The Viral Most Wanted: The Coronaviruses
Seven members of the Coronavirus family are already known to infect people, often with deadly consequences. Disease investigators fear that more new and dangerous Coronaviruses could spill over at any time.
- 14 December 2023
- 10 min read
- by CEPI

It was a Saturday in September 2012 when an unusual email arrived at a British infectious disease laboratory from a team of virologists in the Netherlands. Its contents unnerved the London-based scientists, even though they were among some of the world's most experienced virus handlers.
The email contained details of a mysterious viral pathogen that had been found in two patients many miles apart. One was a Qatari man who at that time was in an intensive care unit at a British hospital. The other was an elderly Saudi Arabian man who had recently died in a hospital in Jeddah after suffering a severe bout of pneumonia and then renal failure.
Intrigued, the viral detectives set to work on deciphering the pathogen's identity. Within days the new virus was confirmed as one never seen before in humans. It was a novel Coronavirus—later to become known as the virus that causes Middle East Respiratory Syndrome, or MERS.
MERS was the second of three highly pathogenic novel human viruses in the Coronavirus family to emerge in the first quarter of the 21st Century. The first, SARS-CoV-1, caused a disease known as Severe Acute Respiratory Syndrome, or SARS. And the third, SARS-CoV-2, caused a disease called COVID-19, which swiftly became a global pandemic. The relatively frequent emergence of novel viruses in this family that can cause outbreaks of severe illness in people shows that Coronaviruses are a deadly force to be reckoned with. They are what make the Coronavirus family one of The Viral Most Wanted.
One Big Close-Knit Family?
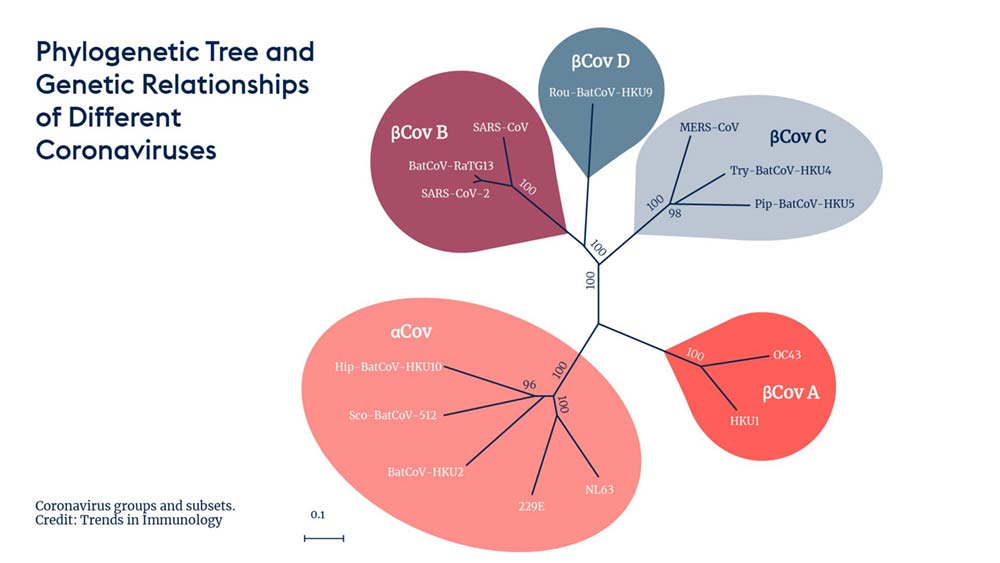
The Coronavirus family is certainly very big, with hundreds of viral relatives within it. It is divided into four sub-groups, each with certain unique characteristics and traits. The sub-groups are known as the Alphacoronaviruses, the Betacoronaviruses, the Gammacoronaviruses, and the Deltacoronaviruses. The most notorious Coronaviruses that cause human disease belong to the Alphacoronavirus and Betacoronavirus sub-groups.
Prime Suspects
There are currently seven known Coronaviruses with the ability to cause illness in people, and disease surveillance specialists fear new Coronavirus suspects could emerge at any time. Studies have found that more than 100 Coronaviruses circulating in animals have the potential to spill over into people. The risk of another novel Coronavirus—often referred to as a 'Coronavirus X'—is ever-present.
The current ultra-prime suspect within the Coronavirus family is its newest known member—SARS-Cov-2, the virus that causes COVID-19. This virus sparked a devastating pandemic in January 2020 which is still now claiming victims every day across the world.
MERS-CoV, the novel Coronavirus that emerged in 2012 and is the cause of MERS, is another key suspect and one that disease detectives are keeping very close track of.
