigens associated with infectious agents – frequently proteins found on their surface. The malaria parasite also possesses such proteins, but targeting them is complicated by the parasite’s multi-stage life cycle and its active efforts to avoid detection by the immune system.
“Parasites in general, are very complex organisms, and the malaria parasite is no exception,” said Yannick Vanloubbeeck, head of discovery and preclinical R&D at GSK’s vaccines R&D centre in Belgium. “The big challenge is that the parasite actually changes its structure and the proteins it exposes on its surface to escape the immune system.”
When an Anopheles mosquito feeds on the blood of an infected person, blood stage forms of the parasite, called “gametocytes”, enter the mosquito’s gut and begin to reproduce. After 10-18 days of growth, their “sporozoite” offspring migrate to the mosquito’s salivary glands and, when the mosquito next bites a human, these sporozoites are injected into that person’s blood.
From here, the sporozoites migrate to the liver, where they multiply inside liver cells and mature into “merozoites”. These leave the liver and infect red blood cells, where they continue to grow and multiply, destroying the red cells, and then infecting others in a cyclical process. It is these blood stage merozoites that cause the symptoms of malaria. Some of them eventually develop into gametocytes, and when another mosquito bites that individual, the whole cycle begins again.
The early days of development
During the 1980s, scientists at the Walter Reed Army Institute of Research (WRAIR) in the US teamed up with scientists from SmithKleine and French, the predecessor to GSK, to try to develop a protein subunit vaccine against the sporozoite form of the parasite.
“If you can prevent the sporozoite from reaching the liver, then the rest of the cycle doesn't happen,” Vanloubbeeck explained.
The idea was to try to train the immune system against a sporozoite surface protein called circumsporozoite protein (CSP). Others had previously tried to do this and failed. A key problem is that sporozoites only exist in the blood for about 30 minutes before invading liver cells, so the immune system only has a short window in which to act. However, a GSK researcher, Joe Cohen, came up with the idea of boosting the immune response to CSP, by making immune cells think it was part of a virus, by using a hepatitis B virus surface protein (HBsAg) as a scaffold to display CSP as a virus-like particle.
This molecular sleight of hand helped, but it still wasn’t enough: “They were able to induce some immune responses, but were not able to show that [the vaccine] was providing protection,” said Lode Schuerman, medical affairs director for global vaccines at GSK. So, the research team went back to the drawing board, and experimented with different combinations of adjuvants – ingredients that boost the immune response to the antigen in various ways.
Have you read?
The breakthrough
A major breakthrough was the development of a human challenge model by WRAIR – a means of safely infecting humans with the pathogen of interest (P. falciparum), to rapidly identify which of numerous vaccine candidates induced the greatest degree of protection against it. This involved raising a colony of Anopheles mosquitoes, and feeding them on blood infected with P. falciparum parasites, which were known to be sensitive to commonly used anti-malaria drugs. Volunteers were then divided into different groups, each injected with a different vaccine candidate.
Once the vaccines had been given time to take effect, these volunteers allowed themselves to be bitten by the infected mosquitoes. As soon as an infection was detected – an indication that the vaccine hadn’t been effective – the volunteers were given antimalarial drugs to stop them becoming seriously unwell.
In 1997, the team identified an adjuvant formulation which, when combined with the CSP-HBsAg construct, was highly protective against malaria. The next step was larger human trials: first in adults, and then in teenagers, children and infants in those sub-Saharan African countries most affected by malaria.
A new model for vaccine development
However, there was another obstacle to overcome. Unlike other major infectious killers that vaccines have successfully been developed against, malaria is primarily a disease of the Global South. This means the typical model of spreading the risks and recuperating the costs of vaccine R&D by charging wealthier countries more for a vaccine once it is finally approved wouldn’t work. A whole new model for vaccine development had to be developed – one that involved external partners, such as The Bill and Melinda Gates Foundation, WHO and the nonprofit global health organisation PATH, from the outset.
“It was about having a joint, integrated end-to-end plan, aligned across key partners, from very early on, so that we could look together for the best solutions,” said An Vermeersch, vice president, head of vaccines global health access at GSK Vaccines. “I think the level of collaboration we had on this was unique.”
She added that a similar model might be applied to the development of vaccines against other diseases in the future. “There are a lot of lessons about the need for early alignment with critical partners, not only on the clinical plan [for vaccine trials], but on the registration and manufacturing phases, and looking for funding solutions – all of those elements. It is clear that it needs to be done together,” Vermeersch said.
