Vaccine profiles: Pneumococcus
Pneumococcal vaccines have substantially reduced deaths from pneumonia and meningitis, but they don’t protect against all bacterial strains, and antibiotic resistance is a growing threat.
- 16 May 2023
- 8 min read
- by Linda Geddes
At the beginning of the 20th Century, South African administrators embarked on a mission to revitalise the country's economy following the Second Boer War. This included returning the country's gold mines to profitability. To achieve this, mine owners began recruiting labourers from beyond South Africa's borders to work in hazardous and unhealthy conditions underground.
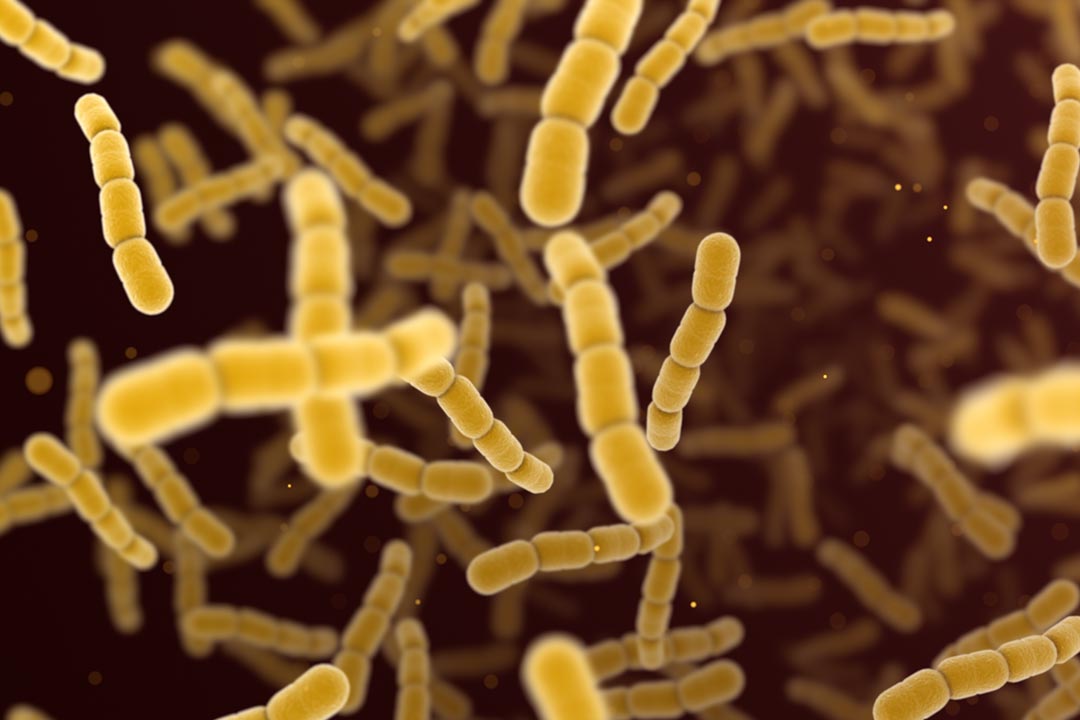
Since miners often arrived in poor health, and were housed in crowded barracks, infections such as influenza and pneumonia quickly spread, killing up to one in ten miners each year. The biggest killer of all was pneumococcal pneumonia, which is caused by Streptococcus pneumoniae (pneumococcus) bacteria. Within the first four months of working in the mines 1–2% of men had been infected with it, and, among men proven to be infected, 25–56% of them died.