While SARS-CoV-1 was a prime suspect in the early 2000s, its activity has dwindled to nothing since 2004, giving investigators hope that the threat it poses to human populations has waned significantly.
Nicknames and Aliases
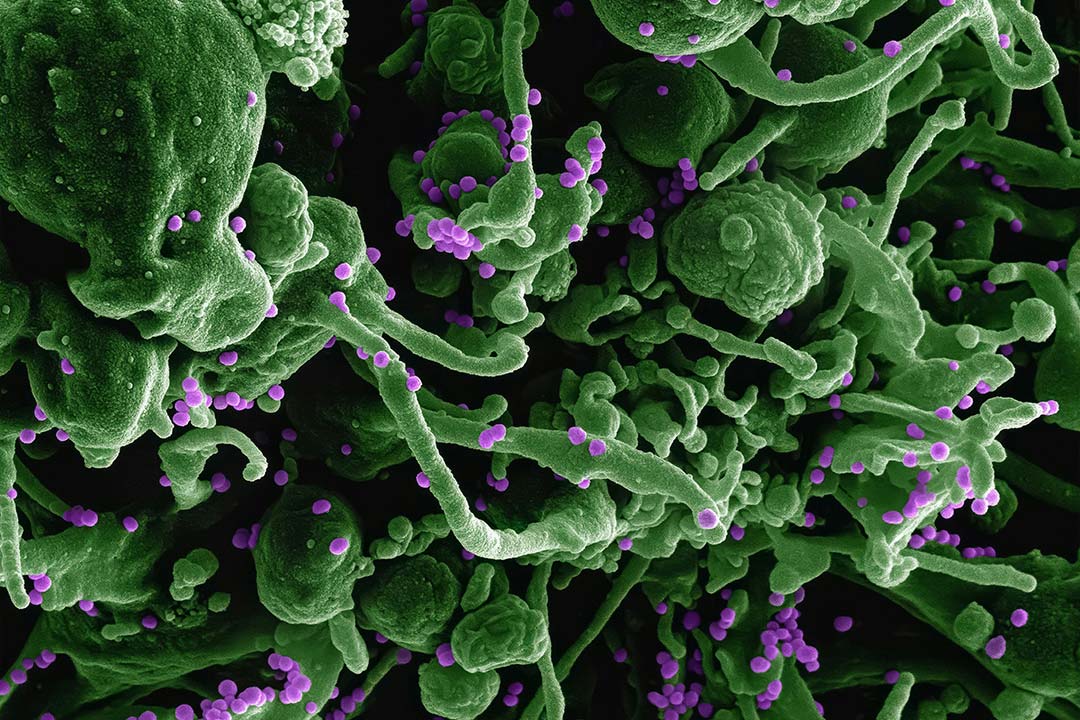
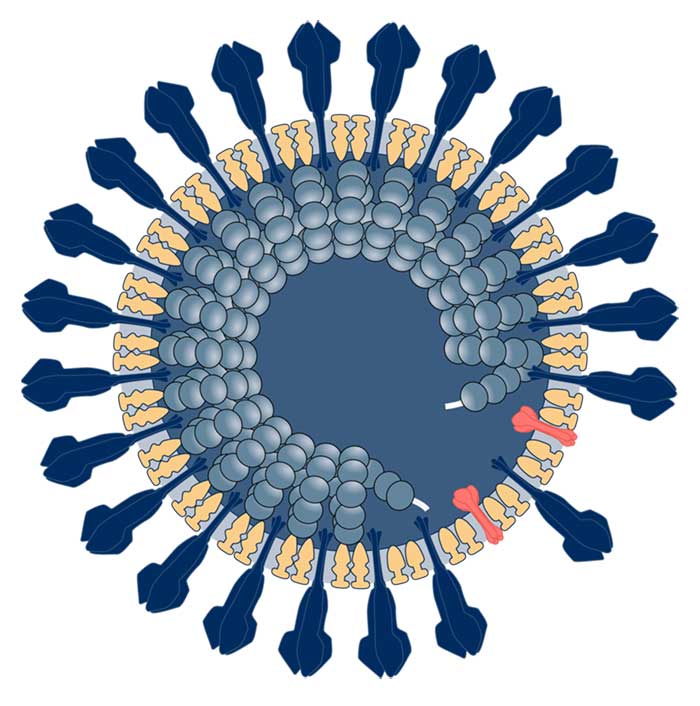
The name Coronavirus is derived from the Latin 'corona', which means 'crown' or 'halo' and describes the crown-like circles of protruding spikes that give Coronaviruses their distinctive appearance.
