How Kerala curtailed the Nipah virus
September’s outbreak of the killer bat-borne infection – India’s sixth - began and ended in just a week. VaccinesWork takes a deep dive into what Kerala got right.
- 17 November 2023
- 8 min read
- by T V Padma

When Kerala, a state in south India, recently found itself confronting the deadly bat-borne Nipah virus for the fourth time in five years, it had its operation manual at the ready, and managed to contain the infection within just a week.
Outbreak
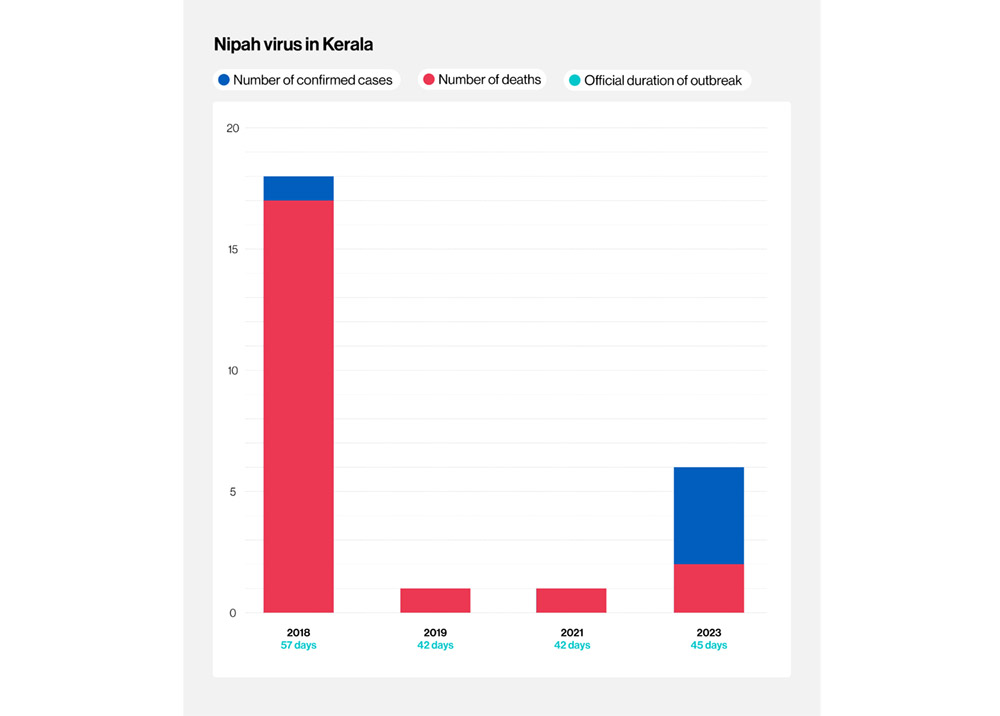
India has faced six Nipah outbreaks since 2001. The most recent four have taken place in Kerala, and all since May 2018. September's outbreak saw the state press its experience of the virus into service.
“The trainings and experience of COVID-19 improved the system.”
– Lathika Arun, district surveillance officer
On 9 September 2023, a case of suspected Nipah was reported in Kozhikode district. Samples were sent to the National Institute of Virology (NIV), Pune, India's apex reference laboratory for major virus outbreaks, for confirmation.
By the 15 September , India's Ministry of Health had reported six laboratory-confirmed Nipah virus cases, including two deaths, in the same district, the World Health Organization stated.
Containment action
Kerala sounded an alert immediately after it detected its first case. As infections spread, the state quarantined the affected areas in Kozhikode and issued alerts to neighbouring districts and states to intensify surveillance. The state government also declared containment zones in villages in the district, restricting movement, public gatherings, and making wearing of masks and social distancing mandatory in public spaces.
“Climate change causes stresses we don't fully understand,” says Jameel. “Stress is known to increase virus shedding in many animal species – be it herpes in humans or Nipah in bats.”
