“The vaccine is extremely effective”: no cases of invasive cervical cancer found in Scottish women vaccinated against HPV
Real-world data suggests the HPV vaccine dramatically cuts cancer risk among women who received it during adolescence.
- 26 January 2024
- 4 min read
- by Linda Geddes

Zero cases of cervical cancer have been detected in the 12 years after vaccination among women who received the HPV vaccine at age 12–13, data from Scotland's cervical cancer screening system suggests.
Although it is possible that some of these women may still go on to develop cancer as they get older, the study adds to mounting real-world evidence that vaccination against human papillomavirus (HPV) is highly effective at reducing the risk of cervical cancer – the fourth most common cause of female cancer deaths globally.
Best protection
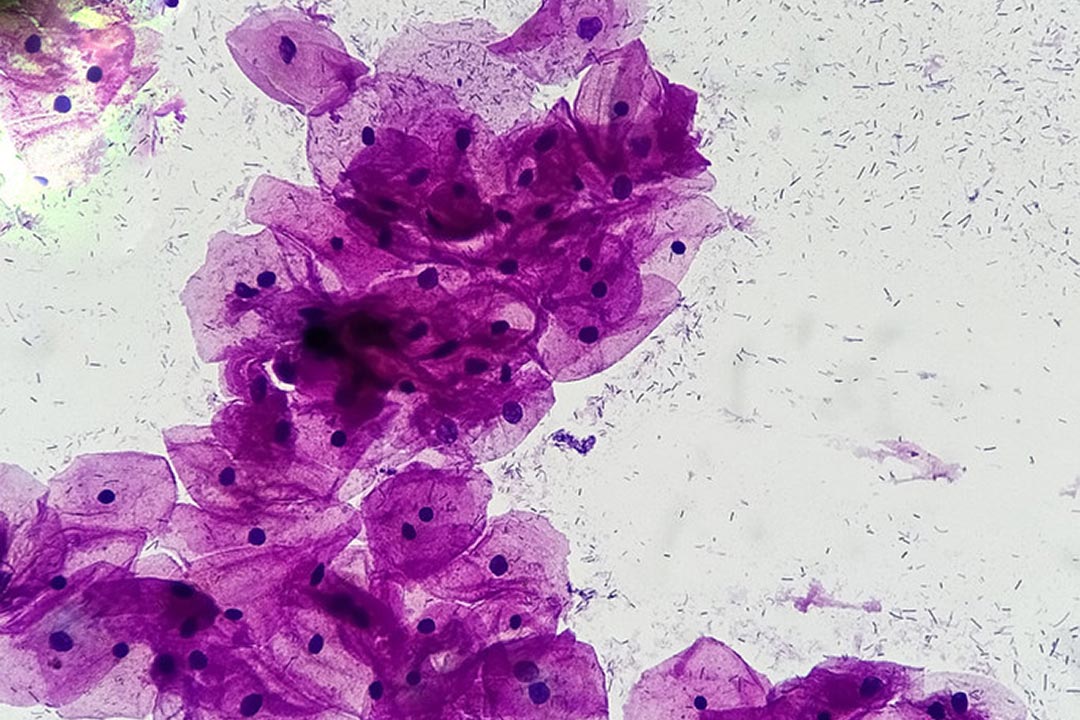
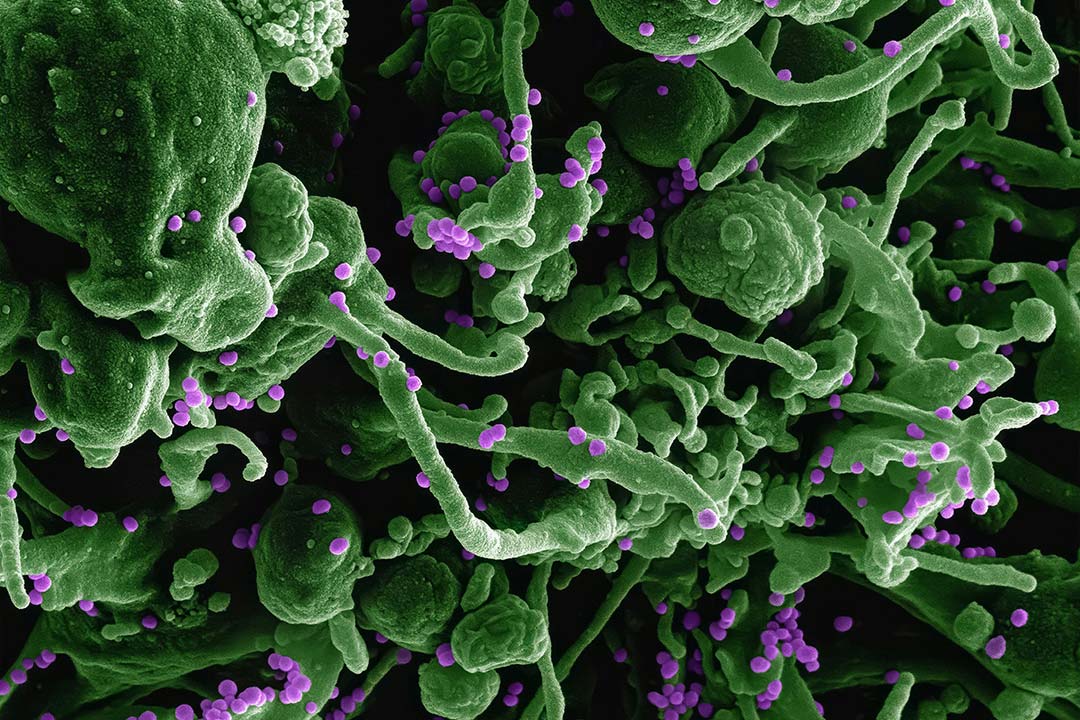
HPV is a common virus that spreads through skin-to-skin contact – especially sexual contact – and is responsible for almost all cases of cervical cancer, as well as causing anal, vaginal, vulval, penile, and mouth and throat cancers in men or women.
“The study is super exciting. It shows that the vaccine is extremely effective. It’s obviously early. We’re just starting to see the first data of the impact of the vaccine because it takes so long from the time of the vaccine to the effects.”
– Prof Kathleen Schmeler, University of Texas MD Anderson Cancer Center
While there is currently no treatment for HPV infection, vaccines protect against the most common cancer-causing forms of the virus, especially if they are given before people become sexually active.
The United Kingdom introduced a school-based national immunisation programme against HPV in 2008, initially targeting girls aged 12 and 13, as well an initial two-year catch-up programme for girls aged 14–18 years.
In a previous study, Dr Timothy Palmer at Public Health Scotland and colleagues reported a 90% reduction in the detection of abnormal cells that could develop into cervical cancer among women in Scotland who received the HPV vaccine at age 12–13, implying that the rates of invasive cervical cancer should also fall in subsequent years.
To investigate, Palmer and colleagues at the Universities of Edinburgh and Strathclyde examined routinely collected data on all women in Scotland born between 1998 and 2016 who were eligible for the national cervical cancer screening programme – including women who were not eligible for HPV vaccination, those vaccinated as part of the routine programme since 2008 and women vaccinated at 14–18 years of age as part of a catch-up program.
