How to end the pandemic
WHO has outlined four potential scenarios for the future of COVID-19 and shared a strategy for how the world can end the acute phase of the pandemic.
- 22 April 2022
- 4 min read
- by Priya Joi

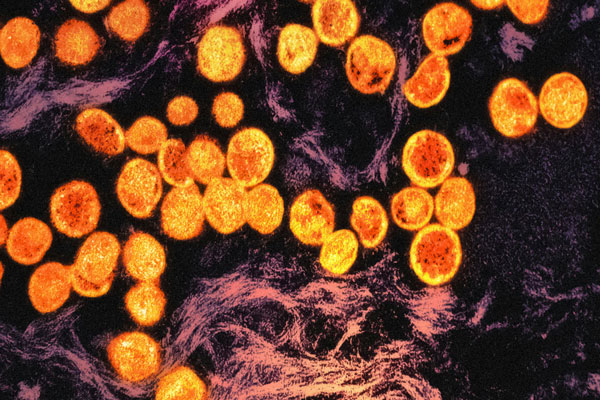
More than six million people have died from COVID-19 and the pandemic continues in most of the world. WHO’s Strategic Preparedness, Readiness and Response Plan (SPRP) has published a new report including strategic adjustments to the current COVID-19 response that can end the acute phase of the pandemic.
It will require, WHO says, coordinated action both within and between countries and a commitment to delivering vaccines and treatment faster and to more people.
In the best case, future variants of SARS-CoV-2 are much less severe than current variants, and immunity can be maintained without regular booster doses of vaccines or developing new versions of vaccines.
The organisation says that while it is not possible to eliminate the SARS-CoV-2 virus at this stage, the global emergency that is filling up hospitals and claiming millions of lives could end through strategic action at both the global and national level.
Planning for potential scenarios
WHO envisions three main potential scenarios regarding viral evolution and human immunity: a base case scenario, a best-case scenario and a worst-case scenario. These are the three scenarios it details for planning purposes, but also adds a fourth scenario where a new SARS-CoV-2 virus emerges that is distinctly different from the current one.
The base case scenario: In the base case, which is the current working model, the virus continues to evolve but the severity is significantly reduced over time due to immunity. In this scenario, there would be a further decoupling between incidence of cases and severe disease leading to progressively less severe outbreaks. There may be spikes in transmission if immunity wanes significantly, which will require booster doses of vaccine.
Have you read?
The best-case scenario: In the best case, future variants of SARS-CoV-2 are much less severe than current variants, and immunity can be maintained without regular booster doses of vaccines or developing new versions of vaccines.
The worst-case scenario: In the worst-case scenario, a more virulent and highly transmissible variant emerges, against which vaccines are not as effective or immunity against severe disease and death wanes rapidly, especially in the most immunocompromised groups. This would require developing significantly different vaccines and either full redeployment or boosting of high-priority groups.
An integrated plan to end the acute phase
WHO has outlined two strategic goals to bring a halt to the pandemic – reducing infections and preventing, diagnosing and treating COVID-19.
The agency has identified five interacting subsystems of preparedness, readiness and response that countries will need to focus on, with the engagement of their population and collaboration with other countries, in order to reduce virus transmission and the impact of disease.
One of these is vaccination and other public health interventions, surveillance and public health intelligence to meet WHO’s goal of vaccinating 70% of countries’ populations by the middle of this year. A third of the global population is yet to receive a single dose.
Another is research, development and equitable access to interventions. WHO and partners, including Gavi, created the Access to COVID-19 Tools (ACT) Accelerator in April 2020. COVAX is part of this and has shipped more than 1.4 billion vaccine doses to 145 economies. To boost the efficiency of delivery, WHO, Gavi and UNICEF launched the COVID-19 Vaccine Delivery Partnership with key partners including Africa CDC and the World Bank.
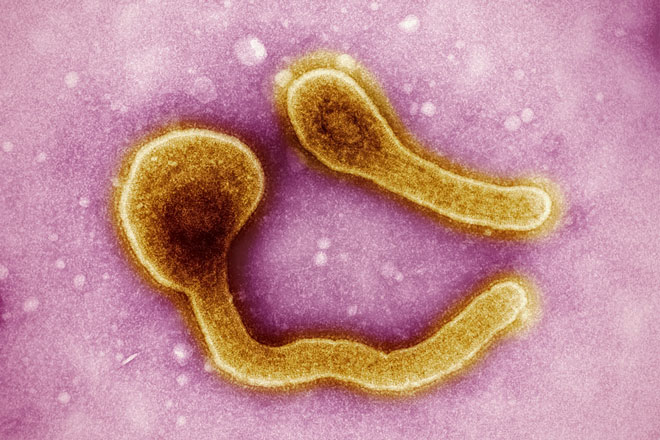
A third is surveillance and public health intelligence – reliable data is critical to tracking the spread and evolution of the virus. Having dynamic knowledge of where to respond and when is vital. WHO suggests integrating the surveillance of SARS-CoV-2 with systems of surveillance for flu or other respiratory pathogens.
Resilient health systems and scalable clinical care make up a fourth subsystem for focus, in which WHO calls for the effective management of COVID-19 through early diagnosis and treatment. To facilitate the dissemination of new treatments at country level, WHO and ACT-A partners have created the COVID-19 clinical care readiness (C3R) framework.
Finally, there is pandemic preparedness, readiness and response coordination. This is where countries need to consider how to transition from an emergency operation to integrating a COVID-19 response into their respiratory disease surveillance and health services management.
More from Priya Joi
Recommended for you