In Kenya, a decade of rotavirus vaccination translates to a drop in childhood mortality
Not only are fewer children being hospitalised with severe diarrhoea, but the vaccine’s evident impact is boosting confidence in immunisation generally, experts say.
- 4 August 2025
- 6 min read
- by Joseph Maina

Kihoto, a densely packed settlement hugging the banks of Lake Naivasha in Kenya’s Rift Valley, has become a living argument for rotavirus vaccination.
Here, in this flat stretch of land where the lake often swells into backyards, diarrhoea is a chronic threat to life, exacerbated by poor sanitation and a growing population.
In this landscape of recurring illness, Nancy Karanja, 54, a local grandmother, plays the role of witness and informal chronicler. Her home, like many in Kihoto, is surrounded by shallow wells and pit latrines – many of which flood when the lake creeps inland. It wasn’t always like this.
“Growing up, the lake was far off,” she said. “We used to draw water from wells that went down 30 feet or more. These days, the water is just below the surface, and I think therein lies the problem.”
Like many of her neighbours, Karanja believes that the rising water table – coupled with an inadequate sewerage system – has transformed Kihoto into fertile ground for illness. “Diarrhoea is common among both children and adults,” Nancy told VaccinesWork during an interview at her home, adding that she recently suffered an episode herself.
Naivasha town has been repeatedly spotlighted in media reports for its high rates of diarrhoeal disease, particularly among children. In 2014 – the year that the rotavirus vaccine first joined Kenya’s routine immunisation schedule – medical officers at the Naivasha Subcounty Referral Hospital revealed that 50% of paediatric admissions were diarrhoea cases. Rotavirus, a highly contagious virus that causes acute gastroenteritis and spreads in contaminated food and water, was identified as the dominant cause, responsible for 56% of diarrhoea cases in Kenya at the time.
Change comes to Kihoto
Back then, diarrhoea was an urgent and widespread threat to life – especially for the youngest residents.
“You would hear about children being rushed to the hospital, weak and dehydrated,” said Fredrick Chege, a community health promoter (CHP) stationed in Kihoto. “Many mothers would come to a local clinic with panic on their faces , especially during the rainy season.”
According to Chege, food and water contamination was a major culprit. “We have poor sewerage here. Toilets overflow. People still rely on shallow wells. And food vendors get vegetables from farms irrigated with sewage water.”
These challenges remain, but both Karanja and Chege say things health outcomes have changed for the better, particularly for younger children.
“Since the vaccine was introduced,” Chege noted, “we still see diarrhoea – that has not stopped completely – but the very severe ones, the ones that required admission? They have reduced. Vaccinated children recover faster, and we rarely see cases of extreme dehydration like before.”
Karanja agrees. Her grandchildren, who live with her, were vaccinated against rotavirus – and she has seen the difference firsthand.
“Their stomach problems are fewer. And when they do get sick, they bounce back quickly. I think that vaccine is what has helped this household.”

Few cases among the unvaccinated
Across Naivasha, health workers describe a profound shift in how childhood diarrhoea is understood. Kirimi Nkatha, a clinical officer who runs a small private facility called Kihoto Links Medical Clinic, says a number of his referrals are still diarrhoea-related, but expectations have changed.
“About a decade ago, we would see a steady stream of children with watery diarrhoea – many of them under five. It was a constant concern. Today, we see fewer severe cases among vaccinated kids. The problem now is making sure everyone gets the vaccine,” he told VaccinesWork at his clinic.
He points to another persistent challenge: access to clean water. “Our vegetables come from polluted farms. Sewerage is openly flowing in parts of Kihoto. We are managing symptoms, not solving the root.”
Nkatha has also had to push back against cultural barriers. “Some people here still prefer herbal remedies, or they do not believe in modern medicine. We are seeing improvement, but vaccine awareness needs to be strengthened.”
