Vaccines Explained
Vaccines save millions of lives a year, but what exactly is a vaccine and what goes into making one? And how do we know they are safe? Here, we talk about every aspect of vaccines and why they are so important for our health.
- 28 April 2021
- 9 min read
- by Priya Joi

What is a vaccine?
Vaccines differ from other medical drugs in two important ways. The first is that they are designed to prevent disease, rather than treat it. They do this by priming a person’s immune system to recognise a specific disease-causing bacteria, virus or other pathogen. This “memory” can last years, or in some cases for life, which is why vaccination can be so effective, stopping people from getting sick rather than waiting until disease occurs. The second is that vaccines by their nature tend to be biological products, rather than chemical like most drugs. This not only means that the processes involved in making them are usually more complex and expensive, but also that they tend to be less stable than chemicals and more vulnerable to temperature changes. Because of this, vaccines normally need to be refrigerated to keep them within a specific temperature range. The type of vaccine will determine how low a temperature the vaccine needs to be stored at. Most vaccines need to be kept refrigerated or frozen, but intranasal vaccines are now being developed that can be stored at room temperature.
How do vaccines work?
Vaccines prime the immune system to detect a particular virus or bacteria by showing it a harmless version of the pathogen, or part of it – much like giving a bloodhound a rag to sniff – so that it can remember it and is able to mount a defence if the person ever becomes infected. They typically do this by stimulating the production of antibodies, which are proteins made by our bodies to fight disease. This can also help stimulate other parts of our immune defences, such as T cells. This is the basic premise for how all vaccines work; precisely how they achieve this can vary significantly. Some vaccines involve introducing a whole but inactivated (or a whole, live but shortened version) – and therefore safe – version of the germ into the body, while others contain only a specific part (such as a single protein normally found on the surface of the pathogen). In all cases, the aim is to get specific antibody-generating particles, or antigens, such as a protein found on the pathogen, to trigger a strong immune reaction. Some newer forms of vaccine don’t contain the antigen itself, but instead a piece of genetic code for it. When this goes into our body, our own cells are used as factories to make the antigens, which the body then reacts to.
Why should I get vaccinated?
Vaccines protect us from serious diseases and some can also help contain the spread of disease, saving around 2-3 million lives every year. Many of us receive these vaccines, for diseases such as measles, meningitis and pneumonia, as routine childhood immunisations. This has led to these diseases becoming less common, or even eliminated, in areas with high levels of vaccination. Some diseases have the potential to be eradicated, as smallpox was in 1980. But because most can exist in animals or in the environment (for example in the soil), they pose an ever-present threat, which is why it is so important that vaccination coverage remain high. Whenever vaccination levels drop, either because of hesitancy or when services are disrupted, these deadly diseases can quickly rebound. The life-saving power of vaccination is a major reason why global health organisations like Gavi are working hard to get vaccines out to low-resource areas where vaccines are either unaffordable or inaccessible. Even in countries where the risk of infectious disease is low, getting vaccinated is still important in order to protect vulnerable people who can’t be vaccinated, such as people with compromised immune systems (like those with cancer or HIV/AIDS) or people with extreme allergies. In addition, vaccines are not always as effective in triggering a robust immune response in elderly people, who may be more vulnerable to disease, and so widespread immunisation is critical to protecting them.
How are vaccines tested?
Vaccines go through a rigorous process of testing before they are used in the general population. Once researchers have found a promising candidate, they put it through pre-clinical studies, usually testing it on animals to assess its safety and potential to prevent disease. If a vaccine passes that test, it goes into phase 1 trials, where it is given to a small group of people to confirm its safety in humans, to see if it triggers an immune response and to figure out the dosage. In phase 2 trials, the vaccine is given to a larger group (usually hundreds) of volunteers to see whether the immune response triggered is strong enough, and whether there are any side effects. In this phase, the volunteers are divided into two groups, one which gets the vaccine and one which gets a placebo. In phase 3 trials, the vaccine candidate is given to thousands of volunteers, again divided in two groups as for phase 2 trials. During public health emergencies, such as COVID-19, when no licensed vaccine or treatment exists, vaccine candidates may be licensed for emergency use, if they have made it to the end or nearly the end of phase 3 trials and the evidence suggests they are safe and effective. Even after a vaccine has been approved and rolled-out into the general public, it is monitored very closely for a number of years to keep a close eye on side effects.
What ingredients do vaccines contain?
