Why we need integrated dengue management to achieve zero deaths
Dengue outbreaks are set to become increasingly common as climate change shifts epidemiological trends. We need an integrated approach to tackle them.
- 2 November 2023
- 5 min read
- by World Economic Forum

In recent years, countries in South and Southeast Asia, including India, Bangladesh, Thailand, Malaysia, Indonesia, Vietnam, Singapore, and the Philippines, have witnessed worse dengue outbreaks than usual ahead of the traditional peak season.
There is also a high probability of an increasing number of cases in non-endemic countries in coming years, as climate change shifts epidemiological trends.
Changes in weather patterns have resulted in the emergence and re-emergence of climate-sensitive diseases such as dengue, and the number of cases of dengue has increased 30-fold worldwide over the past 50 years.
Dengue not only affects public health, but also imposes an economic burden of up to $8.9 billion worldwide. A comprehensive strategy with targeted measures to manage dengue is therefore needed to achieve a zero-mortality rate by 2030.
Along with existing surveillance and vector control measures, a safe and efficacious vaccine may play an important role in reducing the burden of dengue. Importantly, stakeholder efforts from both public and private sectors are crucial in preventing, managing and controlling this health threat.
How dangerous is dengue?
Dengue is a viral infection transmitted by the Aedes aegypti mosquito and dengue infection can range from subclinical disease to severe flu-like symptoms.
Some patients develop severe dengue associated with severe bleeding, organ impairment and plasma leakage – the main causes of hospital admissions and death from dengue among both adults and children.
Additionally, as infection demographics have shifted towards the older age group, higher rates of co-morbidities in these individuals contribute to more severe disease and mortality.
Dengue's prevalence has risen sharply, and first outbreaks have been reported in countries that were previously not endemic. Nearly half of the world's population is at risk of dengue if no effective solutions are implemented.
Closer to home, there were more than 650,000 dengue cases in Southeast Asia in 2019, and its incidence has risen by 46% between 2015 and 2019. Scientists have theorized that factors including urbanization and climate change have contributed to the rise of dengue as one of the fastest spreading mosquito-borne viral diseases.
In fact, with an estimated 100 million cases per year, dengue causes more illnesses and deaths than any other disease caused by arboviruses.
Large dengue outbreaks can quickly overwhelm healthcare systems, and the estimated annual economic burden of dengue in Southeast Asia of US$950 million, is higher than other infectious diseases, including upper respiratory infections and hepatitis B.
The challenges of tackling dengue
Dengue is a complex disease as there are four serotypes of the virus, each interacting differently with antibodies in the human body.
A person may develop immunity following a dengue infection with one of the serotypes, but remain vulnerable to an infection from the three others. In addition, individuals are at an increased risk of developing more severe dengue following a second infection with a different serotype of dengue.
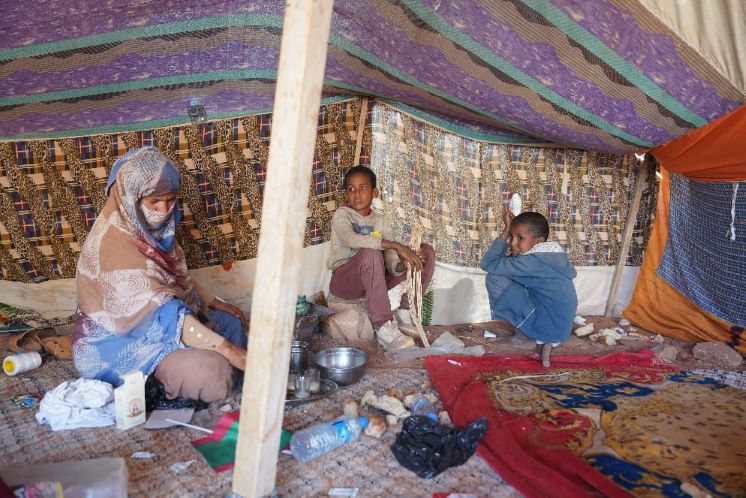
Tackling dengue has posed a difficult task as it is complex and resource intensive to conduct development and research on all four serotypes. Dengue has also historically received limited investment, as the disease burden has been previously restricted to underserved settings.
Currently, there is no universal treatment against dengue, but common prevention methods exist, including personal protection, chemical control and environmental management of the Aedes aegypti mosquitoes.
The World Mosquito Program uses a method that breeds mosquitoes to carry the naturally occurring bacterium Wolbachiaand releases them into the environment. The bacterium makes it difficult for viruses such as dengue to replicate in mosquitoes and reduces the risk of viral spread in humans.
Have you read?
While existing methods of dengue play a role in managing dengue, they are only partially effective. As we intensify the utilization of vector control strategies, a concurrent decrease in population immunity poses a significant challenge in efforts to further control the disease.
This situation resembles the Singapore Paradox, where diminishing immunity levels against dengue lead to increasingly frequent outbreaks.
We must consider the issue of population immunity in the context of integrated dengue management, with vaccines emerging as the pivotal solution to this challenge.
