Seven things you need to know about Nipah virus
India is racing to contain an outbreak of the deadly Nipah virus – but what is it, and how great a threat does it pose?
- 15 September 2023
- 6 min read
- by Linda Geddes

The south Indian state of Kerala is battling an outbreak of Nipah: a virus that comes from bats, but which has triggered multiple human outbreaks in recent decades. The World Health Organization (WHO) lists Nipah as one of its priority pathogens: those with high epidemic potential, and for which zero or insufficient countermeasures exist. The virus is also considered a bioterrorism threat.
Here's everything you need to know about Nipah virus and the risk it poses:
1. It is a relatively new virus
Nipah virus was first identified in the cerebrospinal fluid of a patient in Sungai Nipah, a village to the south of Kuala Lumpur, Malaysia, in March 1999. Tests revealed that this was a previously unknown type of paramyxovirus, belonging to the same family as measles, mumps, RSV and Hendra virus. It was named Nipah virus after the village where it was first identified.
The first way to prevent Nipah outbreaks is to minimise contact with bats. This means encouraging people to wash fruit and vegetables before consumption, to clean their hands after picking or preparing them and covering containers used to collect palm sap and boiling it before consumption.
The virus was subsequently linked to an ongoing outbreak of an encephalitis-like illness in different regions of Malaysia and among slaughterhouse workers in neighbouring Singapore. This outbreak had begun the previous September with a cluster of cases linked to pig farm workers in Northwest Malaysia, who were initially suspected of having Japanese encephalitis.
Typical symptoms included fever, headache and decreased consciousness, and infections were frequently deadly: in total, 265 people were infected and 105 died during the Malaysia outbreak, a fatality fate of 39.6%. Eleven people were infected in Singapore, one of whom died.
The outbreak ended in May 1999, following the slaughter of around a million pigs and a ban on pig exports to Singapore. Subsequent investigations revealed the primary host of the virus to be fruit bats; pigs are initially thought to have become infected because an orchard was planted near a pig farm, and secretions from bats roosting there contaminated the pigs' feed and water.
2. Outbreaks are becoming more common...
Since that initial outbreak, others have occurred in Bangladesh, India and the Philippines. Bangladesh experienced almost annual outbreaks between 2001 and 2013, most of which were linked to contact with fruit bats – especially drinking raw palm sap contaminated with bat urine or saliva – although some limited human-to-human transmission has occurred.
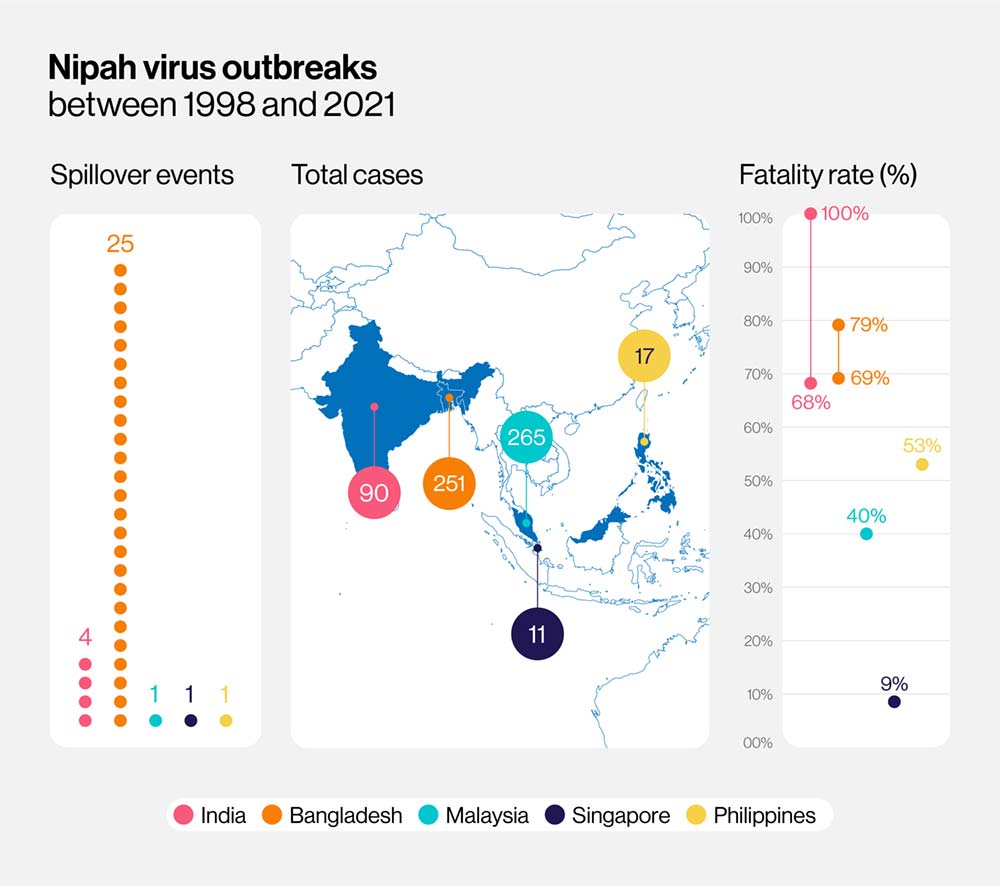
Before the current outbreak in India, a total 634 cases and 376 deaths had been recorded worldwide. While worrying, these are still relatively small numbers on a global scale.
