Ebola is officially over in North Kivu and Ituri - what can we learn for COVID-19?
On 25 June, the outbreak of Ebola in the Democratic Republic of the Congo that has raged for more than 2 years is over. What does this mean for the country and what can it teach us about ending the COVID-19 pandemic?
- 26 June 2020
- 7 min read
- by Priya Joi
Until the COVID-19 pandemic, one of the biggest global epidemic threats was Ebola. The largest ever outbreak of Ebola in the Democratic Republic of the Congo (DRC) started in 2018, and is now officially over. In theory, the end of an Ebola outbreak is straightforward – once there are no more cases of disease, a 42-day countdown starts, at the end of which the World Health Organization (WHO) officially declares it over. This 42 days is not a random number, but is in fact based on the duration of twice the maximum incubation period for the disease, which for Ebola is 21 days. In this particular case the end was declared 50 days after last case and 42 days after the last patient was discharged from the Ebola Treatment Centre.
In practice, the declaration of the end of Ebola means a period of several months in which public health and government officials and local communities wait to see whether the disease truly has been conquered. This is a crucial time to maintain public engagement, and WHO and others emphasise the critical importance of maintaining active surveillance for at least six months after, combined with routine surveillance for diseases with outbreak potential.
When is a health emergency truly over?
Like COVID-19, Ebola had been declared by WHO as a Public Health Emergency of International Concern (PHEIC). This is intended to mobilise coordinated action against a global threat, acting as a wake-up call. A declaration of a PHEIC can also guide countries on quarantine measures and could unlock emergency contingency funding.
Just as declaring the end of an outbreak or epidemic is not easy, the challenge for WHO can be knowing when to declare that a disease is no longer a PHEIC, as the downscaling of the threat can mean that efforts are diverted elsewhere. For instance, although there are fewer than 100 cases of polio worldwide, WHO maintains the disease is a PHEIC to ensure that the world follows through on its plan to eradicate it.
Why ignoring routine immunisation can ultimately be more deadly
There are major concerns though that funnelling vast resources into fighting one threat can sideline others that are just as lethal. In DRC, as of 24 June, Ebola had infected 3,470 people and killed 2,280 of them. Meanwhile, measles has infected over 369,000 people and killed more than 6,700 of them. This could be just one of many more lethal measles outbreaks – 20 countries have suspended routine immunisation against diseases like measles as health care workers divert their attention to fighting COVID-19. Resurgences of polio could be next as childhood immunisation for this disease has also been halted. This would be horrifying given that there are safe and effective vaccines for both measles and polio.
The temporary slowdown in routine immunisation is an indication of the kind of challenges health officials are facing with the COVID-19 pandemic. Also national lockdowns and the need to prevent the further spread of the novel coronavirus is presenting new challenges to organisations that would normally be doing everything in their power to vaccinate children, especially those in vulnerable communities, against childhood killers like measles and polio.
Vaccines were key to ending the Ebola outbreak
For Ebola, as for many diseases in the past, the key to bringing the outbreak under control was vaccination and tracing the people that infected people may have come into contact with. The development of the rVSV-ZEBOV Ebola vaccine happened in record time, and set a precedent for producing a vaccine against an ongoing infectious disease emergency.
When the 2014-2016 Ebola outbreak started in West Africa, no Ebola vaccine had ever been tested in people. In 2014, Gavi helped encourage manufacturers to develop an Ebola vaccine by committing US$ 300 million to procure vaccine doses, once one was prequalified. This meant development rapidly got underway so that the vaccine was able to reach the final stage of testing (phase 3 trials, in which a vaccine has been shown to be safe and effective and is given to thousands of people). This happened in March 2015, a year after that outbreak started.
The promising results meant that even before licensure and prequalification by WHO, the vaccine could be used on a ‘compassionate use’ basis during the next outbreak in the Democratic Republic of the Congo, which emerged in 2018.
Ebola vaccination, in combination with other measures, proved to be extremely effective in stopping the disease. Data released in April 2019 by WHO, while the outbreak was still ongoing, showed that of the more than 90,000 people who were vaccinated, only 71 developed Ebola.
Vaccination is also likely to be key to ending the COVID-19 pandemic. Currently, with no therapeutics and no vaccines, the only strategy that countries can use is physical distancing and self-isolation coupled with travel restrictions to stop the virus spreading, which is why most of the world has been under lockdown at home. This has had some effect in controlling the epidemic in some countries, with the curve slowly starting to go down. Yet ending a lockdown with a return to life as usual would mean coronavirus cases and deaths spiking again. Ultimately, as long as COVID-19 clusters continue globally, everyone is at risk.
This is why a vaccine is the only feasible way for this pandemic to end. Currently, more than 140 candidates are either in pre-clinical phase (nearly ready for testing in people) or phase 1 or 2 trials (the first and second stages of being tested in humans).
What does the end of Ebola in North Kivu and Ituri really mean?
Just as the global health community was not entirely prepared for Ebola, they haven’t been prepared for COVID-19. There have been warnings for some year year now of the potentially catastrophic effects a pandemic could have. Despite this many countries are ill-prepared. For example, many low- and lower middle-income countries still have inadequate surveillance and diagnostic systems, and have poor health systems, either because of a lack of resources or political will, or because of major events such as conflict or natural disasters.
