Mauritania now offers the six-in-one childhood vaccine. Here’s why that matters
It sounds like a small step, but it’s anything but: in July, Mauritania swapped out the five-in-one “pentavalent” vaccine for the hexavalent jab.
- 28 November 2025
- 8 min read
- by Yamina Bendaïda

In the heat of Nouakchott, mothers wait patiently with their infants. For them, every journey to the health centre is an effort – albeit a necessary one. Since 1 July 2025, the effort has become a little lighter.
Mauritania has added the hexavalent vaccine to its national immunisation programme: a major advance that brings protection against six serious diseases – diphtheria, tetanus, whooping cough, hepatitis B, Haemophilus influenzae type b (Hib) and polio – into a single injection.
Until now, children received the pentavalent vaccine (protective against five diseases), with a polio shot administered separately. Moving from several injections to just one goes far beyond convenience: it means greater efficiency, time saved and ultimately, improved equity.
In a country where the infant mortality rate stands at 28.5 deaths per 1,000 live births as of 2025, every improvement in vaccination coverage is a potential leap forward.
“The main objective is to reduce the number of injections and simplify the vaccination schedule,” explains Dr Mohamedou Mohamed Ahmed of the Expanded Programme on Immunization (EPI) at the Ministry of Health. “This simplification is a powerful lever to ensure that every child receives all the necessary doses on time.”
According to the latest World Health Organization and UNICEF immunisation coverage estimates, coverage with the recommended three doses of the diphtheria, tetanus and pertussis-containing vaccine – or DTP3, the conventional indicator for vaccine coverage, then administered as part of the pentavalent jab in Mauritania – reached 90% in Mauritania in 2024. Coverage for the inactivated polio vaccine (IPV) remained lower, at 67%. By combining these vaccines, the new hexavalent shot aims to close this gap and ensure that every child receives protection against all of these preventable illnesses.
Since their introduction into immunisation systems more than half a century ago, the basic DTP vaccines have saved over 40 million lives worldwide – a legacy that the hexavalent vaccine now continues and expands on.
“A more complete protection”
Tfarah, a state-registered nurse and mother of four, gave birth to her youngest child shortly after the hexavalent vaccine’s introduction. The child recently received the first dose of that shot at the Ksar Health Centre.
“During his second visit, the health workers explained to me that the new vaccine combines the ‘penta’ and the polio shot. One injection is enough to protect against six diseases,” she recalls.
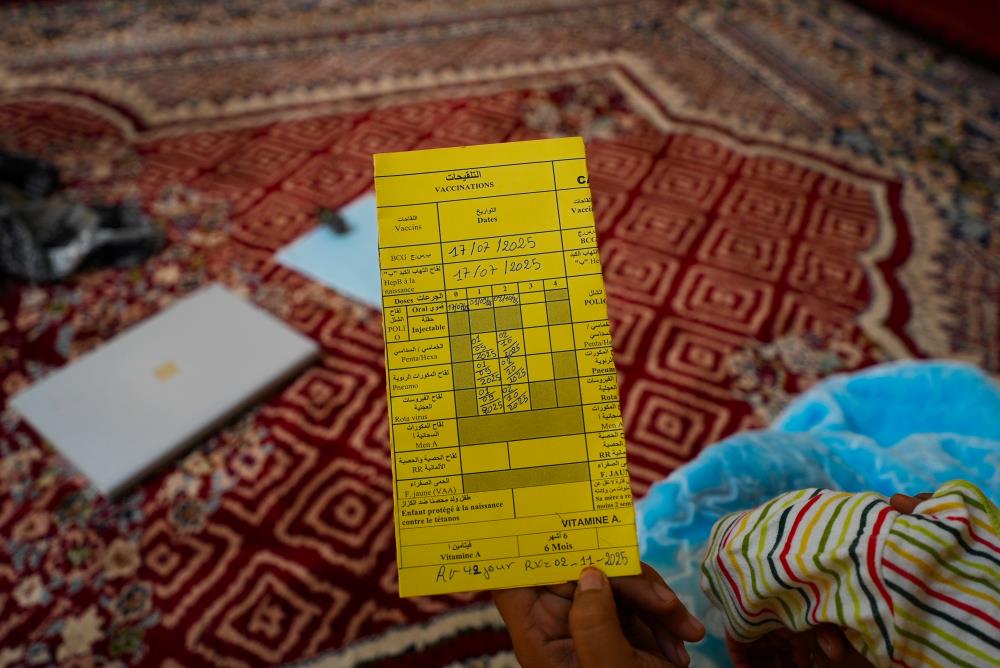
Credit: Yamina Bendaïda
Afterwards, she recalls, her baby had a slight fever and tenderness at the injection site in the thigh for a few hours – “as often happens after a vaccine” – but everything quickly returned to normal. “The doctors explained clearly that this was expected. Thanks to their explanations, I wasn’t worried,” she says.
