Malawi health workers report drop in malaria cases following vaccine intro
This rainy season, referral hospitals in Malawi have found themselves able to dedicate resources to other priorities, following a drop in childhood malaria cases.
- 18 March 2024
- 5 min read
- by Josephine Chinele

From December to March each year, primary health facilities in Nsanje, a district in southern Malawi, used to fill up with gravely sick young patients, as malaria transmission rates rose amid the rainy weather.
Records from the Nsanje District Health Office (DHO) indicate that before 2019, health facilities registered as many as eight to ten malaria episodes per child, per year. "This is a lot for one child," says Nsanje DHO spokesperson George Mbotwa.
But in the years since April 2019, when the world's first malaria vaccine began to roll out in Malawi as part of the three-country pilot programme, there's been a noticeable change to both the frequency and the severity of malaria bouts in this hard-hit district – and a major improvement to rates of under-five hospitalisation nationwide.
“We have seen a reduction in under-five in-patient admissions […]. We are aware that we also have other malaria prevention interventions, and that they complement each other, but I believe the vaccine has contributed significantly to this reduction.”
– Dr Lumbani Munthali, National Malaria Control Manager, Ministry of Health
"We are now registering four or less episodes, or less severe malaria episodes per child per year. It's still a lot, but at least mild. Generally, the introduction of this vaccine in 2019 has contributed to the drop of malaria cases," Mbotwa says.
That's not only encouraging for the most acutely at-risk children and their families, Mbotwa explains. With fewer severe malaria cases being transferred to the district hospital from local health facilities, hospital staff and paramedics are freer to attend to other important responsibilities.
Credit: Nsanje DHO
"When there are severe cases at these facilities, they call for an ambulance to ferry patients for intensive treatment here. Malaria has been the major contributing factor to admissions at this hospital. Less cases mean we are able to concentrate on other things," Mbotwa says.
Three lost each day
According to Malawi's Ministry of Health (MoH), malaria remains the leading cause of death in the country, claiming three lives a day.
"Under-fives make up to 50% of all cases," MoH National Malaria Control Manager Dr Lumbani Munthali reveals.
Malawi was first country worldwide to launch the RTS,S malaria vaccine in pilot implementation. Following the pilot's success, in 2024 a cascade of further countries on the continent are launching the jab as part of their routine immunisation schedules.
Within Malawi, too, access has expanded. Dr Munthali told VaccinesWork that the malaria vaccine is being provided as part of the under-five routine immunisation programme in 11 of Malawi's 28 districts. The implementing districts include Karonga, Nkhata-Bay, Mchinji, Lilongwe, Ntchisi, Balaka, Mangochi, Machinga, Chikwawa, Phalombe and Nsanje.
That means that in those areas of the country, children receive four doses of the vaccine, free of charge. The first is administered at five months old, the second at six months old, the third at seven months old. A final shot is given to children aged 22 months.
"The vaccine is working"
"We have seen a reduction in under-five in-patient admissions […] Nsanje, alongside Balaka, Chikwawa, Mangochi and Ntchisi, has recorded the most improvement in admissions and under-five deaths. We are aware that we also have other malaria prevention interventions, and that they complement each other, but I believe the vaccine has contributed significantly to this reduction," says Dr Munthali.
Have you read?
Overall, he goes on, the roll-out is seeing a positive response. "The vaccine supplies are available, there's also lots of partner support towards awareness, supervision and review meetings. I'm glad that for this vaccine, mothers, communities and caregivers have been very responsive, because they have seen its impact."
