How do RSV symptoms differ from flu, COVID-19 and other respiratory viruses?
Symptoms of respiratory syncytial virus (RSV) are similar to those of other common respiratory viruses, but young children are more susceptible to severe illness. Here’s when to consult a doctor.
- 21 December 2022
- 4 min read
- by Linda Geddes

Respiratory Syncytial Virus, or RSV, is a normal childhood illness, but it is currently generating concern in many countries because it appears to be behaving abnormally. Usually, cases start to increase in Autumn, peaking in mid-Winter, before tailing off in late Spring. Since the arrival of COVID-19, however, this predictable pattern appears to have been thrown off-course.
RSV is extremely common; most children will have been infected by the age of two and may be reinfected many times during their lives. Usually, RSV infections are nothing to worry about, and resolve themselves within a week or two, but occasionally the virus can make children seriously ill.
According to the latest Communicable Disease Threats Report from the European Centre for Disease Prevention and Control (ECDC), a number of countries have detected an unusually early spike in infection, with increased paediatric hospital admissions reported in France, Ireland, Spain, Sweden and the US.
The Pan American Health Organization (PAHO) has also flagged significantly increased RSV infections that are burdening healthcare systems across Canada, Mexico, Brazil, Uruguay, and the US. Children and young infants are particularly affected.
Some of these countries, such as the US, have also experienced mini-surges in RSV infections during the summer months, when the virus is usually less active.
This unusual behaviour is thought to be due to increased contact among children in schools and childcare settings following the relaxation of COVID-19 restrictions, combined with far fewer people than normal having been exposed to RSV since the start of the pandemic. Though somewhat expected, "such large numbers of paediatric hospitalisations are putting stress on the paediatric healthcare sectors in several countries," the ECDC said.
RSV symptoms
Globally, RSV is a common cause of lower respiratory tract infections (those affecting the lungs and airways) in all age groups. Common symptoms include a runny nose, decreased appetite, coughing, sneezing, fever and wheezing. Because many of these symptoms are also seen in people with other respiratory illnesses, including common colds, flu and COVID-19, it can be difficult to tell them apart – although PCR tests are now available in some countries that can detect RSV, influenza and COVID-19 from a single nasal swab.
RSV is extremely common; most children will have been infected by the age of two and may be reinfected many times during their lives. Usually, RSV infections are nothing to worry about, and resolve themselves within a week or two, but occasionally the virus can make children seriously ill with pneumonia (an infection of the lungs), bronchiolitis (inflammation of the small airways of the lungs) or croup (an infection of the upper airway), which makes it harder to breathe.
Have you read?
High risk groups
Babies who were born prematurely, with a heart condition or who have a chronic lung condition are particularly vulnerable, but otherwise healthy infants and young children can also become severely ill – particularly during their first six months of life. In wealthy countries, roughly one in 56 babies who were born on time and are otherwise healthy, will be hospitalised with RSV during their first year.
Danger signs that should prompt parents to seek medical attention include:
-
Difficulty breathing – including a faster than normal rate of breathing and shorter breaths; the rib cage "caving in" with each breath; flaring of the nostrils with each breath
-
Abnormal respiratory sounds, such as wheezing, grunting or a high-pitched sound with each breath (stridor)
-
Coughing or wheezing that does not stop
-
Significantly decreased alertness or activity
-
Skin, tongue or lips turning blue or greyish
-
Symptoms of dehydration, .e.g. fewer than one wet diaper every eight hours
-
A fever in babies younger than three months, or fever that repeatedly rises above 40°C (104°F) for a child of any age.
RSV is also increasingly recognised as cause of severe illness and hospitalisation in older adults – particularly those with underlying heart or lung disease – pregnant women, and people with weakened immune systems.
Prevention
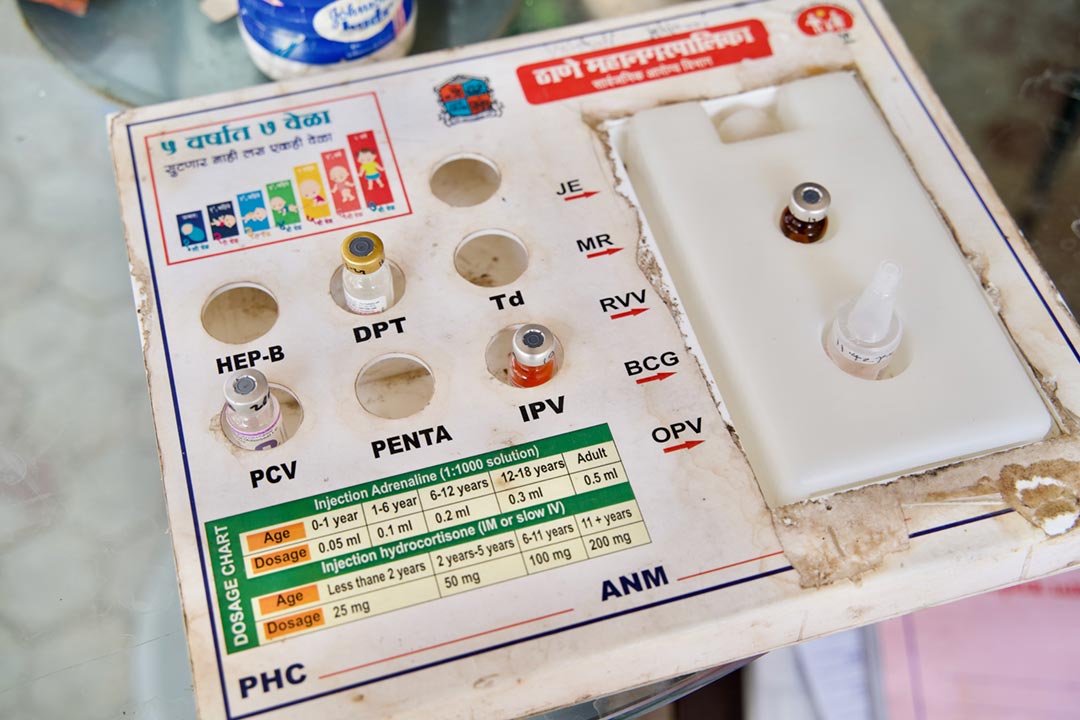
The good news is that a vaccine – or vaccines – against RSV is increasingly within reach, with several candidates currently in late-stage clinical trials. An antibody-based drug called nirsevimab, which is designed to protect babies during their first RSV season, was also recently granted worldwide approval by the European Commission, although it may be some time before it is widely available.
In the meantime, many of the same strategies that will reduce your risk of catching other respiratory viruses also apply to RSV. These include wearing a mask in crowded indoor spaces (although this can be difficult or impossible for young children and infants), frequent handwashing, coughing or sneezing into your elbow and staying home if you are sick. Those with suspected RSV – including children – should avoid contact with other individuals but be particularly cautious around infants and young children, pregnant women and older or vulnerable adults – particularly those with underlying heart or lung conditions.
More from Linda Geddes
Recommended for you