3. ...And potentially more dangerous
Although there haven't been enough human cases of Nipah to say with certainty that the virus is becoming more deadly, the case fatality rate in recent outbreaks in Bangladesh and India is higher than reported in Malaysia and the Philippines. Also, whereas mortality during the first Bangladesh outbreak in 2001 was 69%, during the 2013 outbreak it was 83%, while an outbreak in Kerala, India in 2018 killed 17 out of the 18 people infected – a fatality rate of 94.4%.
Testing of bats has revealed the existence of at least two strains of Nipah virus, known as the Malaysia strain (which was also linked to the Philippines outbreak) and the Bangladesh strain (linked to outbreaks in Bangladesh and India). Human infections with the Malaysia strain appear to be a little less severe, with more subclinical cases (where people are infected with few obvious symptoms), and no sign of human-to-human transmission.
Have you read?
The Bangladesh strain is associated with additional symptoms, including muscle weakness, cough and breathing difficulties and can be transmitted directly between humans, through contact with body fluids and possibly respiratory droplets produced when people cough or sneeze. The 2018 outbreak in Kerala was associated with a further symptom: heart muscle dysfunction.
Nipah is an RNA virus and such viruses tend to have high rates of genetic mutations, making it easier for them to adapt to new hosts and change in response to challenges, for example from their hosts' immune systems. The Bangladesh strain is likely to be more infectious than the Malaysia strain, and it wouldn't be surprising if these strains mutated further, scientists have warned.
4. There are multiple opportunities for humans to become infected
While its usual hosts are fruit bats, Nipah can infect humans and other animals, primarily through eating or drinking products contaminated by bat urine, saliva or droppings. This is problematic because the trees the bats live in are often found near human settlements and include date palms and other fruit trees. Bat guano is sometimes used to fertilise agricultural fields, potentially putting farmers and agricultural workers into close contact with the virus. Humans can also contract Nipah from other animals that have been infected by bats, including pigs and horses; a 2014 outbreak in the Philippines was traced to contact with horses or consumption of horse meat.
5. Once infected, people can pass Nipah to other people
Studies on the spread of Nipah virus in Bangladesh have suggested that human-to-human transmission occurs through direct contact with patients and their body secretions, such as urine, blood, and nasal or respiratory droplets. Such infections have usually occurred in hospitals among healthcare staff, caregivers or visitors, although transmission within households is also believed to have occurred.
6. Outbreak control is possible
The first way to prevent Nipah outbreaks is to minimise contact with bats. This means encouraging people to wash fruit and vegetables before consumption, to clean their hands after picking or preparing them and covering containers used to collect palm sap and boiling it before consumption. Where animals such as pigs have been identified as the source of infection, culling these animals has proved effective.
The risk of human-to-human transmission can be reduced through regular hand washing, avoiding sharing food or bedding with infected individuals and wearing personal protective equipment when handling the corpses of people who have died from Nipah.
During the 2018 Kerala outbreak, public health officials carried out extensive contact tracing, isolated infected individuals and ramped up hospital infection control practices, bringing the outbreak under control within a month. Greater awareness and surveillance of Nipah virus is also important to detect outbreaks as soon as they occur.
7. Vaccines are being developed against it
While there are currently no approved human vaccines or treatments for Nipah, several are currently in clinical trials, including an mRNA-based vaccine, one based on a protein from the closely related Hendra virus and another that uses a harmless vesicular stomatitis virus to deliver a Nipah virus protein. The International Centre for Diarrhoeal Disease Research in Bangladesh is also studying around 50 Nipah survivors to better understand the body's response to the virus and support vaccine development.








