Pfizer’s COVID-19 vaccine may be over 90% efficacious, so what happens next?
An interim analysis of the Pfizer/BioNTech vaccine candidate suggests is more efficacious than many had dared to expect. The announcement is a welcome indication that a safe and effective COVID-19 vaccine might be within reach, but there are still many challenges to overcome.
- 10 November 2020
- 4 min read
- by Linda Geddes
Hopes of an effective vaccine against COVID-19 have been bolstered with the announcement of large-scale clinical trial data by Pfizer/BioNTech, suggesting that their vaccine candidate is more than 90% efficacious at preventing disease and is well-tolerated.
The companies have already begun manufacturing the vaccine and expect 50 million doses to be globally available by the end of the year, with up to 1.3 billion doses anticipated in 2021.
Distribution will initially be challenging for many countries, because the vaccine must be stored at ultra-low temperatures of below -70˚ C.
Although a phase 3 trial of the vaccine is ongoing, interim results suggesting such a high degree of protection raise hopes that the vaccine will at least slow the course of the pandemic. They also suggest that other COVID-19 candidate vaccines which are based on the same viral protein will be successful – including all the vaccines in the COVAX portfolio.
What do we know about the vaccine?
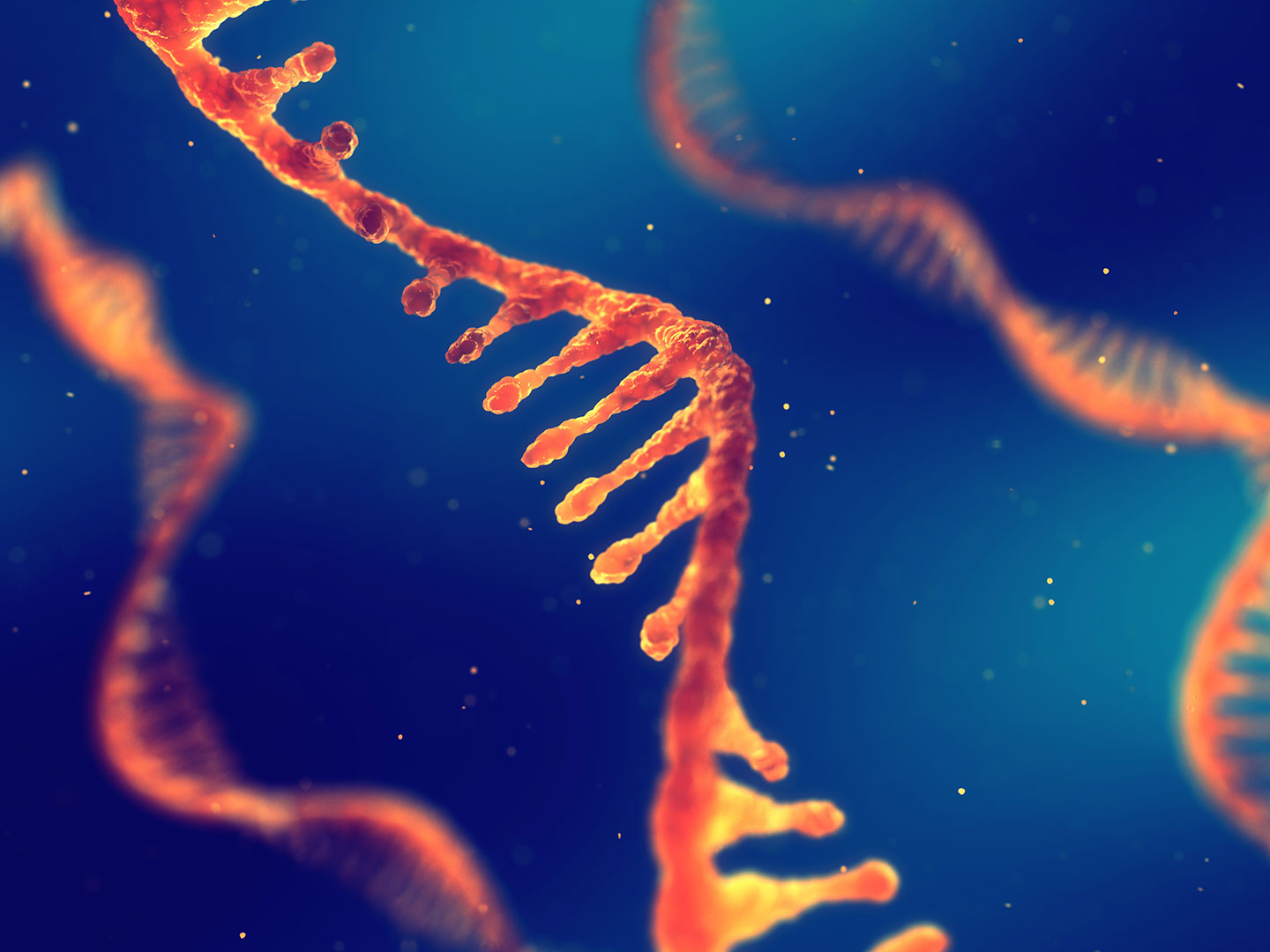
The Pfizer/BioNTech vaccine candidate, called BNT162b2, is based on a relatively new technology. It is an RNA vaccine, which means it uses a piece of genetic code, in this case messenger RNA (mRNA), to issue instructions to cells in the body to make antigens, which then trigger an immune response. In the case of BNT162b2 the antigen is the same as the viral spike proteins found on SARS-CoV-2 virus, which the virus uses to gain entry into our cells.