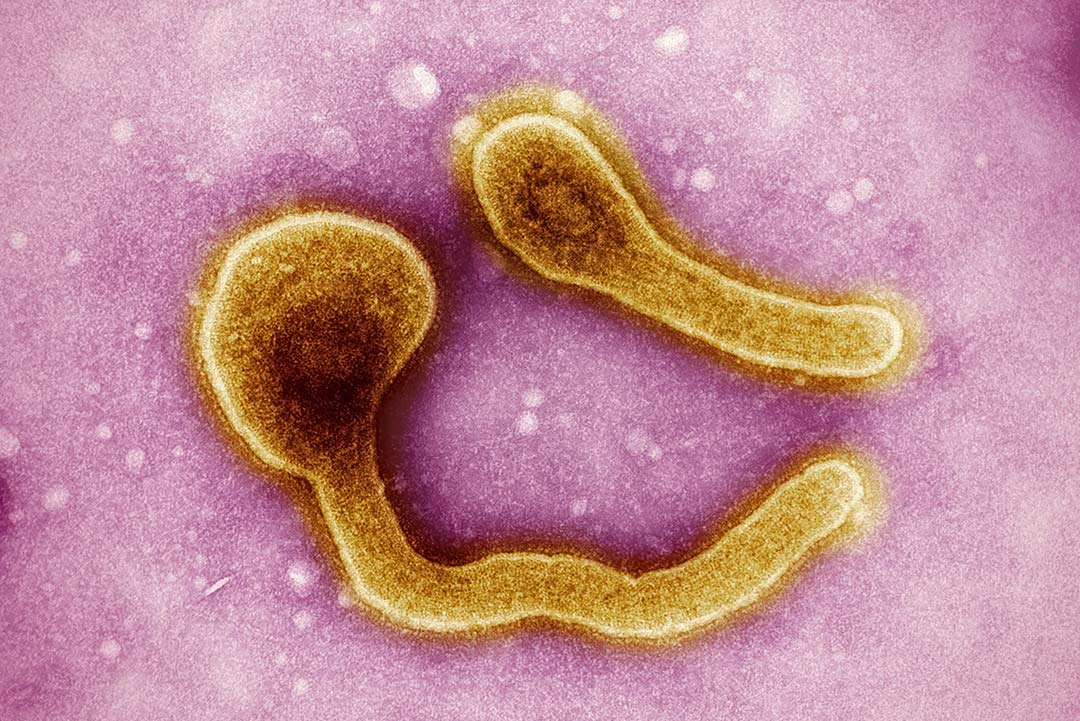
Pneumococcus bacteria continues to be the leading cause of severe pneumonia and bacterial meningitis worldwide. Pneumonia kills some 740,000 children under the age of five each year, making it the single largest infectious cause of death in children.
They weren't alone. A whole century later, pneumococcus bacteria continues to be the leading cause of severe pneumonia and bacterial meningitis worldwide. Pneumonia kills some 740,000 children under the age of five each year, making it the single largest infectious cause of death in children.
The introduction of pneumococcal conjugate vaccines (PCVs) has substantially reduced the burden of death and disease, but millions of children remain unvaccinated, and existing vaccines don't protect against all pneumococcus strains. Also, although antibiotics can successfully treat the illness, antimicrobial resistance (AMR) is a growing problem.
Pneumococcal disease
Pneumococcus bacteria can cause infections in various parts of the body, including the ears (otitis), sinuses (sinusitis), lungs (pneumonia) blood (bacteraemia) or the lining of the brain and spinal cord (meningitis).
There are at least 90 different types, and they are transmitted by direct contact with respiratory droplets when infected people cough or sneeze. The risk of infection varies by season. In temperate climates, rates of pneumococcal disease peak during colder months, while in areas with wet and dry seasons, they are higher during the drier months.
Symptoms depend on which body part is affected, but those with pneumonia may have a cough, fever, chest pain and breathing problems. Meningitis symptoms include fever, a stiff neck, light sensitivity, headache and confusion, while bacteraemia is associated with fever, chills and low alertness. Older adults and young children are at greatest risk of severe illness, particularly if they have other conditions such as chronic heart, lung or kidney disease.
Of the estimated 5.83 million deaths that occurred among children aged under five years in 2015, some 294,000 of these deaths were caused by pneumococcal infections – the majority occurring in Africa and Asia. Case fatality rates for children with severe and invasive pneumococcal infections, such as bacteraemia or meningitis, range from 20–50% in low- and middle-income countries.
However, pneumococcal pneumonia is deadly no matter where in the world you live. In the US, pneumococcal pneumonia kills about one in 20; while pneumococcal meningitis kills around one in 12 children and one in six older adults. Those who recover may experience longer-term problems, such as hearing loss or developmental delay. Pneumococcal bacteraemia kills about one in 30 children and one in eight adults in the US, and survivors may lose infected limbs.
Early vaccines
Efforts to create a vaccine against pneumococcus began in 1911, when South African mining representatives approached a British doctor called Almroth Wright, who had previously worked on a vaccine against typhoid fever.
Wright adopted a similar approach against pneumococcus: injecting whole heat-killed bacteria into thousands of migrant labourers who were working in gold mines near Johannesburg. The results of these initial vaccine trials were encouraging – suggesting a substantial reduction in pneumonia cases and deaths after inoculation.
However, it soon became clear that pneumococcus wasn't a single enemy, but that there were multiple 'serotypes' – groups within a species of microorganism that share distinctive surface structures. Once researchers had figured out how to identify them, they set about combining these whole killed bacteria into multivalent vaccines to protect against more than one pneumococcus serotype.
Polysaccharide vaccines
During the 1930s and '40s, researchers began to test polysaccharide-based pneumococcal vaccines (PPVs), derived from the polysaccharide "capsule" that pneumococcus wears as a kind of coat. This capsule varies between serotypes, and researchers discovered it was a key part of the bacterium that people's immune systems were responding to following inoculation.
