Zika hasn’t disappeared – here’s why it should stay on our radar
Although Zika raced around the world in 2016, leading to babies born with developmental problems, research was slow to explain how the virus worked – until now.
- 26 September 2022
- 6 min read
- by Priya Joi

In May 2015, Brazil reported its first case of Zika virus. The infection raced through 50 other countries in the Americas with lightning speed and by February 2016, Zika virus was declared a public health emergency of international concern. Spread by the Aedes mosquito, Zika is part of the flaviviridae family of RNA viruses, alongside dengue virus, West Nile virus and Japanese encephalitis virus.
Although fatalities from the virus were rare, when pregnant women were infected they were at risk of giving birth to babies with microcephaly, or heads that were smaller than normal, and other neurological impairments. Even when the emergency waned, much remained unknown about how the virus operates.
India had an outbreak of Zika in late 2021 that largely went unreported because the world’s attention was focused on COVID-19. Researchers are concerned the virus is silently spreading across the country.
Now, scientists have found major clues of how Zika virus diverts our immune cells to multiply, and how it can cause microencephaly in babies. This improved understanding could help in developing pan-flavivirus therapies, and also highlights how important it is to find a vaccine.
Hijacking human cells
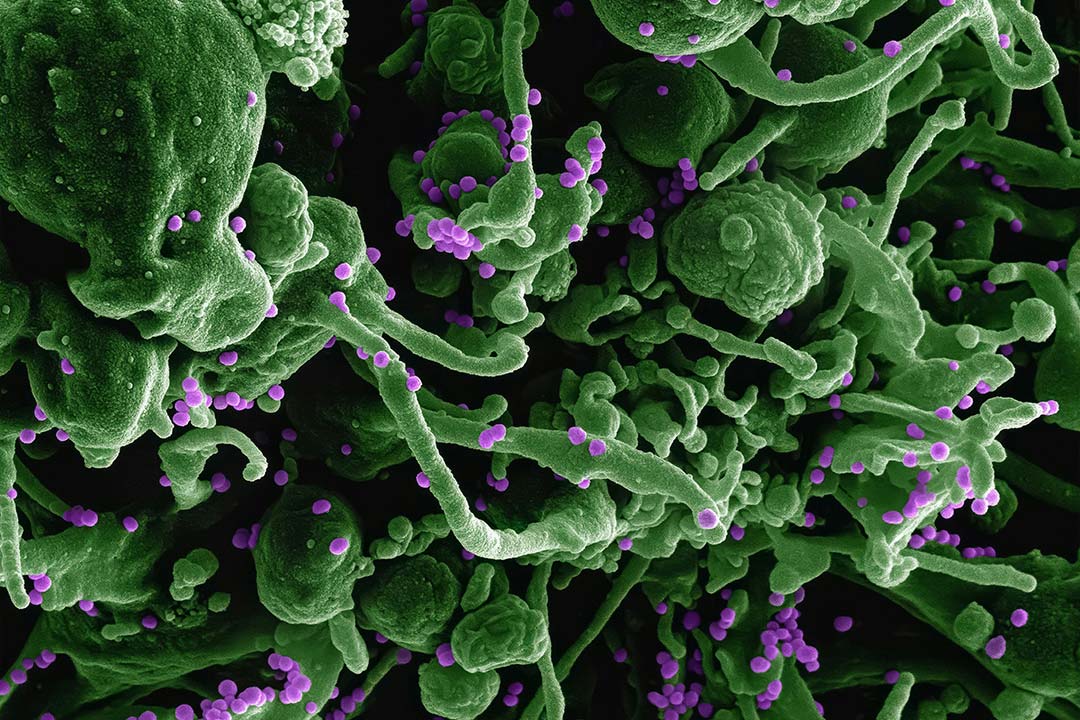
A team led by Emilie Branche at La Jolla Institute for Immunology, California, found that once inside our body, the Zika virus heads straight for dendritic cells that are critical in our immune response to pathogens. Dendritic cells show the antigen – the piece of a pathogen that triggers an immune response – to our immune system.
