Okegbala: the Nigerian community where leprosy-affected people live free from stigma
Leprosy is curable, but for many who have outlived their infection, the fear of discrimination prevents a return “home”.
- 25 March 2024
- 9 min read
- by Afeez Bolaji

A signboard hung on a weedy roadside in Kwara state, Nigeria, announces the ECWA Hospital at Okegbala. Established by the European missionaries in 1942, and later handed over to the Evangelical Church Winning All (ECWA), the health centre is designated for the treatment of people with leprosy.
The hospital sits north of a high-rise church and three brown-painted dormitories. These are home to people who have undergone treatment for leprosy – a curable bacterial disease – and who have been discharged, but who remain unwilling to return to their communities of origin for fear of stigmatisation.
Over the decades, Okegbala, a quiet agrarian area situated about 85 km from Ilorin, the Kwara state capital, has become a refuge and a beacon of hope for people with leprosy.
“A lot of people still see people affected by leprosy as cursed. We are dispelling such myths through awareness creation. We tell people the disease is curable.”
– Dr Andrew Ofoma, Medical adviser to TLM and leprosy project lead
At about noon one mid-March day, Taibatu Owonikoko is outside a small shop where she sells confectionery. Full of life, the 70-something-year-old Owonikoko found new "relations" in this community some 30 years ago, when she came down with leprosy. The evidence of the disease is still on her body – deforming her toes and left arm.
"I was using some herbs when sickness started. I later visited a hospital where I was diagnosed with leprosy. My husband [now deceased] contacted his family, who recommended a traditional healing centre in Ilorin for me. I took some concoctions without seeing any improvement," she recalls.