“Marked drop in childhood mortality”
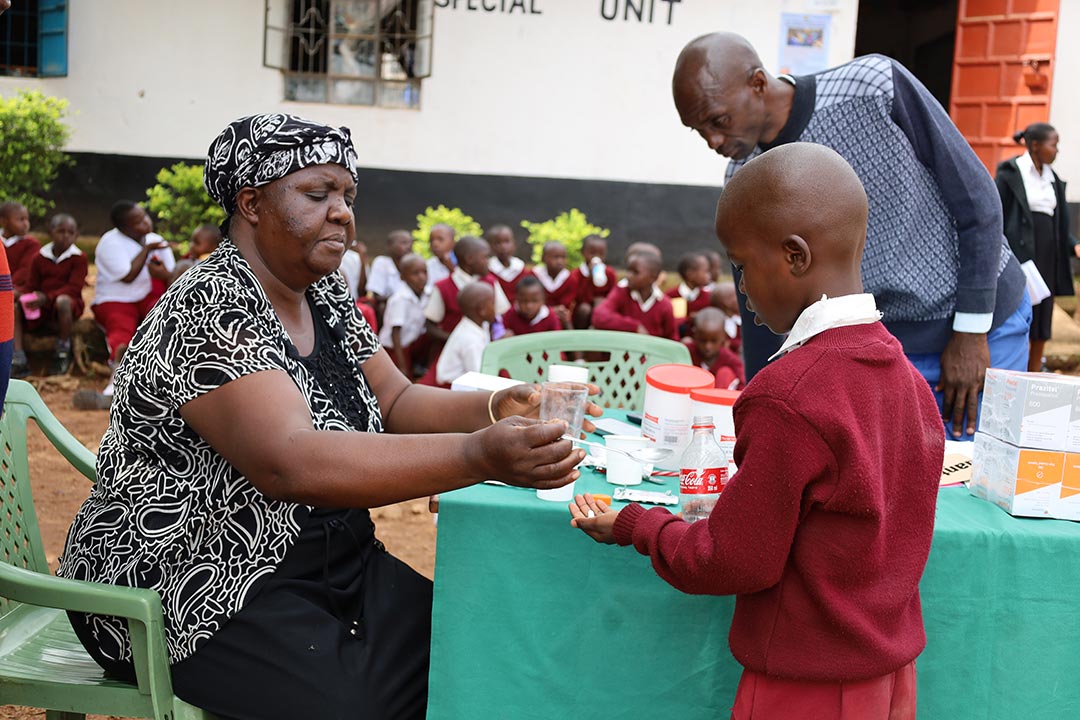
The benefits of Kenya’s rotavirus vaccine roll-out, which was introduced into the national immunisation schedule in 2014, are supported by science. According to Dr Margaret Lubaale, Executive Director of the Health NGOs Network (HENNET), Kenya has witnessed a 60–70% reduction in rotavirus-related hospitalisations in high-burden counties.
“This decline has translated into a marked drop in under-five mortality linked to diarrhoeal diseases, once among Kenya’s top child killers,” Dr Lubaale explained to VaccinesWork. “Beyond the clinical outcomes, the vaccine has not only saved lives but also strengthened public trust in routine immunisation. Caregivers now see real benefits: fewer hospital bills, healthier children.”
Have you read?
Rotavirus still a threat – vaccines are the “best defence”
But while the vaccine has clearly delivered a blow to the virus, it’s far from a knock-out blow.
“Rotavirus is still very present in Kenya,” said Dr George Obiero, a research scientist and a senior lecturer of molecular biology, genomics and applied bioinformatics at the Department of Biochemistry and Biotechnology, The Technical University of Kenya. “In our studies at Mbagathi and Mama Lucy hospitals in Nairobi, we confirmed that it remains a frontline cause of diarrhoea among children.”
He added that informal settlements, with high population turnover and poor sanitation, create ideal conditions for the virus to thrive.
“Accessing healthcare is also costly for low-income families. So the best defence – and the most affordable – is vaccination.”
Still, challenges remain. Dr Lubaale warns that vaccine supply consistency, financing and community awareness must be improved to sustain these gains.
“Gavi support is phasing out by 2029,” she said. “Kenya must scale up domestic funding, align county procurement with national systems and institutionalise civil society participation in immunisation planning.”
She also flagged vaccine hesitancy and misinformation in informal settlements and underserved remote regions as growing concerns.
“There is a need for sustained community engagement strategies using trusted local influencers like CHPs, religious leaders and mothers’ groups. We must invest in communication strategies rooted in local realities.”
And local realities, in Kihoto, are stubborn.
As Nancy Karanja walked through the narrow paths around her compound, she pointed to a sunken patch of earth behind her house – once a vegetable garden, now a breeding ground for mosquitoes.
“That used to be dry. But these days, after it rains, the lake water pushes all the way here.”
Still, she smiled when she talked about her grandchildren. “They are strong,” she said. “I thank God. And I thank the people who brought those vaccines.”
Kihoto remains vulnerable. But in the daily rhythms of illness and survival, the rotavirus vaccine has drawn a new line – one that keeps the worst at bay.
More from Joseph Maina
Recommended for you