MERS, or Middle East Respiratory Syndrome, was named after the region where it was first identified, while SARS, or Severe Acute Respiratory Syndrome, became known by its acronym.
Coronaviruses that cause common colds with mild to moderate upper-respiratory tract infections in humans are known by the code-names 229E, OC43, NL63 and HKU1.
Distinguishing Features
Coronaviruses are large, enveloped viruses with a positive-sense, single-stranded RNA genome. The viral particles, or virions, are spherical in shape and have a crown-like appearance due to spike proteins protruding from their lipid coatings.
Modus Operandi
Coronaviruses use their spike proteins, also known as S proteins, to attach to receptors in host cells. In humans, the primary host cell receptors for SARS-CoV-2 are known as angiotensin-converting enzyme 2, or ACE2, receptors.
One feature of Coronaviruses that makes them particularly tricky for disease fighters to combat is that, because they are RNA viruses, they frequently mutate, or "shape-shift" and spawn new variants. The mutated variants of the original SARS-Cov-2 virus that sparked the COVID-19 pandemic were often able to evade the antibody defences people had developed against previous infections.
The MERS Coronavirus, MERS-CoV, also attaches to human cell receptors known as dipeptidyl peptidase 4, or DPP4 receptors. These receptors are found on the surface of cells in the airways and in the lungs, as well as in the kidneys.
Accomplices
Bats are known to be the major animal reservoir for many Coronaviruses, with the MERS and SARS viruses both widely considered by scientists to have originated in one of several species of bat.
Besides bats, camels, cats, pangolins and many other types of animals, particularly mammals, have also been identified as also being susceptible to Coronavirus infection. This makes them all potential accomplices, or intermediaries, in the original transmission of new Coronaviruses into human populations.
Have you read?
Investigators looking into the origins of the human MERS Coronavirus emergence in 2012, for example, found that one-hump camels—also known as dromedary camels—were the most likely intermediary host as the virus jumped from bats into people.
Explorations into where and how the 2003 SARS outbreak began have zeroed in on a mammal called a masked palm civet cat as the most likely accomplice in that virus jumping from bats and evolving into a human Coronavirus.
Common Victims
The virus that causes COVID-19 can infect anyone, but is less serious as an infection in children than it is when it attacks adults and older people. The disease is often more severe in people who are over 60 years old, or who have health conditions like lung or heart disease, diabetes, or conditions that affect their immune system.
MERS-CoV can also infect anyone, but has been found more frequently in people who work with or have contact with camels. The disease appears to spread more easily among people who are in hospital or other healthcare facilities—including healthcare workers such as doctors and nurses who come into close contact with MERS patients. Infection control experts caution that people with diabetes, kidney failure or chronic lung disease, as well as people who have weakened immune systems, are more vulnerable to MERS-CoV infection than others.
Those most severely affected by the outbreak of SARS in 2003, in which more than 8000 people worldwide were struck by the disease, were primarily adults over 60 years old. The death rate in this age group was almost 50 percent. Meanwhile, children below the age of 12 were far less seriously affected, suffering mostly mild symptoms and recovering more quickly.

Infamous Outbreaks
COVID-19
The COVID-19 pandemic began in January 2020 and had killed almost seven million people across the globe by the time the World Health Organization declared in May 2023 that its most acute and deadly phase was over.