Drawing on her professional experience, Tfarah also stresses the importance of proper technique. “When the injection is done correctly, there’s no problem,” she explains. “The nurses are well trained and know exactly how to ensure children are protected in the best possible conditions.”
Tfarah had learned about the hexavalent vaccine even before coming to the health centre. “I saw it on television, on Facebook, on the Ministry of Health’s page,” she explains.
Convinced of its importance, she spoke about it with the people around her. “With my sisters, friends, everyone. I told them the new vaccine offered more complete protection,” she says.
But reactions have been mixed. “Some still hesitate, worried that it’s six vaccines instead of five,” she acknowledges. “But others – those who are better informed – understand that it’s for the children’s well-being and that this stronger protection is essential.”
This hesitation among some mothers highlights the importance of awareness-raising. Tfarah’s message to other parents is crystal clear: “You must go to the hospital, ask questions, and really take care of your children’s vaccines, because it matters. I strongly encourage them to go.”
At Ksar Health Centre, a small change is a big change
The Ksar Health Centre, where Tfarah brought her son for vaccination, serves as the storage point for the entire moughataa, or district. Dr Sidi, the head physician, welcomes between 80 and 100 children every day for vaccination.
“Before, babies received two separate injections – the pentavalent and the inactivated polio vaccine (IPV). Now, one shot is enough to protect against all six diseases,” he explained in a recent interview.
“Mothers understand better now,” Dr Sidi continues. “Previously, parents felt there were too many injections. Today, they’re pleased: they save time, and their children get fewer shots.”
For Dr Sidi and his team, the hexavalent vaccine has also transformed the centre’s day-to-day operations. “We had a small fridge that couldn’t hold all the vaccines,” he recalls. “Now, our fridge can store everything.” This optimisation of storage space is crucial in a context where the cold chain remains a challenge, with national capacity at just 45%.
Reducing medical waste is another major benefit. In a centre vaccinating dozens of children every day, this reduction amounts to hundreds of syringes saved each month, easing staff workload and lowering environmental impact.

Credit: Yamina Bendaïda
And yet, the introduction of the hexavalent vaccine did not come without apprehension. “In the beginning, there were concerns about allergies or side effects,” acknowledges Dr Sidi.
A strong push on awareness-raising, led by the health workers themselves, quickly reassured families. In parallel, the EPI trained chief physicians and focal points in each moughataa, who in turn supervised their field teams.
“After two weeks, everyone was fully up to speed,” the doctor says with satisfaction.
Evidence of commitment
The introduction of the hexavalent vaccine was propelled, first and foremost, by the commitment of the Mauritanian government, which requested support from Gavi to make the transition, and is co-financing it in line with the Alliance’s co-financing model.
The Ministry of Health integrated the new vaccine into the national programme, organised training for health teams, and adjusted logistics across the moughataas.
Around this national investment of resources, technical partners played complementary roles: WHO provided technical support, UNICEF handled procurement and logistics, and Gavi facilitated access to the vaccine and supported the transition. “The funding request was submitted quickly, and the introduction took place on schedule,” notes Dr Ahmed.
For Dr Nasserdine of WHO Mauritania, the success stems from the strength of this coordination: “We did not observe any serious AEFIs, only minor and entirely normal effects. The introduction proceeded without major difficulty thanks to the government’s commitment and the joint work of all partners.”
Have you read?
Towards polio eradication – and beyond
This new vaccine is a cornerstone of the global strategy to eradicate poliomyelitis. By integrating the inactivated polio vaccine (IPV) into a single shot alongside other essential vaccines, Mauritania increases the likelihood that children receive full protection. The country has not reported a case of wild poliovirus since 2010, but vigilance remains crucial. The hexavalent vaccine is a critical safeguard against any resurgence.
At the official launch ceremony on 30 June 2025, Dr Charlotte Faty Ndiaye, WHO Representative in Mauritania, described the introduction as “progress that saves lives, strengthens health systems and demonstrates strong political commitment.” She also reminded participants that challenges remain, especially in reaching zero-dose children – those who have not received any vaccines at all.
To serve its entire population, Mauritania relies on three vaccination strategies: fixed sessions in health centres, outreach sessions for communities located five to ten kilometres away, and mobile teams in 4x4 vehicles to reach the most remote areas. In this context, the simplification brought by the hexavalent vaccine is invaluable.
Despite ongoing obstacles – limited communication in rural areas, a constrained cold chain, and the need to reach zero-dose children – the momentum is positive. Mauritania is, alongside Senegal, one of the first low-income countries worldwide to have made the switch to the hexavalent formulation, and experts say this marks a decisive step toward vaccine equity. After more than 20 years of use in high-income countries, this combined vaccine is finally accessible to the children who need it most.
As nurse Tfarah says, vaccines really matter. They are the promise of a healthier future – now with fewer injections for every life protected.
This article is translated from the French. Read the original





