What are the biggest vaccine breakthroughs coming in 2026? We asked five experts
From mRNA to HIV, we asked five vaccine leaders to share the advances they believe will shape global health in 2026.
- 5 January 2026
- 7 min read
- by Linda Geddes
Maria Elena Bottazzi
Co-Director of the Texas Children’s Hospital Center for Vaccine Development at Baylor College of Medicine in Houston, US

As we move into 2026, the vaccine development landscape is entering a period of remarkable transformation driven by scientific breakthroughs and global collaboration.
Messenger RNA (mRNA) platforms are expanding beyond their initial applications, opening new possibilities for neglected and emerging infectious disease prevention and even therapeutic interventions. At the same time, recombinant protein technologies and viral vectors continue to be prioritised, offering scalable and cost-effective solutions.
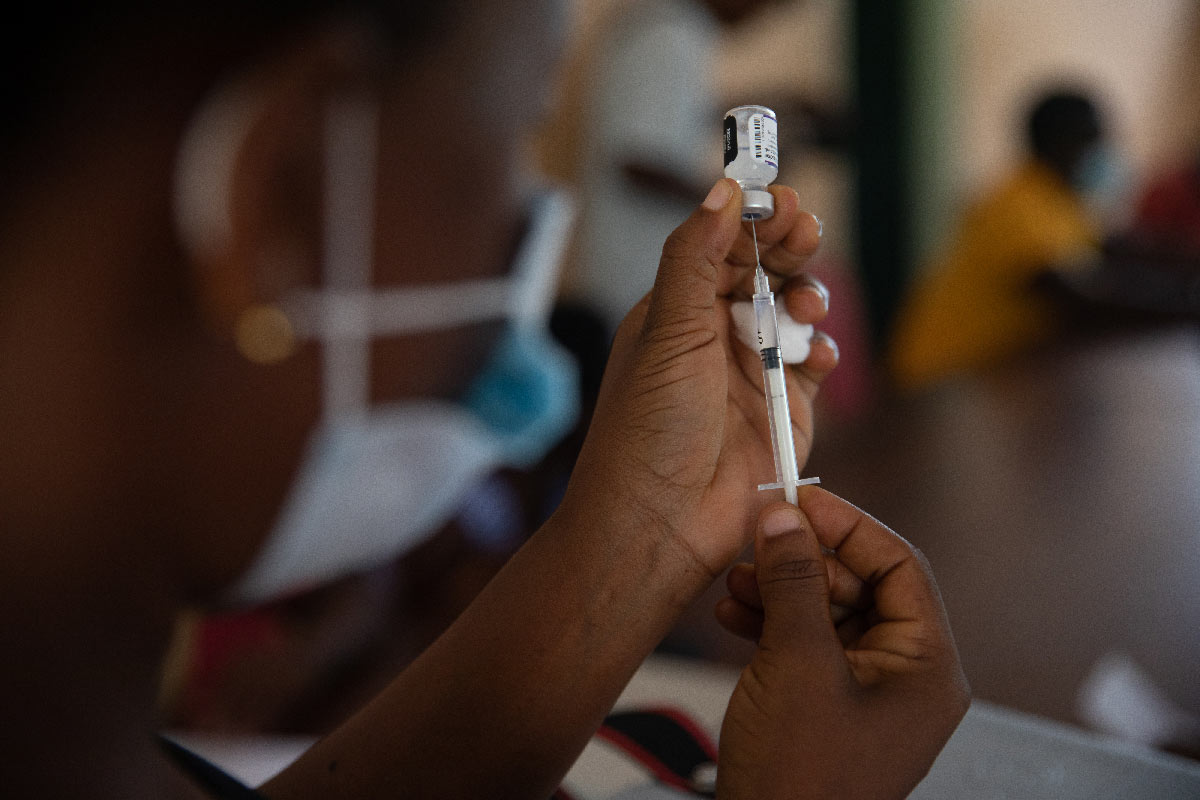
Innovations in vaccine adjuvant and delivery mechanisms – such as targeting the body’s mucosal surfaces (for example the nose, mouth or lungs) and using needle-free patch-based technologies – are poised to enhance immune responses and improve accessibility, particularly in resource-limited settings.
