In rural Malawi, demand for malaria vaccine rises
In districts that got early access to vaccination, parents say fewer bouts of malaria leave more time to tend crops.
- 28 November 2024
- 3 min read
- by Charles Pensulo

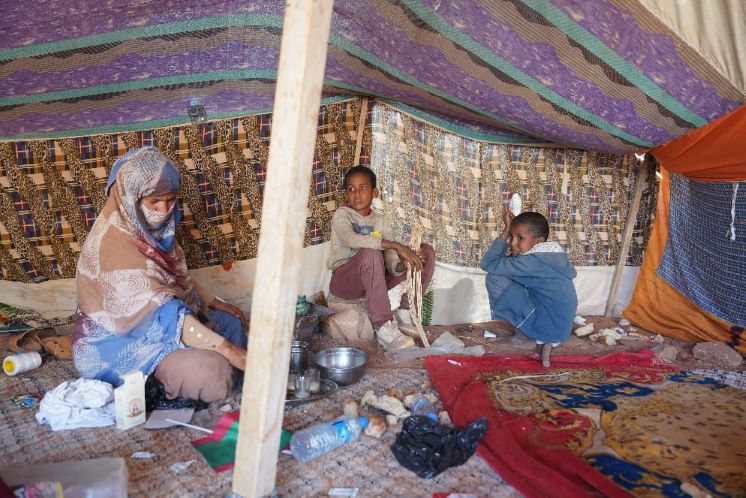
On a cloudy morning, Lucy Zakaria, 38, of Sangano Village in Malawi's Phalombe district, cradles her one-year-and-eight-month-old baby at the hospital as she awaits her turn to see the doctor.
"She has some rashes on her face, I hope nothing serious," she says. Zakaria knows the district hospital, which sits on a plain surrounded by mountains, better than she'd like.
Mother-of-five Zakaria says the vaccine has seemed to leave her youngest safer from malaria than her older siblings, and has given Zakaria and her husband more time to dedicate to their livelihood
She adjusts her wrapper and checks the surroundings. A few years ago, a journey to the hospital on a bicycle–close to two-hours was all but routine, she explains: "I was cycling this trip four times a week because my children used to suffer from malaria," Zakaria says.
The daughter in her arms, Favour Ignasio, is her fifth, and Zakaria is hopeful that Favour is far less likely to fall sick with the parasitic scourge than her older siblings were, growing up.
Favour is one of the 400,000 children in Malawi to have received doses of the world's first malaria vaccine, as a part of the WHO-coordinated Malaria Vaccine Implementation Programme (MVIP).
Phalombe district is one of the 11 of Malawi's 28 districts to have piloted the vaccine as part of the MVIP, and here, as elsewhere in the country, malaria control has included a number of interventions, including, prominently, insecticide-treated nets (ITN) distribution and case management. These interventions remain crucial even in the era of vaccination.
But the addition of the malaria vaccine has clearly made a significant impact. Data from 2016, three years before the inception of the immunisation campaign, records a nationwide incidence rate of 407 per 1,000 people, and a mortality rate of 23 per 100,000 people. By 2021 – two years into vaccination, with other malaria control interventions deployed in complement – those numbers had improved markedly: incidence now registered at 361 per 1000, and mortality was down to 8 per 100,000 people.
Have you read?
Adrian Chikumbe, Ministry of Health (MoH) spokesperson, pointed to a significant decline in malaria prevalence and hospitalisation due to the disease, "particularly in children in the 11 districts where we have been administering the malaria vaccine".
The selection of the districts across the country that would roll out vaccines in the first phase was based on malaria burden: parts of the country with the highest case-load got priority.
In other districts like Nkhata Bay, Nkhotakota, Mangochi and Balaka – which have the highest malaria burden in Malawi – the ministry intends to also spray with mosquito-killing chemicals. Public health officials have emphasised the need to continue to deploy other malaria-control measures alongside immunisation.
Essential Programme on Immunization (EPI) Programme Manager within MoH Dr Mike Chisema acknowledged an intention to expand the malaria programme, but noted that global supply remained constrained, despite the availability since April this year of a second vaccine. "Other countries have also introduced malaria vaccines like Cameroon, South Sudan, Nigeria and others, which are on their way," he remarked.
While some districts continue to wait their turn, mother-of-five Zakaria says the vaccine has not only seemed to make her youngest safer, but has also given her the opportunity to dedicate more time to her livelihood.
"My husband and I grow maize and soya beans among others. We also do small-scale businesses." A child's hospitalisation, as such, means a disruption to the family's income. "My advice is that other parents should go to the hospital and get the vaccine so that their children can be protected," Zakaria says.