However, with the discovery of penicillin, interest in pneumococcal vaccines waned and their development stalled. The assumption was that doctors could simply treat pneumococcus infections with these antibiotics but, although penicillin reduced pneumococcus deaths, it did not eliminate them – particularly deaths occurring during the first 96 hours of antibiotic therapy.
Have you read?
In 1977, Merck licensed a PPV vaccine containing capsular polysaccharides from 14 strains of pneumococcus, followed in 1983 by one containing 23 capsular polysaccharides – Pneumovax – which is still in use today. According to a meta-analysis published in 2008, which combined the results of multiple trials, PPVs reduced the incidence of all invasive pneumococcal disease in adults worldwide by 82%.
However, PPV vaccines are largely ineffective in children younger than two years old, who are the highest risk group for pneumococcal disease – presumably due to their immature immune systems.
Conjugated vaccines
To overcome this problem, scientists needed to find a way to boost the immune response. So, they began chemically attaching these capsular polysaccharides to an inactivated form of the diphtheria toxin, called a toxoid, which the immune system easily recognises.
A key moment came in 2000, with the publication of a clinical trial that evaluated the first of these pneumococcal conjugate vaccines (PCVs) – which was designed to protect against the seven most common pneumococcal strains – in 37,868 infants in Northern California. It found that the incidence of pneumococcal meningitis was reduced by more than 95% in infants who were fully vaccinated, and the efficacy against all pneumococcal invasive disease was greater than 97%. This vaccine, known as PCV7 or Prevnar7, was licensed in 2000.
However, pneumococcus was not so easily defeated. Effective as PCV7 was against the strains it covered, its routine use began to be associated with an increasing incidence of disease caused by a different strain, called serotype 19A – a phenomenon known as "serotype replacement". This highlighted the value of vaccinating against a broader range of strains. PCVs covering 10, 13 and 15 strains have since followed; in some of cases the polysaccharides are conjugated to diphtheria toxid; in others, to tetanus toxoid or protein D (an outer membrane protein from Haemophilus influenzae).
In 2021, PCVs providing protection against 15 and 20 pneumococcal strains were approved for adult use in the US, followed by European authorisation in late 2021/early 2022, while PCVs covering more than 20 strains are also in development.
Three PCVs are currently prequalified by the World Health Organization (WHO) for use in infants and children: PCV13, manufactured by Pfizer; and two PCV10 vaccines manufactured by GSK and the Serum Institute of India. Manufacturers are expected to seek WHO prequalification for PCVs, covering a broader range of strains in the future.
Extraordinary impact
WHO recommends the inclusion of PCVs in childhood immunisation programmes worldwide, and as of the end of 2020, 148 out of 194 WHO member states had introduced it – including 63 Gavi-eligible lower-income countries.
The incidence of pneumococcal meningitis was reduced by more than 95% in infants who were fully vaccinated, and the efficacy against all pneumococcal invasive disease was greater than 97%.
These childhood vaccination programmes have had an extraordinary impact on rates of pneumococcal disease in those countries that have introduced them. For instance, a 2017 study that investigated the impact of routine childhood vaccination in The Gambia found that it had reduced the incidence of invasive pneumococcal disease in children aged 2–59 months by around 55%, and of hospitalised pneumonia by 30%.
Routine childhood immunisation against pneumococcus has also reduced the burden of pneumococcal disease in older children and adults who haven't been vaccinated against it – presumably because there's less community transmission of strains that are covered by the vaccines.
Fewer countries have specific policies or programmes for vaccinating adults against pneumococcus. Those that do tend to be higher income countries and focus on adults over the age of 65 or those with a health condition that increases their risk of pneumococcal infection.
Four vaccines are currently available for the prevention of pneumococcal disease in adults: PCV13, PCV15, PCV20 and the polysaccharide-based pneumococcal vaccine, PPV23. If PCV13 or 15 are used, this is usually followed by a dose of PPV23, typically a year later. Adults who receive PV23 or PCV20 usually only need one dose.
Ongoing challenge
Although many countries have introduced routine childhood immunisation with PCV, not all have, with 80% of the 345 million children who have received no doses of PCV living in 25 countries. Nearly a third of these countries are Gavi-eligible, and four of them are planning to introduce PCV into their routine immunisation programmes in the coming years. A 2019 study estimated that nearly 400,000 of the 672,000 annual child deaths from pneumonia could be averted through pneumococcal vaccination, so continuing to support uptake is important.
The emergence of disease caused by non-vaccine pneumococcal strains is also an ongoing problem, and is prompting research into alternative types of vaccines, including next-generation protein-based vaccines, mRNA vaccines, or genetically modified pneumococcal whole cell vaccines.
The road to defeating pneumococcus has been a long one, and there's still a way to go, but through sustained efforts to increase vaccine uptake, and future innovations, many more lives could be saved.