The coming year offers a chance not only to advance science, but to redefine how we deliver impact at scale – building a vaccine ecosystem that is innovative, equitable and globally connected.
Meanwhile, controlled human infection models, in which carefully monitored volunteers are safely exposed to a pathogen, are accelerating early proof-of-efficacy studies, while artificial intelligence is revolutionising vaccine development by helping scientists identify promising targets and design smarter, more flexible clinical trials, enabling unprecedented precision and efficiency.
Equally important are the systemic changes shaping vaccine access and sustainability.
Partnerships with the Developing Countries Vaccine Manufacturer Network are strengthening global supply chains, and manufacturing capacity is expanding significantly in Africa and Latin America – critical steps toward regional self-reliance and resilience. New frameworks for combination vaccines and strategies to establish clear value propositions will help align policy, economic and demand considerations. I view these global trends as an opportunity to ensure that innovation reaches the most vulnerable populations.
The coming year offers a chance not only to advance science, but to redefine how we deliver impact at scale – building a vaccine ecosystem that is innovative, equitable and globally connected.
Beate Kampmann
Director of the London School of Hygiene & Tropical Medicine's MRC Unit The Gambia, and Scientific Director of the Charité Centre for Global Health at Charité – Universitätsmedizin Berlin.

In 2026, further implementation of the safe and effective pre-F fusion vaccine against respiratory syncytial virus (RSV), which is administered to pregnant women and protects young infants, should be a priority.
The pre-F fusion RSV vaccine safely transfers protective antibodies from mothers to babies before birth, protecting them during their most vulnerable period and reducing serious illness and hospital strain.
RSV is a common respiratory virus that can cause severe lung infections and hospitalisation in young infants, especially in the first months of life.
The pre-F fusion RSV vaccine safely transfers protective antibodies from mothers to babies before birth, protecting them during their most vulnerable period and reducing serious illness and hospital strain.
Clinical trials showed efficacy results of over 80% protection from severe RSV in the first few months of life and, following large implementation studies from several high-income countries, we can now be confident that this also holds up in real life without any safety concerns.
I am happy to see that Gavi recognises RSV as a priority and supports introducing maternal vaccines in low- and middle-income countries where RSV mortality is highest. I now look forward to the action.
Gagandeep Kang
Director of Enterics, Diagnostics, Genomics and Epidemiology at the Gates Foundation

Going from a tough year in global health into 2026, we have a lot to look forward to for enteric vaccines – designed to protect against illnesses affecting the gastrointestinal tract.
The Gates Foundation has invested for a while in supporting Biovac, a South African company, directly to develop oral cholera vaccines and in bringing technical and financial partners together to provide further support for what will be the first end-to-end vaccine development programme in Africa.
With successful early-phase testing and regulatory approvals, Biovac’s clinical partners will be recruiting for a phase 3 trial in 2026. This is important not just for the company, but also for the increasingly strong South African regulatory system, as it builds its abilities in making and testing vaccines.
Enteric disease morbidity is a marker of inequity around the world and the more ‘diarrhoea wards’ that close, the better we are doing for the most vulnerable children.
In 2025, we saw the publication of remarkable rotavirus vaccine effectiveness data from India with the Indian-made Rotavac vaccine. In 2026, we should get results from the second Indian vaccine, Rotasiil. These are two of the three WHO-prequalified vaccines that supply Gavi-eligible countries, so this data demonstrates the high impact that rotavirus vaccines have where they are most needed.
In late 2026, we will see the first results from an ongoing study in Pakistan that is testing whether adding a booster dose of oral rotavirus vaccine at nine months increases protection in the second year of life.
