Why we still need R&D into COVID-19 vaccines
There are now 17 COVID-19 vaccines approved for emergency use, but as the virus continues to evolve, here is why we can’t pull the plug on research into new vaccines and therapeutics.
- 16 June 2021
- 4 min read
- by Priya Joi
By any measure, the roll-out of more than a dozen safe and effective vaccines against the pandemic virus - with more on the way - has far surpassed what scientists predicted as possible a year ago. But now that there are so many, with a diverse mechanisms of action, why should we continue supporting research into COVID-19 vaccines?
Staying ahead of new variants
One of the biggest issues the world is facing as the pandemic continues to rage is the emergence of new variants. Concerns have been raised over whether the emergent variants could evade the vaccines, and although the vaccines seem to be largely protective so far, people do need to have had two doses to be well protected against the Delta variant. The virulence of this variant might mean that people need an additional booster dose, too.
R&D into vaccines and medicines needs to go hand in hand with innovative ways of creating sustainable surveillance, detection and manufacturing capacity.
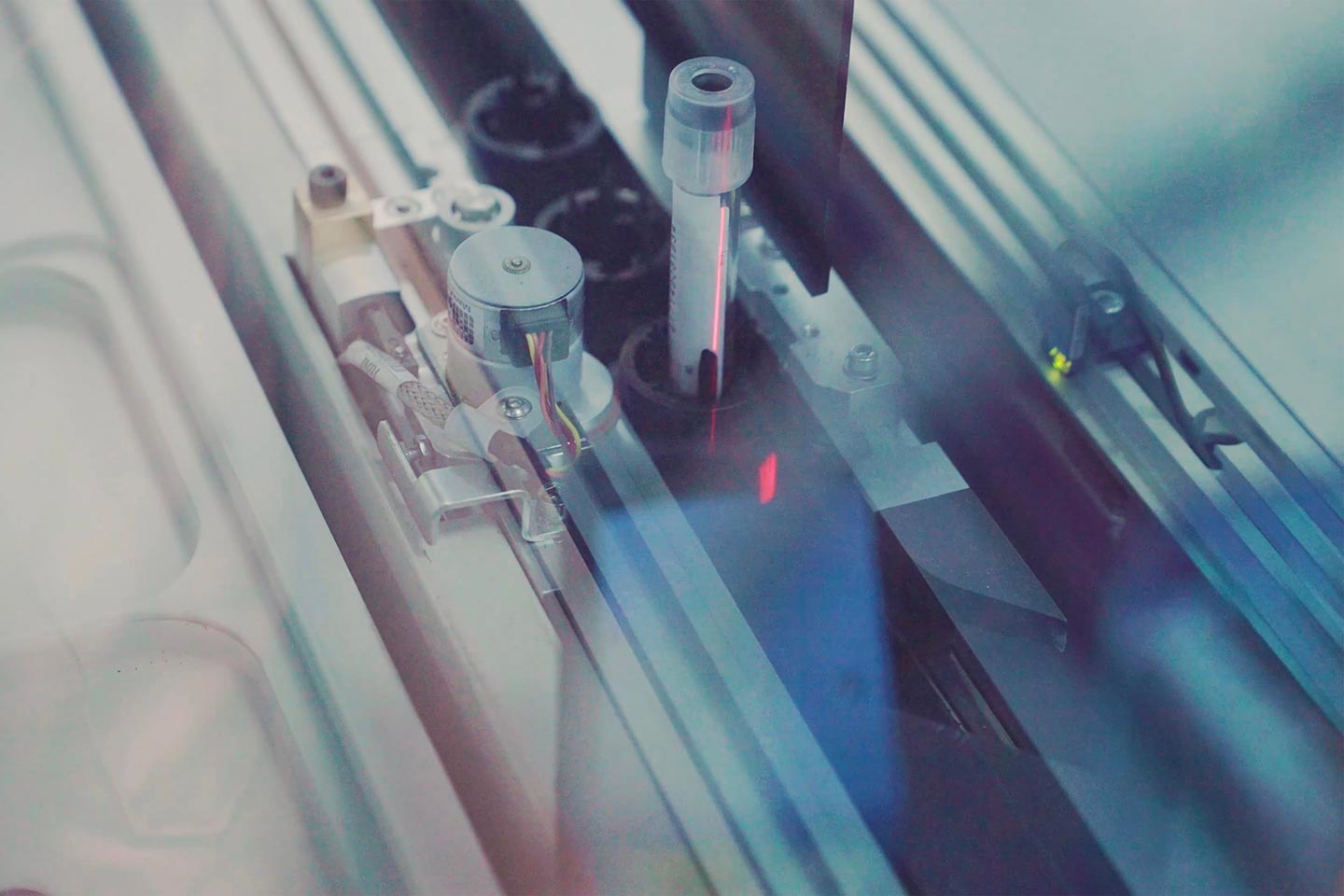
To stay ahead of new variants, CEPI (the Coalition for Epidemic Preparedness Innovations) has set up a network of laboratories to assess how well COVID-19 vaccines work against variants of concern, and is supporting R&D into vaccines specifically targeted to these variants. The scientific community, meanwhile, has set itself an ambitious goal of getting new vaccines developed and tested within 100 days. If this becomes reality, it would mean tackling new variants faster than ever before, potentially stopping them in their tracks.
Next-gen vaccines could work in different ways
Scientists developing the next round of vaccines are planning to make them better than the first round in a variety of ways. Novavax’s vaccine, which took a long time to come close to approval, can be stored long-term in a fridge, giving it an advantage over vaccines that have short shelf-lives or that need the ultra-cold freezers that many low and lower middle income countries don’t have.