The Zika virus hijacks our dendritic cells, preventing them from helping the fight against the infection, and forces them to churn out lipid (fat) molecules that the virus uses to replicate.
In their paper in Nature Communications earlier this month, the team showed that Zika manipulates the genes controlling lipid metabolism in dendritic cells. The virus uses a protein called SREBP to force lipid production to ramp up. The researchers suggest that a therapy that silences SREBP could stop the Zika virus from making copies of itself.
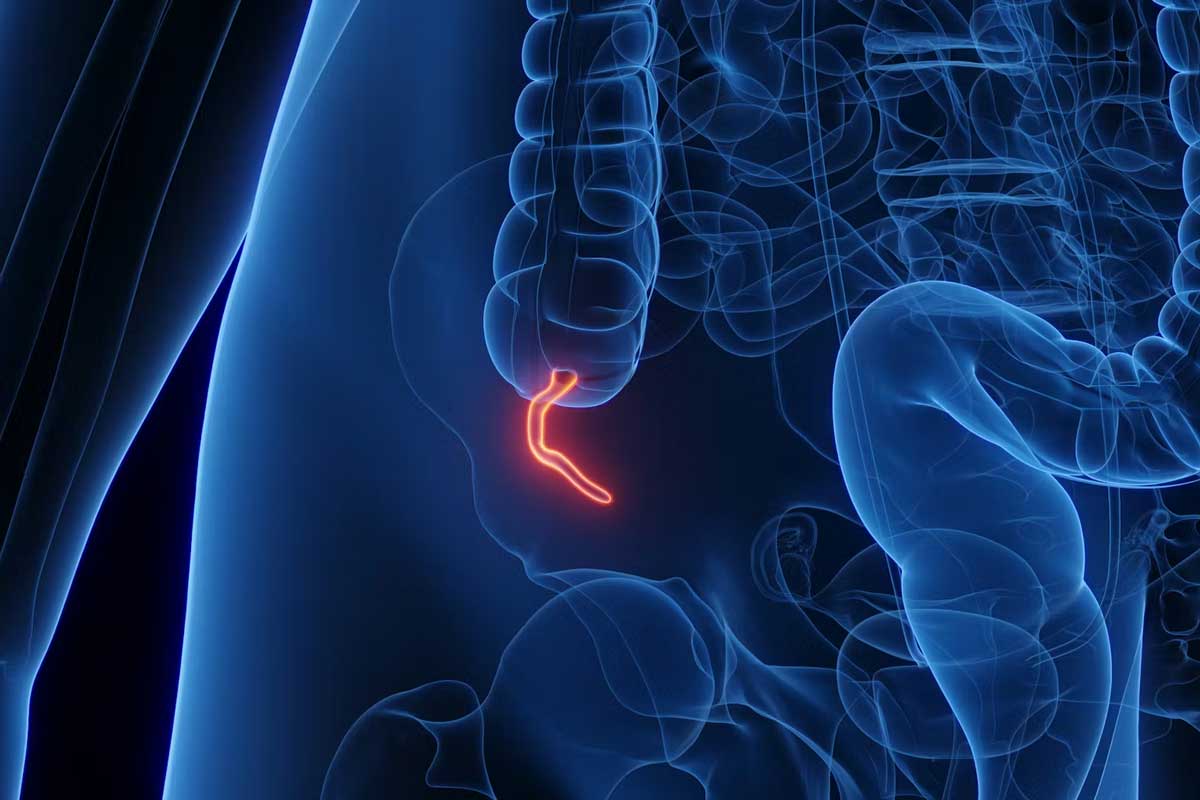
In parallel with this research, a Brazilian research team at the State University of Campinas (UNICAMP), D’Or Institute and the Federal University of Rio de Janeiro unearthed a mechanism by which the virus could be causing microcephaly.
