COVID: why some people with symptoms don’t get tested
Recent research found around a quarter of people with classic COVID symptoms didn't get tested.
- 25 January 2022
- 4 min read
- by The Conversation
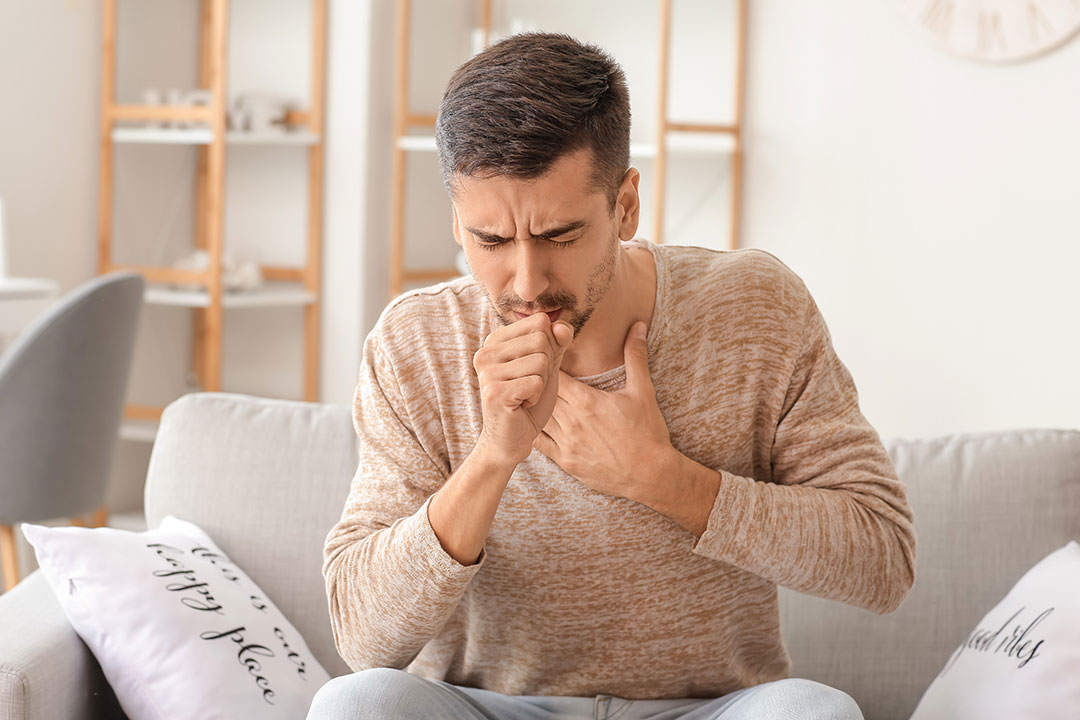
Testing people with COVID symptoms has been a pillar of the UK’s pandemic response, reducing transmission by identifying and isolating those with the virus. But to be effective, it relies on people with symptoms getting tested, which raises an obvious question: what proportion of symptomatic people actually take a test?
The ZOE COVID Study, which is funded by the government and run by a group including King’s College London and the city’s Guy’s and St Thomas’ hospitals, is uniquely positioned to answer this question. Each day more than 4 million participants in the UK report any symptoms they are feeling via the study’s app, and record the results of any recent COVID tests.
Testing rules have evolved during the pandemic, but one rule has remained consistent: if you have one of the main three symptoms of COVID listed by the NHS (fever, a persistent new cough, or loss of taste or smell) but don’t otherwise know if you have the virus, you should take a PCR test. And by analysing the study’s data, my colleagues and I have been able to see what proportion of participants experiencing any of these symptoms then go on to have a test shortly after their symptoms appear.
The results were surprising. In December 2020 we found that 25% of those who reported one of the three core symptoms didn’t report a PCR result shortly afterwards, suggesting they weren’t getting tested. This was despite there being plenty of spare testing capacity at the time.
Armed with this information, we then sent out a survey to a sample of 4,000 users in the UK who had had symptoms but no test, to better understand why they didn’t get tested. We found this was mostly down to three reasons.

Firstly, people were less likely to get tested if they had only one of the three symptoms or if their symptoms lasted only a day. This suggests people might have the erroneous view that their illness is unlikely to be COVID if their symptoms are brief or mild.
We also found that 40% of our respondents couldn’t identify all three of the symptoms that qualify you to get a COVID test. Older groups were less likely to know: 80% of respondents aged 25-34 could identify all three symptoms, but just 25% of those 75 and over could.
Have you read?
Plus, even when individuals knew they should get a test, we found they weren’t always able to. Of those that wanted but failed to get one, the most common reason provided was, “I did not know where to go in order to get tested”. Other common reasons were “I was not able to get to a testing location” and “I tried to get a test but was not able to get one”.
Together, these results demonstrate that knowledge is often a barrier to getting tested for COVID. People may not know that their mild illness could still be COVID, they may not realise that their symptoms mean they should get a test, and even if they want a test, they may not know how to get one.
Expanding the symptom list
These findings could have big consequences. It’s important that we identify and isolate as many cases of COVID as possible to help reduce the spread of the disease. People that don’t get tested may continue their daily lives, unwittingly infecting people at home and at work.

Our results show that educating the public is crucial for increasing test take-up. Efforts need to be made to inform the public that even mild symptoms can be COVID, to teach them what these symptoms are, and how they might get tested. It might help to target this messaging at older populations, who are less likely to know what symptoms qualify them for a test.
Recently, there have been calls to expand the list of symptoms that qualify someone for a COVID test, based on evidence that with variants such as omicron and delta, many infected people have symptoms other than the core three. While this approach may be sensible, our results indicate that extensive efforts will be needed to educate the public about any new set of symptoms to ensure that people experiencing them do get tested.![]()
Authors
Mark Graham, Research Associate in Health Data, King's College London

This article is republished from The Conversation under a Creative Commons license. Read the original article.
Disclosure statement
Mark Graham receives funding from the Wellcome Trust.
Partners

King's College London provides funding as a member of The Conversation UK.