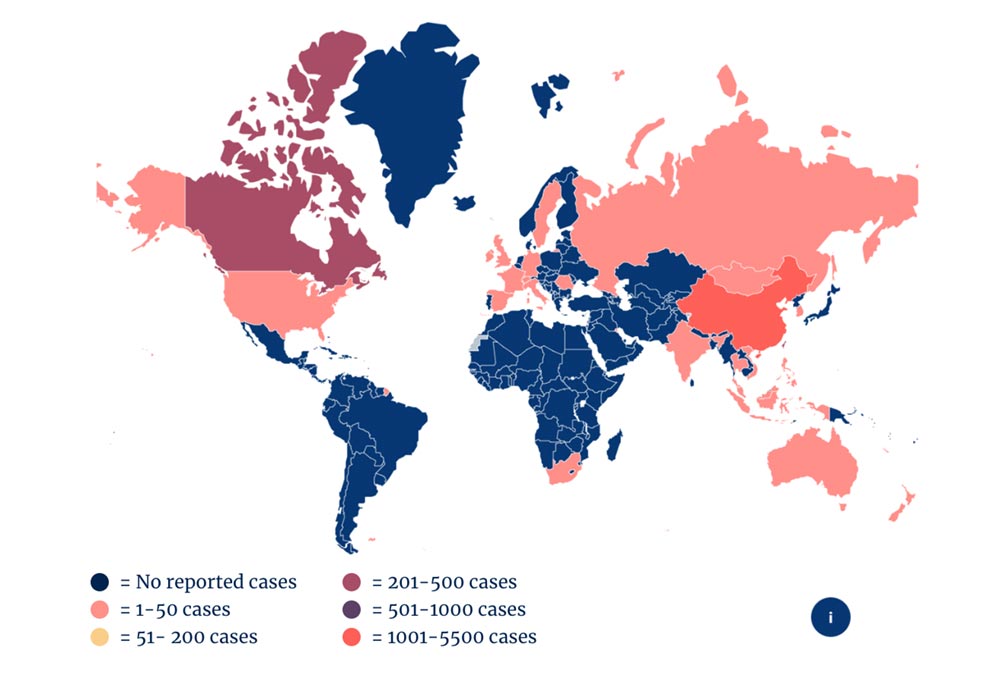
The pandemic was the deadliest in more than 100 years, with the SARS-CoV-2 virus and multiple variants of it continuing to circulate and spread in wave after deadly wave of infection. The pandemic caused hundreds of millions of COVID-19 cases and affected people in every country in the world for more than three years.
The COVID-19 catastrophe was also estimated to have cost the world up to $28 trillion in economic losses.
MERS
After MERS first emerged in Saudi Arabia in 2012, it spread in a slowly-growing but highly-deadly epidemic. That epidemic, which has affected at least 27 countries in more than a decade, has so far infected more than 2,600 people and killed at least 938 of them.
The largest outbreak of MERS outside of the Arabian Peninsula region erupted in South Korea in 2015. Disease detectives later discovered that the so-called 'index case' for the Korea outbreak was a business traveller who had been in Saudi Arabia. The subsequent wave of infections began primarily in healthcare workers and people who had come into close contact with them, and eventually spread to infect almost 200 people, killing at least 38 of them.
SARS
Severe acute respiratory syndrome, or SARS, was the first severe and readily transmissible new disease to emerge in the 21st century. It was detected in China in February 2003, but investigators believe it had probably been circulating and causing death and disease for at least a few months before then.
The virus spread in an epidemic of disease that ultimately affected 29 countries across the world, including in Asia, Europe, North America and South America. The outbreak killed almost 800 people worldwide, and was contained by late July 2003.
Since 2004, there have not been any known cases of SARS reported anywhere in the world.
Common Harms
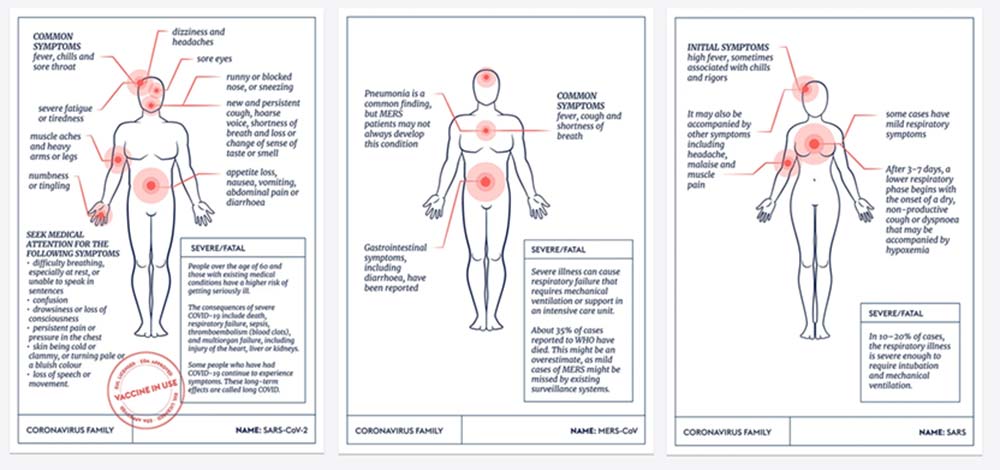
As many people in the world have learned since January 2020, infection with SARS-CoV-2 can cause a vast range of symptoms—from a slight cough with headache, loss of senses of taste and smell and mild fatigue, to extremely severe and acute respiratory distress resulting in lung and heart damage, respiratory failure, septic shock, pneumonia, heart failure, multiorgan failure and death. Many people suffer repeat infections with the virus, in part because it has continued to mutate and evolve, with the ability to evade antibody defences mounted against previous infections.
