The long tail: Post-Polio Syndrome
Decades after recovering from polio, some survivors are developing progressive muscle weakness and fatigue that can severely impair their quality of life.
- 15 August 2022
- 4 min read
- by Linda Geddes

For much of the 20th century, parents feared the onset of the warmer months, and the outbreaks of polio they would often bring. Even as recently as 1988, the disease was still present in 125 countries and paralysed nearly 1,000 children per day. Those who recovered counted themselves lucky, but even then, many endured years of painful rehabilitation to regain the use of their arms and legs. Although global vaccination efforts have reduced the incidence of polio by more than 99%, as those survivors progress through adulthood, a significant proportion of them are now developing a host of new neurological symptoms known as Post-Polio Syndrome (PPS).
Depending on how it is diagnosed, PPS is estimated to affect between 20% and 85% of polio survivors.
Characterised by new, gradual and progressive muscle weakness and wasting, difficulty swallowing, joint or muscle pain, and general fatigue after being stable for many years, PPS typically develops 15 to 40 years after people have recovered from polio. Although it is not contagious, it can still have a considerable impact on people’s quality of life.
History of Post-Polio Syndrome
The first medical reports of PPS appeared in France in 1875. Doctors described four young men – all working in physically demanding jobs – who had experienced polio-related paralysis during infancy, recovered, and subsequently developed new weakness in previously affected and unaffected muscles.
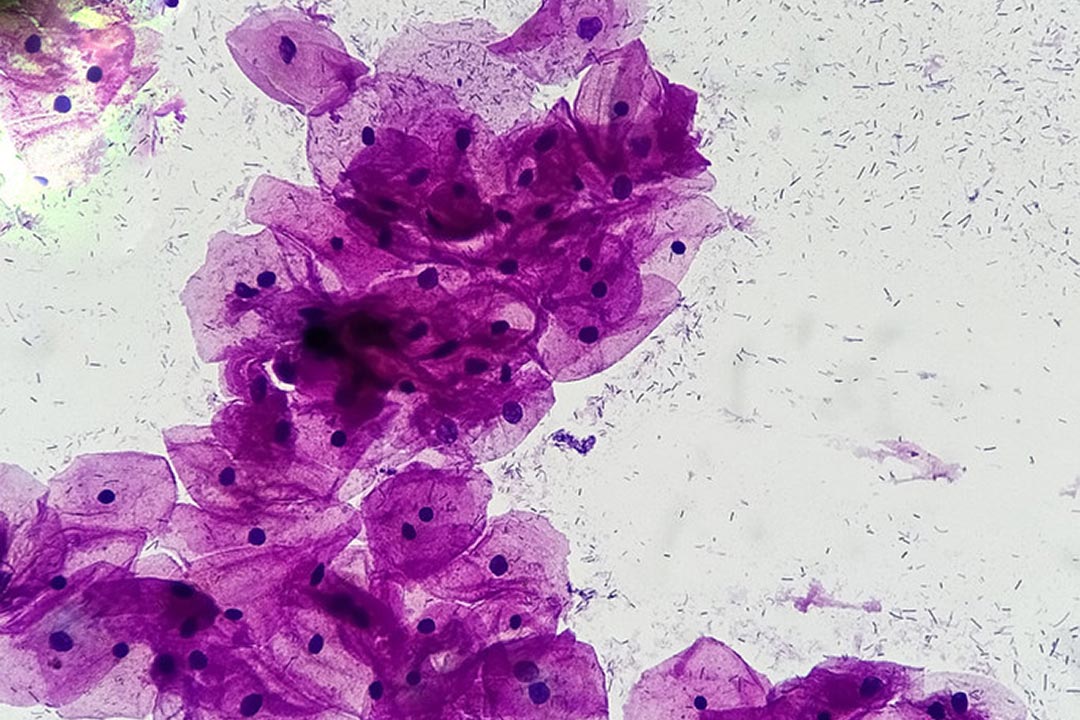
Further research in the 1950s identified significant damage to nerve cells within the spinal cord. However, as the UK-based Polio Survivors Network points out, there is no set pattern of nerve damage: “Damage to the nerves from the virus varies in level and area(s) of the body. Dr Marinos Dalakas [a neurologist at Thomas Jefferson University Hospital in Philadelphia, US] likened it to standing polio survivors in front of a white sheet, throwing a bucket of black paint at them, and at the same time hitting a wind machine with millions of settings, a different one for each person. The poliovirus having no set pattern of damage to the body makes it much more challenging for health professionals."
Have you read?
Prevalence and symptoms
Not everyone experiences severe symptoms; in some individuals, they may be mild, whereas in others they may significantly impair that person’s ability to live independently. Weakness in the neck, chest or diaphragm muscles, for example, can result in problems breathing or swallowing, which can in turn impact people’s sleep and daytime functions, or result in food or liquids accidentally being inhaled into the lungs, leading to pneumonia.
Depending on how it is diagnosed, PPS is estimated to affect between 20% and 85% of polio survivors. Because of the time lag between catching the disease and developing these later complications, PPS is likely to continue blighting people’s lives for at least several more decades, despite the huge progress that has been made in eliminating polio from most regions of the world.
Potential causes
Precisely what causes PPS is unknown. If poliovirus gets into the blood during the initial infection, it often attacks nerve cells in the brainstem and spinal cord. Those cells that survive may subsequently sprout new projections that reconnect with muscle fibres and restore some degree of power and movement to affected limbs. However, one theory is that, because these connections are weaker than the originals, and some residual damage to the nerves remains, years of accumulated stress can gradually cause them to deteriorate, resulting in muscle weakness. Brain scans have also identified damage to cells in the brainstem that control alertness in some patients, which may contribute to fatigue, but poor-quality sleep, or reduced physical fitness as a result of muscle weakness, may also play a role.
Treatment
Although there’s currently no drug or procedure to reverse nerve damage or prevent further deterioration, various strategies exist to help people manage their symptoms. These include avoiding activities that cause pain and/or fatigue that lasts more than ten minutes, and pacing yourself in daily activities, routinely stopping to take 15- to 30-minute rests. Mobility and breathing aids can also help to reduce muscle tiring and exhaustion.
Some patients benefit from light exercise to improve cardiovascular fitness, but this should only be done under close medical supervision, and needs to be carefully monitored to ensure it doesn’t contribute to further weakness or fatigue.