– Shahid Jameel, virologist
On 14 September, the district administration shut down schools for a week as a precautionary measure and switched to online classes.
Teams of officials from the central and state health ministry and the NIV, along with mobile diagnostic units, equipped with a point-of-care micro polymerase chain reaction (PCR) assay that multiplies gene sequences, and enzyme linked immune sorbent assay (ELISA) to detect antibodies in blood, fanned out to Kozhikode. Rapid diagnosis enabled quicker health system reflexes.
WHO reported that, "As of 27 September 2023, 1,288 contacts of the confirmed cases were traced, including high-risk contacts and healthcare workers." High-risk contacts would remain under quarantine and monitoring for 21 days. .
End zone
With the maximum incubation period reported for similar Nipah virus strains circulating in Kerala found to be 17 days, Kerala's standard operating procedure allowed for a potential incubation period of 21 days. If no new cases were reported during a 42-day period, the outbreak would be considered over.
14 September saw the final case notified. Accordingly, the outbreak was declared finished on 26 October 2023.
Public know-how
It helped containment efforts that people from Kozhikode were practised at social restrictions following the COVID-19 pandemic. "The trainings and experience of COVID-19 improved the system," says Lathika Arun, district surveillance officer. People were familiar with use of masks and sanitisers, with social distancing and the frequent washing of hands with soap. Field-level workers were well trained on contact tracing and the importance of isolation, says Arun.
And Nipah was no stranger, by 2023. "Not only the system, but the people also learnt from recurrent outbreaks of Nipah," says TS Anish, professor at the Department of Community Medicine at the Government Medical College, Manjeri, Kerala. "They avoid fruits bitten by bats and other instances of contact with the animals."
The Kerala model of disease control
The key elements in Kerala's public health response were good coordination between the central and state health authorities, agile house-to-house surveillance and contact testing on the ground, efficient laboratory testing, quick preparation of health facilities for isolation centres, and efficient management of the dead bodies, says WHO.
According to Anish, it's important that the state's health system is sensitive: capable of detecting clustering of encephalitis or acute respiratory distress syndrome, two typical symptoms of Nipah infection, even in 'single-case clusters' – meaning outbreaks that involve just a single patient.
"As the system starts working in the early phase of the outbreak, patients are captured early and the best care is provided," says Anish. "This might have contributed to the low case fatality [rate] this time."
Kerala has efficient locally-available testing facilities, a standard operating procedure for control in place with experience gained from previous outbreaks, strong political leadership and coordination of various departments, as well as decentralisation of all activities to local administration and health units.
That means that a district with Nipah cases can act fast, rather than waiting for approval from state HQ in Thiruvananthapuram. A study on Kerala's handling of the three prior Nipah outbreaks and COVID-19, published in March in the journal Public Health Action, found that this decentralised agility was crucial to its successes.
Other contributors to Kerala's success at containing the virus rapidly, according to Anish, included public awareness campaigns run by local administrations, and the training of community health workers to detect any unusual events occurring in their vicinity.
Have you read?
Based on previous outbreaks, medical experts identified 19 core areas to be focused on, and set up 19 committees to manage those areas on day one. Those committees reported to daily review meetings.
The state also set up screening facilities and, in 2019, a new virology institute to study emerging threats. While there were none during the first outbreak of Nipah in Kerala, the state now has at least four biosafety level 2 (BSL-2) laboratories with a BSL-3 facility to extract the virus.
Growing with experience
During the 2018 outbreak, the health system was inexpert at dealing with infections that spread rapidly and can be fatal, says Arun. Hospital infection control measures were "also not up to the mark".
The state has since mastered the entire chain of operations: route mapping, tracing of possible contacts, listing contacts and quarantining them to watch for any symptoms, transporting the symptomatic cases in designated ambulance vans, and setting up isolation facilities.
Kerala has a public health system that works well at the primary level, has prior experience of Nipah and is able to spot it more easily now than earlier. Similar situations elsewhere may go unnoticed and uninvestigated.”