This mRNA is packaged into lipid nanoparticles, which act like a delivery system, enabling the genetic instructions to cross the fatty membranes that surrounds cells. The vaccine is administered by injection into the shoulder muscle, with a second dose required three weeks later. Once inside the body, the mRNA makes its way into cells, where the protein factories within the cell read the genetic code and manufacture large numbers of these viral proteins. The cell then secretes the viral protein, triggering an immune response.
How effective is it?
So far, the vaccine has been administered to 43,538 people, 38,955 of whom have received a second dose. Pfizer and BioNTech agreed to conduct an interim analysis of the vaccine’s efficacy once there were at least 62 confirmed cases of COVID-19 among trial participants – some of whom received a placebo vaccine. So far, there have been 94 confirmed cases.
We still don’t know precisely how many of those who received the active vaccine went on to develop COVID-19, and we’ll need to wait for the data to be published to better understand some aspects of the vaccine’s performance. However, according to a Pfizer press release “the case split between vaccinated individuals and those who received the placebo indicates a vaccine efficacy rate above 90%, at seven days after the second dose”. It is also too soon to know if the vaccine will be equally efficacious among different age and racial groups.
Have you read?
The results of an earlier trial suggested the production of lower quantities of neutralising antibodies among older vaccine recipients. It also suggested that the side effects associated with the vaccine were mild, and in line with what would normally be expected following vaccination, namely soreness at the injection site, muscle or joint pain, chills, fever and headache. No serious safety concerns have been observed during the latest trial, which is not yet complete and will continue following volunteers until at least 164 confirmed COVID-19 cases have accrued among participants. Pfizer is expected to apply for an Emergency Use Authorisation from the US Food and Drugs Administration by the end of November.
How easy will the vaccine be to distribute?
Distribution will initially be challenging for many countries, because the vaccine must be stored at ultra-low temperatures of below -70˚ C. This is far lower than most existing vaccines (which are kept between 2-8˚ C), and well below what can be achieved with conventional cold storage refrigerators and freezers. The need for specialised cold storage facilities represents a potential barrier to widespread use as currently few countries already have this kind of equipment in place.
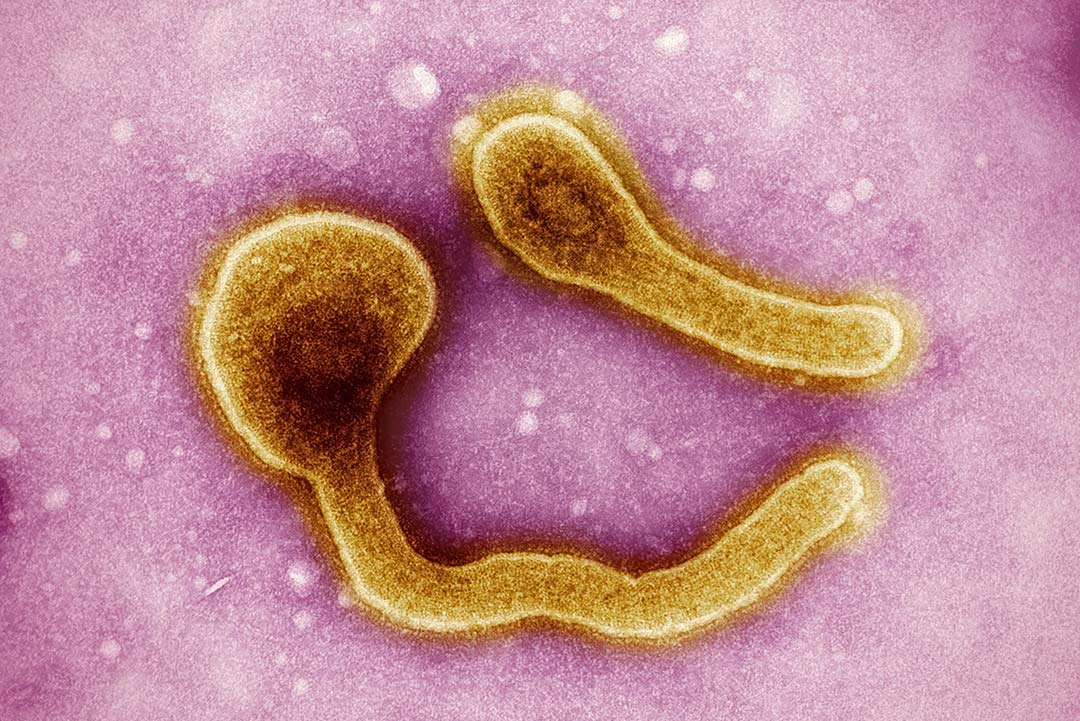
Anticipating this challenge, Pfizer is also reported to have designed a suitcase-sized shipping container, each capable of holding between 1,000 and 5,000 doses at the desired temperature for up to ten days during transportation from its manufacturing facilities. And even in low- and middle-income countries where this could imply additional costs, the challenge of storing these kinds of vaccines isn’t insurmountable, as the Democratic Republic of the Congo is already demonstrated. The currently licensed Ebola vaccine requires similar storage at -70˚ to -80˚C, and yet the country still vaccinated over 300,000 people during the recent epidemic in the East of the Country.