An immunologist’s reflections on nine months of long COVID
In 2022, Dr Stéphanie Longet got COVID-19 and then Long COVID. Here, Longet, who studies vaccine-induced immunity, talks to VaccinesWork about her mission to understand the condition better.
- 15 March 2023
- 7 min read
- by Priya Joi

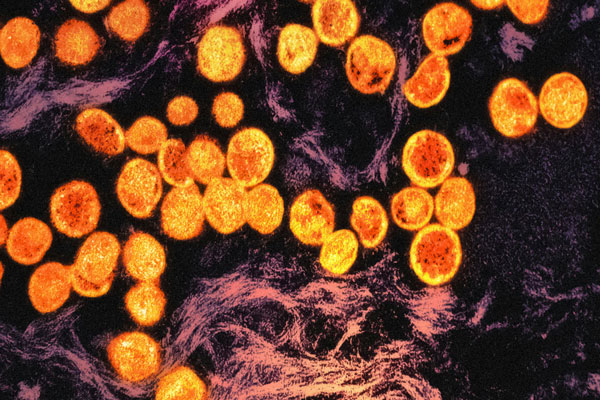
11 March marked three years since the World Health Organization declared COVID-19 to be a pandemic, and 15 March is International Long COVID Awareness Day. Between 10% and 20% of those who get COVID-19 develop Long COVID, in which symptoms such as fatigue, brain fog, muscle pain and shortness of breath persist long after the initial infection.
Several mechanisms have been suggested that trigger Long COVID, and treatments and vaccines are being tested, but for now, many patients exist in a limbo where they are not sure why they are still symptomatic, are unable to alleviate their symptoms for any length of time, and are unsure about when, if ever, they will fully recover.
Mucosal vaccines would stimulate neutralising antibodies and active immune cells at site the virus enters the body, which could prevent infection rather than fighting it – this would also reduce the spread of the virus.
Dr Stephanie Longet, who moved recently from the University of Oxford, UK, to be an assistant professor at the University of Saint-Etienne in France, had studied how to trigger immunity in the mucous membranes such as inside the mouth and nose long before the COVID-19 pandemic hit. When she became sick with Long COVID in June 2022, from which she has still not fully recovered, her work took on a new personal relevance. Now, she is working on how to induce mucosal immune responses to SARS-CoV-2 infection through vaccines targeted at the nose and throat, where the virus enters the body.
At what point after your COVID-19 infection in June 2022 did you realise that you had Long COVID?
I realised I was developing Long COVID a few weeks after my acute infection. When I was not observing any improvements in my legs, I had to accept that probably I had developed chronic symptoms linked to this infection, especially when it got to 12 weeks post-infection, which is the World Health Organization definition of Long COVID symptoms.
This wasn't the first time I experienced persistent symptoms following viral infections. In 2019, I had muscle pain in my back for six months after a flu infection, and then in 2011, I had an intestinal infection that resulted in persistent intestinal symptoms for several years. When I developed Long COVID, I was sad, but I resigned myself to the situation. I knew there were no miraculous cures.
How does Long COVID affect your day-to-day life? Apart from leg pain, do you have any other symptoms? Do you have to adapt your day to accommodate your symptoms?
I lost my sense of taste for three weeks and my sense of smell for six weeks. However, the leg pain is the only symptom which has never gone away. Luckily, it is my only persistent symptom, but I have the feeling that I have the legs of an elderly person (Editor's note: Longet is 36 years old).
I sleep with a pillow under my knees, and I have to sit down much more at work. Climbing stairs is the hardest activity for me. A few days ago, the lift in my institute was not working and as the lab is on the third floor, I had to stop twice while I was climbing stairs.
Usually, in the lab I try to forget my problem and focus on my passion for science, but each basic problem like this reminds me that I did not fully recover from COVID-19. In addition, I had to stop going to concerts when seats are not available. My leg pain worsens when I have other viral infections. Even though I am very cautious, I got a cold a few weeks ago and I am currently in my bed with what is probably flu. So, this is another factor I need to learn how to live with.