The researchers looked at protein expression in infected cells and, in a paper published this month in Molecular Neurobiology, found that when Zika virus invades the foetal brain, it controls the RNA metabolism expressed in cell nuclei. This change in cell function, the team say, can interfere with particles that act as precursors of oligodendrocytes – neural cells that produce myelin, which is crucial to our nerves being able to transmit information. This can be damaging to brain development, which could explain microcephaly, they say.
Lying in wait
Back in 2016, Brazil was the hardest hit country, with 205,578 probable Zika cases, according to its Ministry of Health. Cases have fallen since the end of 2016, and now the virus is circulating in low levels in Latin America and South and Southeast Asia. However, India had an outbreak of Zika in late 2021 that largely went unreported because the world’s attention was still focused on COVID-19, and researchers publishing in June this year in Frontiers in Microbiology are concerned the virus is silently spreading across the country.
Given the likelihood that Zika could bounce back with climate change, it will be important to have a vaccine at the ready when it does, say researchers. Although several vaccine candidates are in trials, none have been approved so far.
Zika virus is transmitted by infected Aedes species mosquito (Ae. aegypti and Ae. albopictus), the same mosquitoes that spread dengue and chikungunya viruses. In the case of India, inadequate surveillance and poor vector control because of the intense focus on COVID-19 coupled with heavy rains led to an increase in mosquitoes and the spread of the virus.
Climate change could cause a dramatic uptick in Zika cases by altering the range of disease-spreading mosquitoes, as previously uninhabitable areas become warmer and more humid.
Have you read?
Researchers at the Center for the Ecology of Infectious Diseases at the University of Georgia, USA, have created a complex model for how the spread of infectious diseases like Zika will evolve. They found that by 2050, an additional 1.3 billion more people will be living in areas where Zika can spread if nothing is done to combat warming temperatures. Of this 1.3 billion, 737 million people would be living in temperatures allowing Zika transmission year-round.
Halted research
Despite this looming threat, and the 2016 outbreak, the research into Zika has been woefully inadequate, and many questions remain, including how the virus that was first identified in a forest in Uganda 75 years ago turned up in the northeast of Brazil in 2015.
Although we do now know that the Zika virus mutated to allow it to cross the barrier of the placenta in the womb, it’s not clear why some babies born to infected pregnant women are not affected. Nor is it clear why some babies escape microencephaly but still suffer neurological or developmental abnormalities, or why others were born with microencephaly but had no brain damage.
Dr Albert Ko, an epidemiologist and professor of public health at Yale University, told the New York Times that, as Indian researchers suspected, there is Zika transmission in Brazil that is being undetected.
Vaccine urgently needed
Given the likelihood that Zika could bounce back with climate change, it will be important to have a vaccine at the ready when it does, say researchers. Although several vaccine candidates are in trials, none have been approved so far.
The challenge in developing a vaccine has, ironically, been the massive drop in cases. In 2018, the US National Institute of Allergy and Infectious Diseases (NIAID) in Bethesda, Maryland, launched a vaccine trial at 17 sites in nine countries, but as the virus had largely disappeared in the Americas, there were not many infections to prevent.
In addition, as researchers writing in The Lancet have pointed out, the paradox with the related flavivirus dengue is that previous dengue exposure does not provide protection to a subsequent infection by a different serotype. Instead it increases the risk of development of severe dengue disease. This understanding, they say, led to “justified caution” and the development of tetravalent dengue vaccines. As Zika and dengue can often be endemic in the same area, it will be critical to understand how Zika and dengue immune interactions will affect subsequent flavivirus outbreaks and the use of vaccines against these diseases.
While it’s hard to predict what the next infectious disease to cause a public health emergency will be, Zika experts are agreed that the disease is unlikely to disappear and the world needs to be ready to prevent the next outbreak.