The vaccine trials
Another milestone came in 2004, when the results of a double-blind, randomised controlled trial in young children in Mozambique, provided the first indications that the RTS,S vaccine was safe, well-tolerated, and helped to prevent malaria in this age group.
More trials followed, until, in 2015, the results of a large phase 3 trial conducted in more than seven African countries showed that three doses of RTS,S/AS01e, administered with a one-month interval, and followed by a booster dose 18 months later, helped to protect children and infants from clinical malaria for at least three years after the first vaccination. Among children who were aged 5-17 months at first vaccination, the number of clinical malaria cases was reduced by 39% up to the end of the study (the average follow-up was four years), while for those who were aged 6-12 weeks when they received the first vaccine dose, clinical malaria cases were reduced by 27%. More cases were averted in areas of higher malaria transmission.
“I almost get emotional again when I when I think about it,” said Schuerman. “It was the first time that a vaccine against a human parasite [managed] to reach that level of protection, so it was very exciting.”
The potential impact
Compared to the efficacy of the current COVID-19 vaccines, say, 39% may not sound like a lot, but weighed against the huge global burden of malaria it constituted a massive reduction in cases.
Schuerman said: “People sometimes think that if you don't reach 80 or 90% efficacy, it is not a good vaccine. But first of all, there is no other vaccine – this is the first against malaria. And there are so many cases of malaria, so if you can prevent [close to] half of them, that’s huge.”
For instance, one modelling study suggested that the vaccine it could prevent the deaths of 23,000 children a year, if all of those in high incidence countries received the full series of doses.
“Ultimately, what we want is 80 or 90% efficacy and something that lasts for many years, but this is a very difficult target, and I think we focus too much on the percent efficacy,” said Ashley J. Birkett, head of malaria vaccine development at PATH. “With malaria, it's such a highly prevalent disease, where children can be getting sick over and over again, many times throughout the year. So actually, a 30% reduction translates into a very large number of cases averted. In one of the clinical centres involved in the phase 3 trial, we saw over 6,000 cases of malaria prevented for every 1,000 children who were vaccinated.”
Also, the vaccine isn’t designed to be used in isolation, but alongside other malaria prevention tools, such as insecticide-treated bed nets, insecticide spraying, or seasonal malaria chemoprevention (SMC) – the intermittent administration of antimalarial medicine during the malaria season to prevent illness. “We've shown that if you layer partially efficacious tools against malaria effectively, you can translate that into very high impact,” Birkett said. For instance, a recent trial in Burkina Faso and Mali suggested that combining the RTS,S/AS01e vaccine with SMC lowered clinical episodes of malaria, hospital admissions and deaths by about 70%, compared to SMC alone.
“Our work has shown a combination approach using a malaria vaccine seasonally – similar to how countries use influenza vaccine – has the potential to save millions of young lives in the African Sahel,” said study leader Daniel Chandramohan from the London School of Hygiene and Tropical Medicine. “Further research is now needed to examine how seasonal malaria vaccination could be delivered most effectively at scale.”
The pilots
Following the publication of those trial results in 2015, the WHO requested that vaccine rollout be piloted in three to five African countries, to assess the feasibility of delivering four doses to children alongside existing vaccine programmes and to gather additional real-world safety and efficacy data. These pilot programmes were launched in Ghana, Kenya and Malawi in 2019, with more than 830,000 children vaccinated so far. The first results showed that hospitalisations from severe malaria have decreased by about 30%. The vaccine has also increased access to malaria prevention, reaching more than two thirds of children not protected by an insecticide-treated net. In areas where nets were already being used, vaccination hasn’t reduced their use.
Combined with the clinical trial results, it was this data that gave the WHO the confidence to make its recent recommendation.
A silver bullet it is not, but other malaria vaccines are likely to follow in the coming years. Birkett said: “A lot of people ask me ‘can this vaccine be used for elimination of malaria?’ For elimination, we're probably going to need a vaccine that works across all age groups, possibly with high levels of efficacy as well. So, this is really a tool targeted to younger children.”
However, layered alongside other malaria prevention methods, RTS,S/AS01e could still make a major dent in the annual disease toll from malaria – particularly during those critical first five years of life, when children are at the greatest risk of death. That alone is surely enough to earn it a place in the history books.