Five ways in which the climate crisis is worsening antimicrobial resistance
Extreme weather events, higher temperatures, rising pollution and overcrowding are all contributing to the increase in antimicrobial resistance.
- 21 November 2024
- 5 min read
- by Linda Geddes

Antimicrobial resistance (AMR) and climate change are two of the greatest challenges we face in the coming century, and both have the potential to seriously undermine our health and lifespans. AMR is driven largely by the overuse or misuse of drugs to treat pathogens like bacteria and fungi, and climate change is causing extreme weather events that are devastating communities worldwide. Although on the surface they may appear to be unconnected, these emergencies are surprisingly interlinked.
1. Increased prevalence of disease
Many diseases are climate-sensitive, and changing temperature and weather patterns could enhance the growth, survival and spread of various bacterial, viral, parasitic, fungal and vector-borne diseases. A study of 375 known infectious diseases found that 218 of them could potentially be aggravated by climate change. For instance, warming temperatures and altered rainfall patterns are causing the mosquitoes that transmit malaria to expand their geographic distributions, and helping some fungal pathogens such as Coccidioides, which causes Valley Fever, to spread to new places.
The mass movement of people from one geographical location to another can enhance the spread of resistant microbes around the world.
Extreme weather events such as flooding may also overwhelm sanitation and wastewater treatment infrastructure, bringing more people into contact with bacteria and viruses that live in the gastrointestinal tract, resulting in outbreaks of diseases such as cholera, typhoid and polio. They can also disrupt access and delivery to health services, including routine immunisation, further increasing the risks of health emergencies and disease outbreaks.
The overuse and misuse of antimicrobial drugs and disinfectants are key drivers of antimicrobial resistance, and an increased prevalence of disease could result in even more antimicrobials being used.
2. Population disruption and displacement
Droughts and flooding can contribute to population displacement, meaning there will be more people living in overcrowded camps with fractured public health infrastructure, and inadequate access to clean water and good sanitation. Such conditions further increase the spread of disease and the potential overuse of antimicrobials.
Limited access to health care and robust health guidance may also result in people self-medicating with antibiotics (especially in countries where the sale of pharmaceuticals is poorly regulated), or not completing their full courses of drugs, which can also contribute to the development of antimicrobial resistance.
Meanwhile, the mass movement of people from one geographical location to another can enhance the spread of resistant microbes around the world and the sharing of resistance genes between them.
3. Increasing pollutant exposure
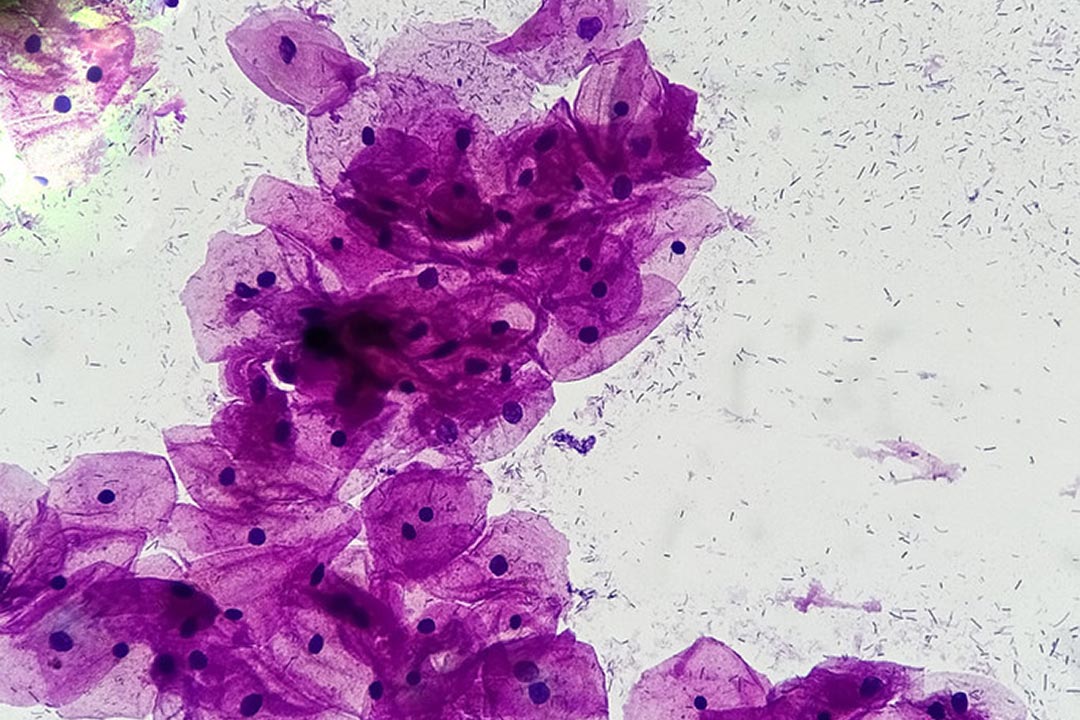
The floodwaters themselves provide another means through which antibiotic resistance can spread – by bringing bacteria into contact with antibiotic resistance genes in soil and wastewater. Floods can also help transfer resistant organisms to new locations.