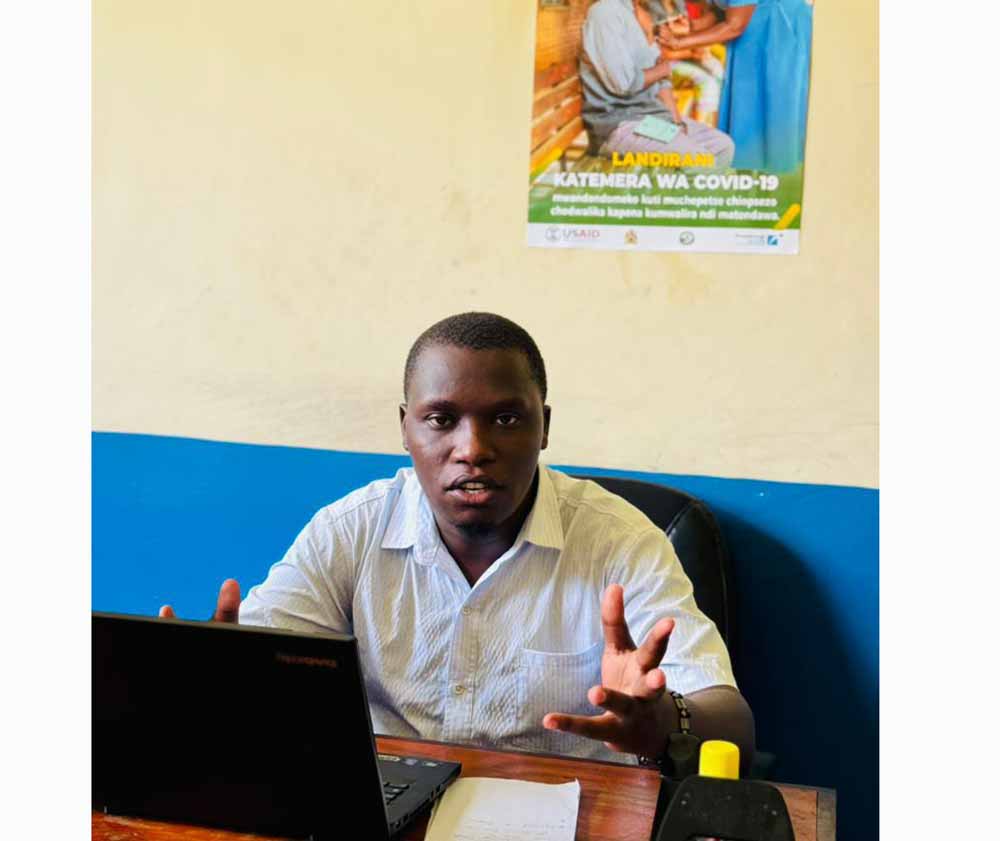
Laban Mtenje, a Health Surveillance Assistant (HSA) assigned to Ndamela Health Centre in Nsanje, remembers how busy the months of January and February used to be with cases of malaria. "This ain't happening anymore, at least in the past few years. For example, last month, 12 under-five children were tested for malaria, but none tested positive. This is a sign that the vaccine is working," Mtenje asserts.

Credit: Kazembe Vuntande
Another HSA, Kazembe Vuntande, says, "This vaccine coincided with COVID-19 vaccine, so parents were initially hesitant. But they have now come through and are vaccinating their children without hesitancy."
Mary Kaluwa, who is raising her two young children in Ngomwa village in Nsanje, is confident of the benefits of the vaccine.
"I’m glad that for this vaccine, mothers, communities and caregivers have been very responsive, because they have seen its impact. Last month, 12 under-five children were tested for malaria, but none tested positive. This is a sign that the vaccine is working.”
– Laban Mtenje, Health Surveillance Assistant, Nsanje
"I have seen children getting deformed or dying due to malaria. I don't want any of my children to go through this," she says.
"My newborn baby will receive the first dose at five months, but my other three-year-old child received all the doses and she has never had malaria."
However, the benefits are not yet being seen everywhere. George Mbotwa points out that geographically hard-to-reach zones, such as swampy areas, have seen higher rates of vaccine defaulting.
"These places are only reached through outreach clinics, which are only possible if we have resources. At times we would want to have these outreach clinics, but may not have fuel to do them," says Mbotwa.
Vaccine's future
Extended Programme on Immuniation (EPI) Programme Manager within MoH Dr Mike Chisema says the Ministry is working towards expansion of malaria vaccine by adding nine more districts by year 2026.
"The remaining districts to cover the whole country will be done by 2028. The vaccine expansion has been slow due to vaccine supply constraints," he says.
Dr Chisema cautions, however, that the malaria vaccine is not a perfect shield, and other interventions – including bednets and seasonal malaria chemoprevention – remain essential. "Take note, this is not a standalone strategic intervention, but complementary. As such, not everything can be attributed to it."