Vaccination, along with other pillars such as surveillance, a robust healthcare system and sustainable community awareness, have been widely recognized at this year's Asia Dengue Summit, where an integrated approach is anticipated to help eradicate the increasing global burden of dengue.
Moving towards dengue eradication
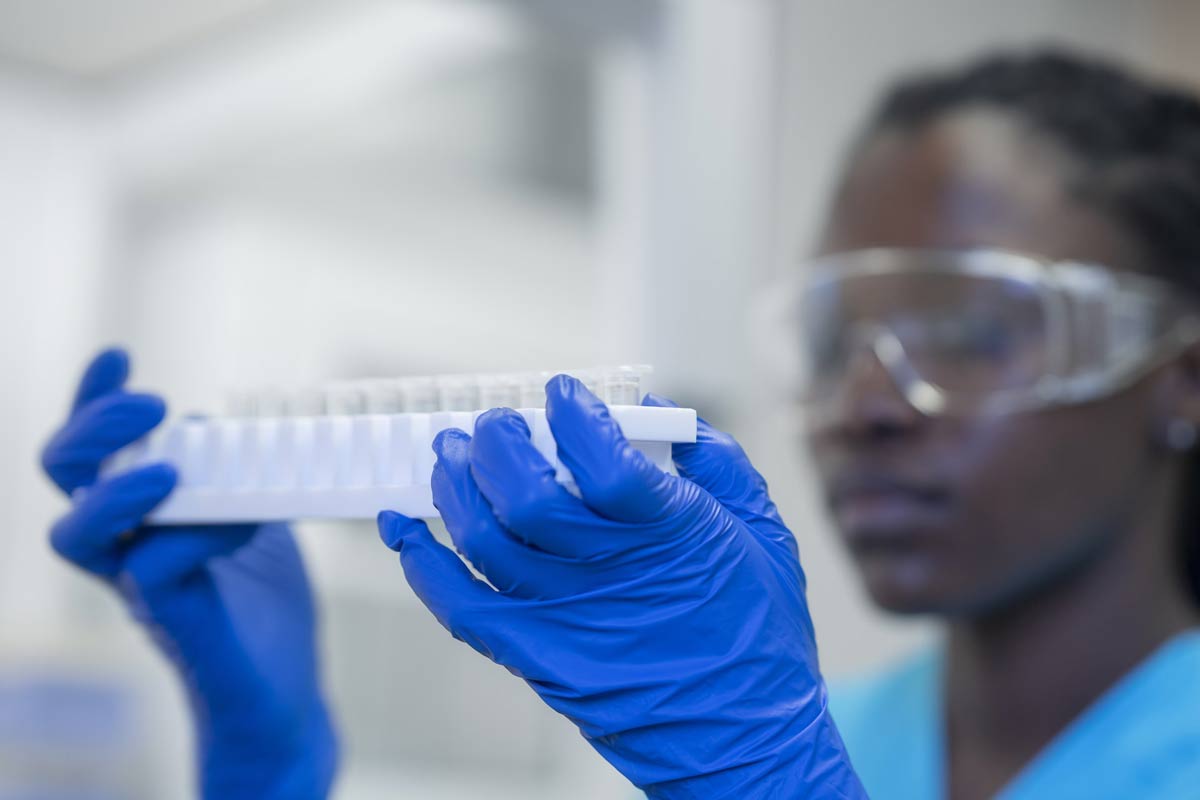
Despite the challenges of developing a dengue vaccine that can protect against all four serotypes of the virus, safe and effective vaccines have now been developed.
Earlier this month, the WHO's expert group on vaccines, SAGE, recommended vaccination be considered in settings with high dengue disease burden and high transmission intensity.
With one of the vaccines recently having been approved in more than 30 countries and another undergoing phase 3 clinical trials, it is hopeful that within the next year, safe and effective vaccines will be available for governments in South and Southeast Asia to consider rolling out public vaccination campaigns.
To complement vaccine innovation, public health communication on the benefits of dengue vaccines is crucial to dispel any vaccine hesitancy, misconceptions and fears. The COVID-19 pandemic has provided a glimpse of the negative impact of misinformation, which led to widespread mistrust in vaccine safety and efficacy.
Lessons can be learned and applied to the introduction of the dengue vaccine, including the importance of collaborating with stakeholders and health authorities to ensure evidence-based educational content is used to promote trust in public health institutions.
This is essential to ensure successful implementation of the vaccine and prevent the spread of misinformation. We need to learn from these events to ensure sustained faith in new interventions.
At the core of the dengue danger is a complacency towards acting regularly to break the cycle of dengue transmission. However, we should not lose hope to prevent future outbreaks in our region.
The road to zero dengue deaths may seem far away, but together, we can start making headway toward achieving this goal.
Written by
Dr Goh Choo Beng, Head of Medical Affairs for India and South-East Asia, Takeda Pharmaceuticals
Prof Tikki Pangestu, Co-Chair, Asia Pacific Immunization Coalition and Visiting Professor, Yong Loo Lin School of Medicine, National University of Singapore
Website
This article was originally published by the World Economic Forum on 1 November 2023.
More from World Economic Forum
Recommended for you