Credit: Afeez Bolaji
"A friend told me about this place [ECWA Hospital], but before I got here my toes and hand were already affected. They treated me for free, and the patches on my skin disappeared. I have been here for over 30 years now.
"Relocating from the city centre to live here is tough, but I have no choice. Most of us are here because we don't want to be stigmatised if we go back to our communities. It is our fate and we have accepted it. I do this petty trade to augment the money my children, who live in the city, give me," she explains.
Leprosy, also called Hansen's disease, is a chronic infectious disease caused by Mycobacterium leprae. Despite significant progress towards the elimination of leprosy globally, more than 200,000 new cases continue to be reported every year across 120 countries, including Nigeria.
The disease mainly, and progressively, affects the skin and peripheral nerves, leading to loss of feeling or weakness of the muscles. Though curable with a six-month or year-long course of multi-drug therapy (MDT), which effectively eliminates the bacterial infection, the nerve damage and deformity caused by the bacteria can be permanent if detected late or left untreated.
"Damaged nerves cannot be automatically repaired. When somebody is infected with leprosy, they begin to have nodes and patches on their skin. Those nodes and patches can disappear if the case is presented early for treatment. But a dropped nose and clutched fingers cannot be reversed, even after leprosy is cured. That is why we always advocate early identification and detection of cases to avoid disability," explains Jeffrey Chinwendu, communications officer with non-profit organisation The Leprosy Mission Nigeria (TLM), which supports health facilities like ECWA Hospital to treat infected persons.
Loss of sensation puts even cured patients at risk of progressive disability, as unfelt injuries, especially to the hands and feet, are easily sustained and difficult to safeguard from infection.
People with leprosy accepted by host community
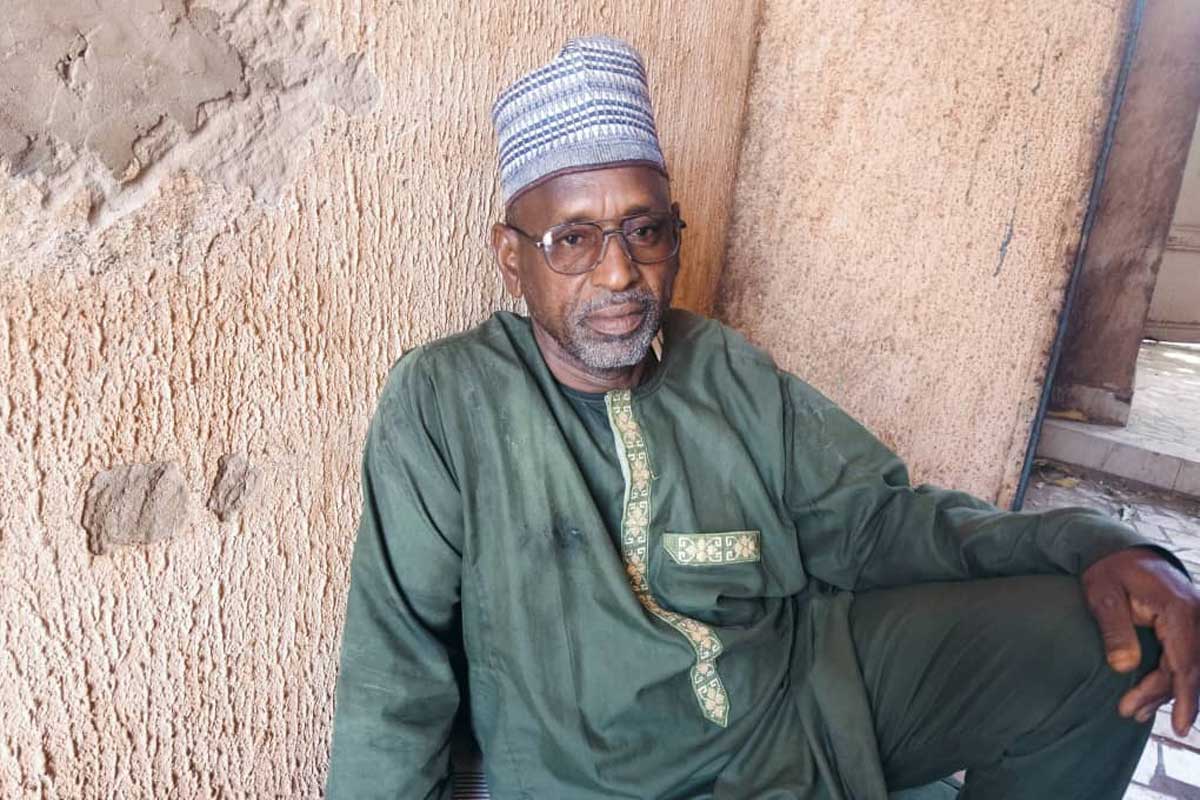
Fabunmi Julius, head of the community of leprosy-affected people here, says TLM's sensitisation efforts have led to increased acceptance of people with leprosy by the host community, and bolstered survivors' self-esteem as they struggle daily to get by.
Julius has no deformity. He was among the few whose case was detected early enough to avert lasting damage.

Credit: Afeez Bolaji
"I have been here for about 36 years. It is fear of stigmatisation that makes many people stay back after they have been treated," he says, echoing Owonikoko. "Some were sent back by their families after they returned home. We are about 40 families living here. Some of us relocated our children and wives to this place. And we are happy our hosts don't discriminate against us. TLM and some other organisations usually come to sensitise them.
"Some people have been abandoned by their families," he says. "Some can't walk and most of us survive on charity from individuals and organisations that visit here. A few people who work also assist others in little ways.
"A foundation built the dormitories and gave us beds and fans. They also sank a borehole, while TLM facilitated power supply into this community. We also get aid from the government on World Leprosy Day, but we need them to do more. Many survive on begging," he explains.
Workers count successes amid challenges
Abiodun Samuel, ECWA Hospital administrative head, says the medical team has treated over 100 active cases through aid from TLM and other organisations, since he joined the health centre 20 years ago.
"We used to have many cases. There were times we had emergency cases brought in at midnight. It [leprosy] has reduced drastically, but we still receive one or two new cases every year," he says, indicating two middle-aged patients chatting with each other along the hospital walkway.
For Samuel, working at the hospital is a personal mission. He says his team makes a lot of sacrifices – sometimes at the expense of their own welfare – to take good care of the patients.
"If I were to consider my remuneration, I am not supposed to work here. I render the service for the sake of God, and that is what has kept me here. I had worked in a place with a much better welfare package. There was a time the church owed us [health workers] two months' salaries. They had to downsize the workforce to be able to pay salaries regularly, and the remaining health personnel took on more responsibilities. My joy is that the hospital is now far better than the way I met it.