Have doctors that you have seen taken your symptoms seriously?
I was lucky, as my general practitioner took my symptoms seriously and sent me for a blood test to exclude other muscle conditions. The test came back normal. However, I know that for some patients, it is a very difficult journey to find doctors who pay proper attention to their symptoms. This is why scientists and patient associations have to educate medical staff about the condition, and on how to support patients. Recognition of Long COVID as a , and follow-up of Long COVID patients remains essential.
Have you read?
Have you had any explanation for your leg pain? And are there things that exacerbate it – e.g. walking or standing, or are your symptoms more random?
I haven't had a specific explanation, no. When I exert myself, the activity can exacerbate pain but my symptoms can be random as well. Sometimes pain can be triggered without any reasons. Sometimes, I wake up with strong pain as if I had run a marathon, but I was only sleeping in my bed.
A study published in February 2023 compared muscle biopsies from Long COVID patients with those from people without Long COVID. The sample number is quite small and it is not a comparison with individuals who fully recovered from COVID-19, but the researchers observed a modification in muscle structure, which could explain fatigue and pain. They also detected more macrophages (a type of white blood cell that kills and removes micro-organisms) in Long COVID patients, and their presence in skeletal muscle tissue could indicate an inflammatory response.
Viral persistence in parts of the body has been suggested as one theory for Long COVID, but in this study the researchers did not find any traces of the SARS-CoV-2 virus in biopsies of Long COVID patients.
Of the various theories for why Long COVID develops, you said the viral reservoir idea seems quite likely. Can you expand on why this one makes most sense to you? Do you think it's possible that in different people, there are different triggers for Long COVID?
Biology is complex, and usually there is not just one explanation. Given that Long COVID symptoms are very heterogenous, I would not be surprised if several causes could trigger the condition, and it could differ from one patient to another. It might be a combination of factors and we need to wait for data to confirm or rule out hypotheses.
A study reported that circulating spike proteins were detected in 60% of patients with Long COVID up to 12 months after acute infection, which could be linked to the hypothesis of viral antigen reservoir. However, an association does not necessarily mean causation. One study showed that vaccination after Long COVID could improve symptoms – possibly by clearing viral antigens – but this is just a hypothesis.
You are now going to work on mucosal vaccines (sprays delivered in the nose and throat rather than as injections in the arm). How could improving long-term respiratory immunity help reduce the infection rate?
Vaccination by injection induces strong protective immune responses at the systemic level and can reduce the risk of severe illness. But it is not very efficient in triggering immune responses in mucosal tissues including respiratory tissues, which is the route of entry of respiratory pathogens such as SARS-CoV-2. Mucosal vaccines would stimulate neutralising antibodies and active immune cells at site the virus enters the body, which could prevent infection rather than fighting it – this would also reduce the spread of the virus.
You also mentioned looking to see whether there are differences in mucosal immunity between people who fully recover from COVID-19 and those who develop Long COVID. Do we know anything about this so far? Are there known differences in immunity between people who get Long COVID and those who don't?
To my knowledge, we do not know if there are any differences in mucosal immunity between individuals who fully recovered from COVID-19 and people who develop Long COVID. If differences are seen, it could potentially be linked to susceptibility to reinfection or susceptibility to other infections, as well as on mucosal inflammation.
Studies have shown microbiome changes associated with ME/CFS (myalgic encephalomyelitis/chronic fatigue syndrome), which might be caused by an infection. Thus, it will be interesting to see if researchers observe differences in the microbiome of Long COVID patients as well.
Long COVID patients also tend to have elevated antibody responses against SARS-CoV-2 and to develop antibody responses against other viruses such as Epstein-Barr virus. Long COVID patients also showed lower levels of cortisol. It's important to remember that while these associations provide new insights, it does not necessarily mean it is the cause of symptoms.