Have you read?
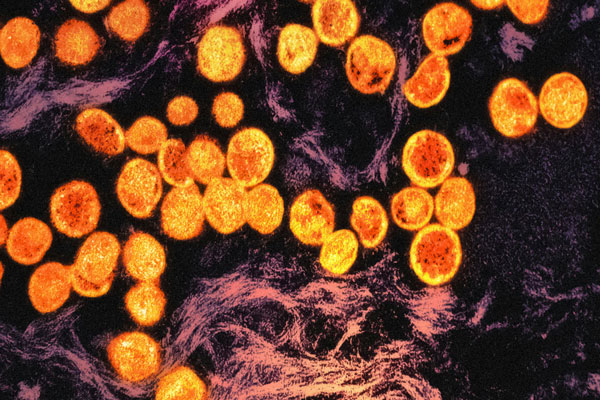
Valneva’s vaccine uses a whole inactivated virus, which the vaccine makers say could offer it an advantage over vaccines that target the spike protein. Should a new variant develop a mutation in that spike protein, existing vaccines may not be able to successfully target it anymore. Essentially, a whole-virus approach offers several targets for our immune systems to aim at.
German biotech CureVac is making a new version of its vaccine that demands a lower dose, opening the door to combination jabs targeting different variants in a single shot.
Other vaccine makers are trying to eliminate the need for injected vaccines. ImmunityBio is developing a vaccine that can be injected, but is also testing three other different delivery systems – a nasal spray, a pill that dissolves under the tongue, and a capsule. Vaxart is also trying to develop an oral vaccine. Any vaccine that is easy to administer and doesn’t require refrigeration or freezing could hugely ease rollout in low and middle income countries.
Building surveillance systems that can surge in emergencies
When the pandemic started, large-scale rolling surveillance of COVID-19 transmission was possible because the widespread influenza surveillance network that existed across the world, including across Asia and Africa, was able to be adapted to monitor the new coronavirus. Yet these systems became overwhelmed by demand, and although rates of flu transmission fell amid lockdowns and restrictions, as the world opens up again, rates of flu will rise too.
Manufacturing capacity for other vaccines also pivoted to produce COVID-19 vaccines - yet these production pathways, too, became overwhelmed. R&D into vaccines and medicines needs to go hand in hand with innovative ways of creating sustainable surveillance, detection and manufacturing capacity. This type of pandemic preparedness, designed for COVID-19, could also create surge capacity for the management of future pandemics, as even while we continue to fight the coronavirus, the next pandemic is a certainty.