They looked at their incidence of invasive cervical cancer, where the cancer spreads from the cervix's surface to deeper tissues or other body parts, often requiring more intense treatment such as chemotherapy and/or radiotherapy.
Have you read?
The research, published in the Journal of the National Cancer Institute, found zero cases of cervical cancer among women who were given their first dose of the vaccine at age 12–13 years until the end of the study period in 2020, irrespective of how many doses they received.
There was also a significant reduction in the incidence of cervical cancer among women who received three doses of the bivalent vaccine – which protects against the two major cancer-causing forms of the virus – when they were aged 14 to 22.
While some cases of cervical cancer were detected among such women, their incidence was two-and-a-half times lower than in unvaccinated women.
The vaccine's impact was also greater among women from more deprived areas, who otherwise experienced a generally higher incidence of cancer.
"This study showed a greater risk reduction than predicted for girls vaccinated at age 12 or 13 years because no cases of invasive cancer have yet been diagnosed in this age group," the researchers said.
However, since a small number of cancers related to lower-risk types of HPV will remain, they cautioned that some women may still develop cervical cancer as they get older. To reduce this risk, countries are increasingly switching to HPV vaccines that protect against further types of HPV, including the quadrivalent and nonavalent vaccines that protect against four and nine types of HPV respectively.
"The study is super exciting. It shows that the vaccine is extremely effective," Prof Kathleen Schmeler at the University of Texas MD Anderson Cancer Center told Stat magazine. "It's obviously early. We're just starting to see the first data of the impact of the vaccine because it takes so long from the time of the vaccine to the effects."
The study is one of several to provide real-world data on the effectiveness of HPV vaccination in recent years. A 2021 study, which examined what happened after the bivalent vaccine was introduced in England in 2008, found that there was a 87% reduction in cervical cancer among girls who received the HPV vaccine when they were 12 or 13 years old. A Danish study published in the Journal of the National Cancer Institute the same year reported similar findings.