Sierra Leone’s mpox case-count is plummeting. Can the country get to zero new infections?
Ten months into a national public health emergency, and nearly six months into a vaccination campaign, Sierra Leone appears to be winning its fight against mpox.
- 20 November 2025
- 6 min read
- by Saidu Bah

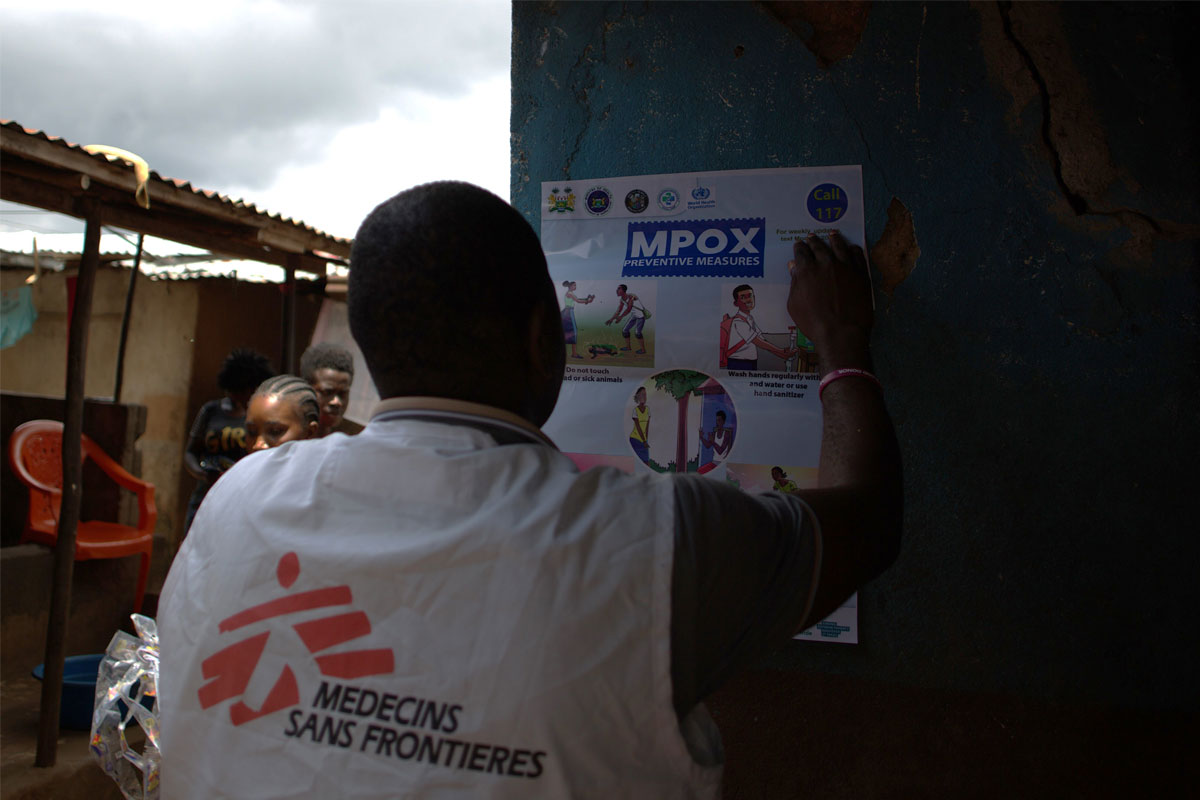
Sierra Leone health authorities are racing against the clock to achieve a sustained zero mpox caseload nationwide, by strengthening surveillance systems while promoting vaccination through deepened community engagement.
Ten months after the mpox outbreak began in the country, the number of new infections has plummeted in recent months.The mpox vaccination campaign, driven by community-led action, is working.
New cases are down from 600 per week in May to less than 30 cases per week in October with some districts recording zero cases sequentially, according to published tallies from the National Public Health Agency.
Previously-established patients centres for infected patients and some treatment centres have been closed by health authorities due to the low admission rate. At the time of writing, fewer than 50 mpox patients were being treated in facilities across the country.
Beating back mpox
The first recorded mpox case in Sierra Leone was in a 27-year-old man from the Western Area Rural District in January. Within four days, a national public health emergency had been declared. Since then, close to 5,500 people have been infected.
People with co-morbidities were more vulnerable – particularly those with HIV, malaria, diabetes, tuberculosis and cancer. By October, 59 people had died with mpox.
“If you have a good immune system, it can be mild. But when your immunity is compromised, then it becomes very contagious,” the clinical lead at the PTS Mpox Treatment Centre in Hastings, Dr Samuel Kelly, told VaccinesWork.
“The virus begins as a rash, then turns to flat spots and grow into bumps before bursting, scabbing over and falling off, often revealing raw flesh beneath. The itching and pain they cause can be painful to the patient,” Dr Kelly said.