All vaccines contain active ingredients called “antigens” that trigger an immune response to viruses, bacteria and other pathogens. But in order to work well, it is important that they also contain other key ingredients to keep them safe and effective. The main ingredient in most vaccines is water. They also contain emulsifiers and stabilisers to ensure that the other ingredients remain suspended in the solution, and are protected against the effects of temperature changes during transportation or storage. Some vaccines may also contain an adjuvant, a substance designed to boost the immune response to the antigen, while for vials of vaccine containing more than one dose, the addition of a preservative prevents the growth of harmful bacteria or fungi, which may be introduced when each dose is extracted. Finally, vaccines may contain residual trace amounts of materials used during the manufacturing process.
All such vaccine ingredients are included in only tiny amounts, with some found naturally in our bloodstream. They are listed in the written document that accompanies each vaccine container, and subject to rigorous assessment before they can be included. This ensures that the vaccine ingredients are safe in the quantities used, with systems in place to monitor their safety on an ongoing basis.
How are vaccines made?
Vaccines are made up of a whole bacterium or virus, or parts of them, often a protein or sugar. These active components of the vaccine, called antigens, are what trigger an immune response once in the body. Since vaccines are biological products, most conventional viral vaccines need to be grown on biological material, such as chicken eggs with influenza vaccines, mammalian cells with hepatitis A vaccines or yeast for hepatitis B vaccines. The process is fairly laborious and slow. With flu vaccines, for example, the live virus is injected into an embryonated egg, and then once the virus has replicated, the viral material is collected, purified and inactivated. Newer RNA vaccines can be produced from a DNA template; this can be much cheaper and faster than conventional vaccine production.
What different types of vaccines are there?
The types of vaccines include: whole virus (inactivated and live-attenuated) vaccines; genetic material RNA (mRNA) vaccines; subunit; recombinant; polysaccharide and conjugate vaccines; toxoid vaccines; and viral vector vaccines.
-
Whole virus vaccine
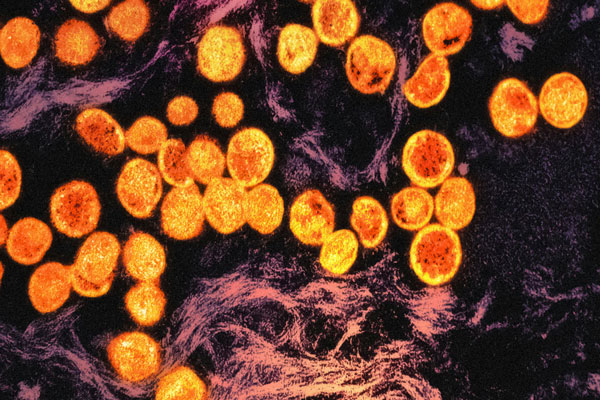
Many conventional vaccines use whole viruses to trigger an immune response. Live attenuated vaccines such as the measles-mumps-rubella (MMR) vaccine use a weakened form of the virus that can still replicate but are unlikely to cause disease. Inactivated vaccines such as hepatitis A use viruses whose genetic material has been destroyed (sometimes referred to as ‘killed’) so they cannot replicate.
-
Nucleic acid
Nucleic acid vaccines use genetic material – either DNA or some forms of RNA – to provide cells with the instructions to make the antigen. Some of the new COVID-19 vaccines use messenger RNA technology.
-
Viral vector
Viral vector vaccines also contain genetic material that give our cells instructions to produce antigens. They use a harmless virus as the ‘vector’ or carrier – which is different from the one the vaccine is targeting – to deliver these instructions into the cell. An example is the rVSV-ZEBOV Ebola vaccine.
-
Subunit, recombinant, polysaccharide and conjugate vaccines
These use one or more antigens – such as a protein or sugar – to trigger an immune response to the germ. Conjugate vaccines for example combine a weak antigen carried by a strong antigen to ensure a stronger immune response. An example is the recombinant hepatitis B vaccine containing a surface antigen.
-
Toxoid vaccines
Toxoid vaccines, such as the tetanus vaccine, use controlled amounts of a toxin made by the germ. They create immunity to the disease-causing parts of the germ instead of the germ itself. That means the immune response is targeted to the toxin instead of the whole germ.
How do we look for potential vaccines?
Scientists might look for vaccine candidates by first looking at vaccines that work for similar diseases, or they might look through libraries for potential pathogenic proteins that could trigger a strong immune response. Scientists must balance the ability of a protein to prime our immune systems with its likelihood to withstand mutation. If pathogens evolve to form new strains, proteins that were once vaccine targets may no longer be present, and this may render the vaccine ineffective. Looking for core proteins may guard against this. This process once took months or years, but now advanced bioinformatic tools, powered by supercomputers, scan and analyse these proteins in days. Artificial intelligence (AI) technology is also starting to be used in ways that could radically change the speed at which potential vaccines are created. This could be extremely important for vaccines against bacteria or viruses that are rapidly evolving, rendering vaccines less effective against them. The global databases that are being mined have been constructed over years, with scientists around the world compiling and inputting information on various pathogens.