Credit: Afeez Bolaji
"To the glory of God, we have treated over 100 cases since I came here. We performed corrective surgeries successfully for some patients. TLM has done a lot for the patients, but we need more help. We want to renovate the hospital wards; the ceilings are old. We also need modern equipment. If any patient needs to be amputated, we have to take them to a hospital in the city," he says.
Have you read?
Samuel complains that inadequate funding delays treatment of patients and calls for support from the government and donors to sustain quality service delivery.
"State-run hospitals use this facility as a referral centre for leprosy. The state government gives us 100,000 naira (about US$ 80) every month to support the running of the hospital, but until recently, the stipend was not regular.
"Also, if drugs some patients need are not among those donated by our donors, they [the patients] have to procure such drugs. Many of them can't afford the price of the drugs. Most times, they have to wait for good Samaritans to visit the hospital and pay for the drugs.
"Another challenge we have is that many of them who have been treated and discharged go to marketplaces to beg to feed themselves. We are appealing to the government to help more so they can stop begging," he adds.
Tope Adebayo, a nurse at the hospital, says the social stigma attached to leprosy remains relatively rife. Her own relatives have expressed reservations, she says.

Credit: Afeez Bolaji
"I started working here six months ago. I come from Omu-Aran (a neighbouring community) to this place every day. I spend a lot on transportation. My family discouraged me from working here, but I stood my ground. It has been a new learning ground for me and an opportunity to gather more experience.
"We work 24 hours on shifts, dress the patients' wounds and give them drugs. Even though the task is challenging, I am passionate about it. Leprosy is contagious, but we are very careful in the way we handle the patients," she tells VaccinesWork.
TLM rolls out multiple strategies to tackle leprosy
Medical adviser to TLM and leprosy project lead Dr Andrew Ofoma says the mission adopts a global goal of "the three zeros" – zero transmission of leprosy, zero discrimination, and zero disability – in its advocacy. To achieve that end, the organisation trains health care workers, community volunteers, medicine vendors and traditional healers, he says.
Traditional healers, commonly patronised by locals, are taught to spot leprosy signs and refer patients to the nearest MDT clinic, Ofoma explains, adding that the mission trains health workers across Nigerian hospitals too.
"We train them [health workers] to identify symptoms and diagnose leprosy and to either manage or refer to the appropriate centre where the patient can get adequate care. The treatment is free. In Kwara, we have over 25 MDT clinics across the 16 local government areas of the state.
"We equally do empowerment, because most of those affected by leprosy are impacted by the economy. Some of them lose their jobs. A lot of times, they depend on begging. So, we build their capacity by empowering some of them to make money for themselves. We teach them skills that can earn them money to support themselves and their families.
"We also do high-level advocacy for stakeholders in the government to own and commit to the project, though we have not got enough support from them. The programme is funded by TLM North Ireland," Ofoma explains.
TLM Nigeria, meanwhile, operates in ten states and the federal capital territory, Abuja.
"A lot of people still see people affected by leprosy as cursed. We are dispelling such myths through awareness creation. We tell people the disease is curable," says Ofoma. We also sensitise health workers, because some of them discriminate against people with leprosy when they come for treatment. Once they see someone with skin lesions, they believe it is leprosy even without testing, and assume they will get infected by touching the person.
"We also use community volunteers and mass media to inform communities to stop discrimination against people with leprosy and make them understand they can't contract leprosy by shaking hands with the patients or eating with them.
"We are not where we want to be, but the sensitisation is gaining momentum. We will not relent until we get to the level where everybody will accept people with leprosy and protect their rights. We are collaborating with the federal ministry of health and civil society organisations," he reveals.
Since its inception in Nigeria in 1988, Ofoma says the mission has contributed to the treatment of over 18,000 people affected by leprosy and rehabilitated many with disabilities.
"We provided assistive devices to some people who lost either their lower or upper limbs to leprosy. Last year, we distributed artificial limbs to over 50 people free of charge with the support of TLM Australia, to help them walk around freely. However, the economic meltdown is impacting our project in terms of funding," he adds.