But as it turned out, no country in the world was truly ready for a pandemic on this scale, with the one possible exception of South Korea, which had previously grappled with MERS.
In 2019, ten years after the last pandemic of H1N1 influenza, an assessment by the Global Health Security Index showed that fewer than 5% of all countries were adequately able to respond to and mitigate the spread of an epidemic. As COVID-19 has submerged health systems even in the richest countries, it is clear that despite the warnings, no nation had learned from history.
DRC, like many countries in Africa, and indeed like low- and middle-income countries worldwide, is dealing with COVID-19 on top of existing health threats. On the one hand, its people may feel weary at the idea of fighting yet another deadly disease.
On the other hand, DRC is fresh with experience of what is really needed to eliminate an infectious threat. Having an effective vaccine is just one piece of the puzzle. A vaccine may not be instantly available for everyone, everywhere and targeting vaccination at those at risk and the people an infected person has been in contact with will be important.
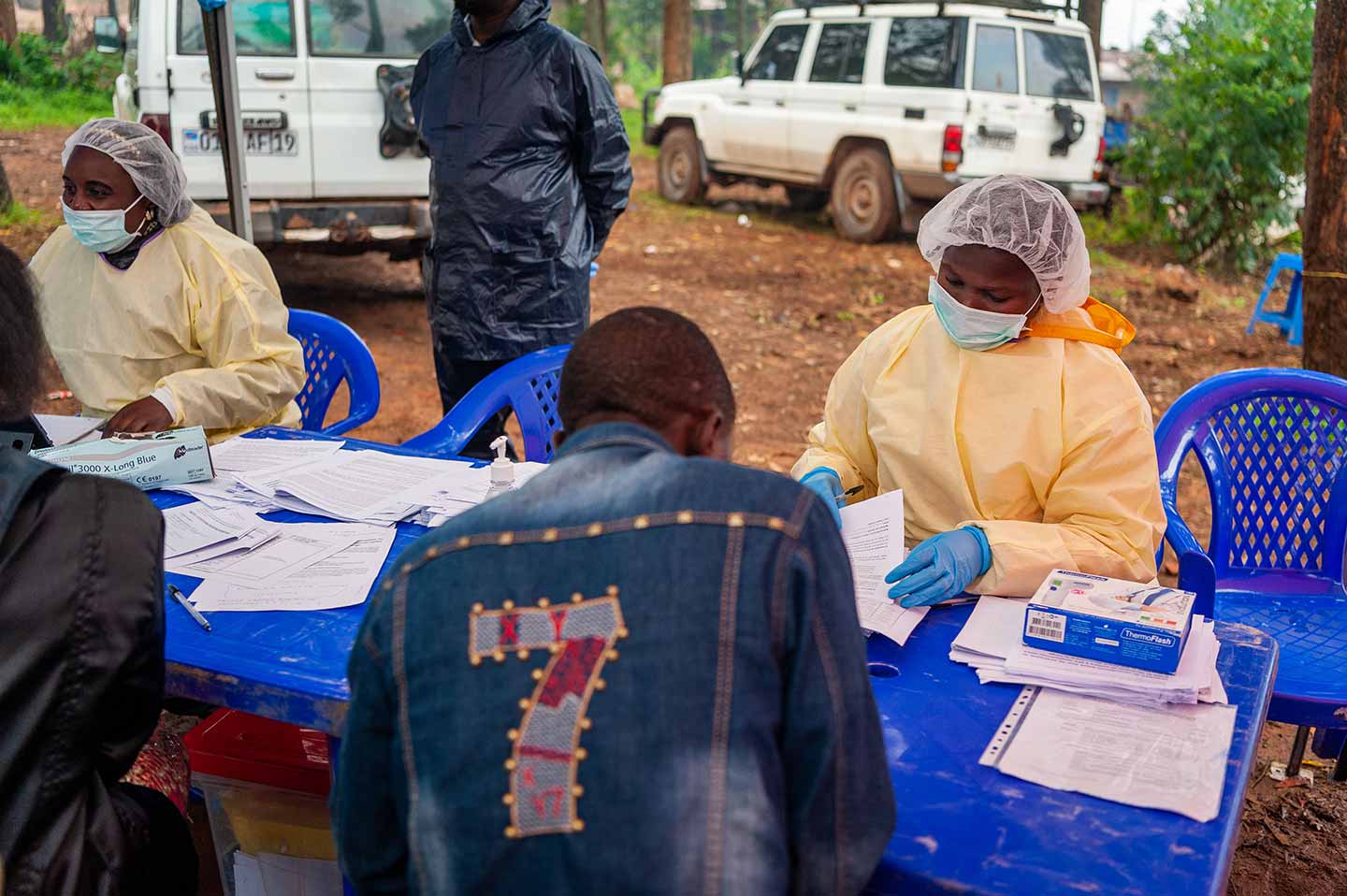
Community engagement and trust is just as important. In DRC, conflict and social tensions meant that health workers – who often needed military escorts for insecure areas – were often viewed with suspicion, as were decisions to bury people who died of Ebola without allowing family to touch the bodies. Ensuring public trust was also key in fighting misinformation about the disease that threatened the efforts to control it.
Similar concerns have arisen over misinformation about COVID-19 – either totally inaccurate information that 5G mobile networks spread the virus, or a misunderstanding that because the coronavirus can cause many cases of mild disease that it is not that deadly.