Exposure to toxic heavy metals in polluted floodwater may further exacerbate this problem. Some bacteria have evolved resistance to heavy metals, and these metal resistance genes are often carried alongside antibiotic resistance genes in mobile genetic elements known as gene cassettes. Since metal-resistant bacteria are more likely to survive in polluted waters, this can also increase the abundance of antibiotic-resistant organisms.
4. Increased malnutrition
Extreme weather events such as flooding and droughts can lead to food shortages or food with low nutrition, leading to malnutrition. People who are malnourished have immune systems that are less well equipped to fight off infections, resulting in more frequent and severe bouts of disease, and an increased demand for antibiotics and other antimicrobials.
Research has suggested that children who are malnourished carry more multi-drug-resistant bacteria in their guts and are more prone to illnesses caused by them. Recent research in mice has also suggested that deficiencies in crucial micronutrients can lead to significant shifts in the bacteria, viruses and fungi living in their digestive systems, including an expansion of bacteria and fungi that can cause opportunistic infections. Nutrient deficient mice also harboured more bacterial genes that have been linked to antibiotic resistance.
Have you read?
5. Growing food insecurity
Climate change is expected to increase the prevalence of plant and animal diseases, placing additional pressure on food systems. Farmers and livestock producers have long used antimicrobial agents to prevent and treat crop and animal diseases, and boost yields. Climate change could further increase their use.
For instance, in rural areas around Bangalore in India, many agricultural farmers are switching to poultry rearing, as water shortages and higher temperatures affect crop productivity. Yet, higher temperatures also increase heat stress among broiler chickens, reducing their immunity and making them more susceptible to bacterial infections – increasing demand for antibiotics. Heat stress can also cause symptoms such as decreased appetite and diarrhoea, which less experienced farmers may mistakenly treat with antibiotics. Both situations increase the risk of antibiotic resistance developing.
A reduction in the effectiveness of antimicrobials to treat plant and animal diseases could affect the livelihoods of millions of farmers, pushing more people into extreme poverty. It could lead to food shortages and increased rates of malnutrition, further increasing demand for antibiotics to treat human diseases. Human health is also closely connected to the health of animals and our shared environment, with many existing and emerging animal diseases having the potential to transmit to humans.
Climate change and antimicrobial resistance present a serious and urgent threat to global public health and will require the shoring up of preventive measures, including routine immunisation and disease surveillance, to reduce the risk of outbreaks, particularly in low- and middle-income economies. Vaccines can also help to prevent antimicrobial resistance from developing in the first place by reducing rates of infection and reliance on antimicrobial drugs.