– Shahid Jameel, virologist
"[Our] results highlight the importance of human resources and service delivery as balancing factors during public health threats in any developing nation with limited resources," reported the team of scientists behind the Public Health Action study in March 2023.
Another group that analysed the 2019 outbreak reported that "the major enablers for [Kerala's] apt response were identified to be effective communication, good line of control, effective division of work, intersectoral coordination, strong leadership, political commitment, resilient public private partnership and support groups, past experiences in disaster management, quick procurement of medicines and availability of lab facilities."
Climate risk?
One of India's top virologists, Shahid Jameel, recommends that bats from different areas in India are sampled to see what viruses they harbour, as Nipah is borne and spread by bats. "The geography of the outbreak suggests that bats in the Khozikode area carry the virus," he says, explaining that Nipah's seasonality could be linked to ripening of date palm fruit, which bats lick at night and which is also consumed by humans. Several factors such as climate change-induced stress and deforestation could contribute to the recent increased frequency of outbreaks.
"Climate change causes stresses we don't fully understand," says Jameel. "Stress is known to increase virus shedding in many animal species – be it herpes in humans or Nipah in bats." Deforestation brings animal species out of their natural forest habitats, and closer to human habitations, causing fruit-eating species to dine on trees that are also accessed by people.
A robust response that includes a system that quickly detects spillovers holds the key, says Anish. Nipah is caused by an mRNA virus prone to rapid mutations that can change the entire spread of the disease. This increases its potential to cause bigger future outbreaks or even a pandemic, he cautions. The fatality rate of Nipah is high: 60–90% for the variant found in Kerala, says Anish.
The average case fatality rate of Nipah "is on the relatively lower side (around 40%)" for the strains responsible for outbreaks in Malaysia during 1990s. "It is on the higher side (around 75%) for the strain responsible for the outbreak in Bangladesh and West Bengal during the early years of 2000," he explains. In Kerala, the circulating strain was closer to the Bangladesh strain in terms of deadliness – around 90% in 2018, he says.
"But, [this time] we could save more people," he adds. Four out of six patients in the recent outbreak survived, "maybe because the system was able to pick [up] cases early and [they] could be treated with available antiviral drugs and supportive care".
“Every spill-over is a ‘test run’ for the virus to check the effectiveness of already acquired mutations that may end up in more efficient human spread,” says Anish, “so prevention of spill-overs is very important.”
– Anish TS, professor, Department of Community Medicine, Government Medical College, Manjeri, Kerala
Kerala has a public health system that works well at the primary level, has prior experience of Nipah and is able to spot it more easily now than earlier, says Jameel. "Similar situations elsewhere may go unnoticed and uninvestigated."
Scanning the horizon
Other challenges include the huge reservoir of the virus in Asia, imprecise knowledge of the burden and regional distribution of infected bats, and insufficient evidence on the potential intermediate hosts or mechanisms that can hand over the infection to humans, he adds.
"Every spill-over is a 'test run' for the virus to check the effectiveness of already acquired mutations that may end up in more efficient human spread," says Anish, "so prevention of spill-overs is very important."
Anish warns of two factors that could contribute to bigger future outbreaks. One is the
possible presence or future emergence of an intermediate host, which would magnify chances of human infections because of their closer interactions. "The intermediate host can act as a substrate for viral mutations, and the epidemic can become propagated in nature." He cites the example of 1996–1998 outbreak in Malaysia, which saw a prolonged period of risk for human infections from infected pigs.
A second is that often the system may not recognise a Nipah outbreak, because the clusters are typically small in number and often limited to single cases.
But in future, there could be more spill-overs in such areas, because the local community does not perceive the risk, and these areas "could act as a good field for the virus to mutate" and could be "the cradle for new pandemics." Those future pandemics could be devastatingly deadly, if not dealt with swiftly.