“After the spike in cases in March during the Muslim fasting period and the Easter holiday in April, we were recording 80 to 100 cases daily. We went back to the drawing board for a new strategy on how to tackle the rise in mpox cases,” said Stephen Ibrahim Mohamed Koroma, Social Mobilization Coordinator and risk-communication lead for the western rural district.
With support from partners, the District Health Medical Teams started to engage community stakeholders like religious leaders, tribal headmen, traditional healers, market women, schools and transport unions, hoping to spread understanding of the signs and symptoms of mpox, and the means to halt the spread. A dedicated hotline – 117 – took case referrals.
“The community-led action helped us to raise awareness about the virus and we succeeded in reducing the cases across the country,” Koroma said.
Vaccine reaching the last-mile
Sierra Leone received 283,500 doses of mpox vaccine earlier this year, with those doses earmarked for the highest-risk individuals, people living in close contact with infected persons, and frontline health workers. Gavi funded 100,000 of these doses, with an additional 67,000 facilitated by the Vaccine Alliance.
“We started mpox vaccination on 26 April 2025 and the vaccination is still ongoing. With the recommendation from the National Advisory Group, we have expanded the vaccination age from one year and above, instead if 12 years [and up],” Desmond Maada Kangbai, programme manager with the Sierra Leone Expanded Programme on Immunization, told VaccinesWork.

“We are vaccinating more people across the country. Initially we were strictly following the vaccination of all primary and secondary contacts, but now we are also focusing on the high risk population: people living with HIV, cancer and tuberculosis; commercial sex workers and individuals with non-heterosexual or non-cisgender identities like lesbian, gay, bisexual and transgender.
“We have vaccinated nearly 200,000 people since the mpox outbreak and we still need more in a bid to get to zero mpox cases nationwide,” Kangbai said.
He added that the vaccine has played “a very important role”, with a drop in the case-count following hard on the heels of intensified immunisation efforts. At this point, the target seems in reach. “We want to bring the cases to zero and be declared over,” Kangbai said.
“Thankfully our partners from different countries, through the Gavi platform, provided us the vaccines with support from Africa CDC, UNICEF, UAE and the United States Government,” Kangbai said.
Have you read?
Getting those doses to the people in need has relied on a concerted national effort. “We are becoming more innovative in our approach around access – reaching the last mile with the vaccine. The foundational experience from Ebola and COVID-19 has helped us a lot with an effective response strategy.”
Mpox survivors fighting mistrust
Mpox survivors in Sierra Leone have launched an initiative to fight against discrimination, launching an anti-stigma campaign under the slogan: ‘I’m not Contagious, I am a Survivor.’
The campaign is aimed at supporting the reintegration of recovered patients through working with families, chiefs, religious leaders and employers to combat discrimination and prevent job loss.
Nelson Johnson, a 29-year-old entrepreneur who is leading the advocacy group after his recovery, recalls how he got the virus after attending a public event in Bo District South of the country, where he noticed rashes and bumps on his body.
After conducting a laboratory test, Nelson was confirmed mpox-positive and was rushed to a treatment centre in Freetown. There, he was cared for until the infection resolved.
Soon he learned that recovery was not the end of the ordeal for many of his fellow patients. Many were rejected by families, employers, and communities, even after their illnesses had passed the infectious stage.
Refusing to remain silent, Johnson formed a WhatsApp group to connect, share resources and support other recovered patients. It has since become something of a lifeline to many former patients – and a source of strength and support to national efforts to tamp down the outbreak.

“We are working towards ensuring no survivor is abandoned after the outbreak, through a compassionate approach in educating and empowering communities with accurate information about epidemic threats, and to reduce fear through a newly formed organisation called the Sierra Leone Epidemic Action Network,” Johnson told VaccinesWork.
The network is working closely with Ministry of Health and the National Public Health Agency on a national mpox risk-mapping exercise across the country.
“Survivors of an epidemic can heal, and also turn resilience into action,” Nelson said. “We actively refer suspected mpox cases to the designated testing and treatment centres and provide psychosocial support with messages of hope to reassure patients that they are not alone in their recovery journey.”