Enteric disease morbidity is a marker of inequity around the world and the more ‘diarrhoea wards’ that close, the better we are doing for the most vulnerable children.
Salim S Abdool Karim
Director of the Centre for the AIDS Programme of Research in South Africa (CAPRISA)
The development of an effective HIV vaccine remains an important goal in efforts to achieve an AIDS-free generation.
Following the unprecedented success of mRNA-based COVID-19 vaccines, this platform has become a central focus of HIV vaccine research, offering a promising approach to induce robust and targeted immune responses.
Its ability to rapidly deliver RNA sequences encoding protein immunogens via lipid nanoparticles is promising, though HIV’s genetic diversity and the need to elicit broadly neutralising antibodies – necessary to prevent HIV infection – remain major challenges.
The mRNA vaccine platform will also be tested... to see whether a vaccine could help keep the virus under control without daily medication
Current HIV vaccine research focuses on a germline-targeting approach, in which a sequence of specially designed vaccine components – given over several doses – are used to gradually guide the immune system toward making the rare, powerful antibodies needed to block HIV.
In simple terms, it works like a step-by-step training programme that helps the body develop the immune cells capable of producing these protective antibodies.
The mRNA platform has been prioritised for manufacturing of candidate HIV vaccines now in phase 1 trials, although early studies have noted some safety concerns, particularly skin reactions. Progress is expected to accelerate once these challenges are overcome.
A new phase 1 clinical trial, IAVI G004 , planned for 2026, will test a booster designed to further strengthen the immune response toward developing broadly protective antibodies.
The mRNA vaccine platform will also be tested in studies where people pause their HIV treatment under close supervision, to see whether a vaccine could help keep the virus under control without daily medication as part of the quest for a cure. Despite this progress, an effective HIV vaccine is still out of reach, and no candidates have yet advanced to phase 3 trials. The landscape has also grown more complex after a recent study of Lenacapavir – a long-acting antiretroviral drug used for HIV prevention and treatment – showed 100% efficacy in African trial participants, setting a very high bar for any future vaccine to meet.
Because prevention tools are now so effective, upcoming HIV vaccine trials will need new approaches to show whether vaccines add meaningful benefit.
As a result, 2026 is likely to see the emergence of innovative clinical and regulatory strategies to help germline-targeting vaccines continue to move forward in a world with highly effective HIV prevention.
Dr Jerome H. Kim
Director General of the International Vaccine Institute in Seoul, Republic of Korea

In 2026, vaccines, technologies and stronger ecosystems are converging to expand access to vaccination and drive a more self-sufficient, resilient vaccine landscape.
On the technology front, the year could bring important advances for mRNA platforms, microneedle array patches and combination vaccines. These offer advantages for low- and middle-income countries through better thermostability, simpler delivery models and improved vaccine confidence by reducing pain and decreasing the number of injections required.
There is growing interest in developing vaccines that target high-burden pathogens driving antimicrobial resistance. At the same time, more evidence and updated policy recommendations stand to reshape how we think about life-course vaccination, with a focus on special populations including pregnant, school-age and elderly people.
On the technology front, the year could bring important advances for mRNA platforms, microneedle array patches and combination vaccines.
The year should also bring progress on the systemic enablers needed to translate these innovations into real-world gains. Regional end-to-end vaccine ecosystems are building local capacity, increasing production and access and transforming development away from a model of aid, and towards sovereignty and self-sufficiency.
The growing importance of locally produced vaccines for locally relevant infectious diseases is exemplified by Biovac’s oral cholera vaccine entering a clinical trial – a first for end-to-end cholera vaccine production in Africa.
A renewed emphasis on the full value of vaccines is also needed globally in 2026, highlighting their role in sustaining health systems, protecting economies and enabling progress.
The International Vaccine Institute (IVI) is advancing many of these priorities and continued strategic investment – including support for enabling partners such as Gavi – will be crucial for ensuring that these new innovations reach populations, overcome market and systemic barriers, and deliver impact for the communities that need them most.