As many as 10 to 20 percent of survivors of COVID-19 can suffer longer-term complications, a syndrome known as "long COVID". Symptoms can include persistent and debilitating fatigue, bouts of heart and respiratory problems, and neurological symptoms such as brain fog, short-term memory loss and inability to concentrate.
Victims of MERS-CoV infection often suffer initial symptoms of fever, cough and shortness of breath. Many also develop pneumonia, and some also suffer gastrointestinal symptoms, including diarrhoea. Severe MERS-CoV infections can cause respiratory failure that can be fatal. The virus appears to cause more severe disease in older people, people with weakened immune systems and those with chronic diseases such as kidney disease, cancer, chronic lung disease, and diabetes.
The case-fatality rate for MERS is the highest of all the known human Coronaviruses, at around 35 percent. Investigators say, however, that this may be an overestimate of the true mortality rate, since there may be milder cases of MERS-CoV infection that are not being picked up by surveillance systems and are therefore not recorded.
People infected with the SARS-CoV-1 usually develop a high fever and suffer chills, headache and body aches for a few days to begin with. SARS symptoms can then progress to a dry, non-productive cough and, in more serious cases, to oxygen levels in the blood dropping to dangerously low levels—a condition known as hypoxia. Most SARS patients develop pneumonia, and almost 10 percent of those infected during the 2003 outbreak died.
Lines of Enquiry
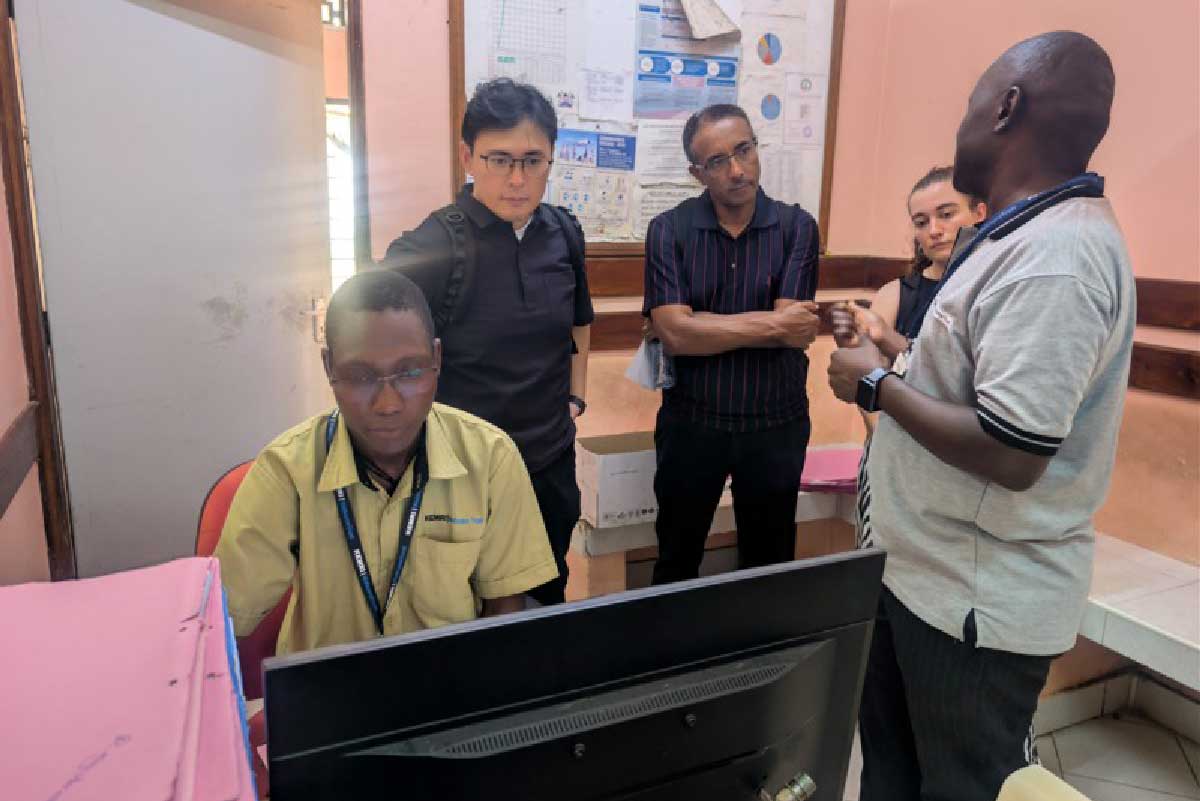
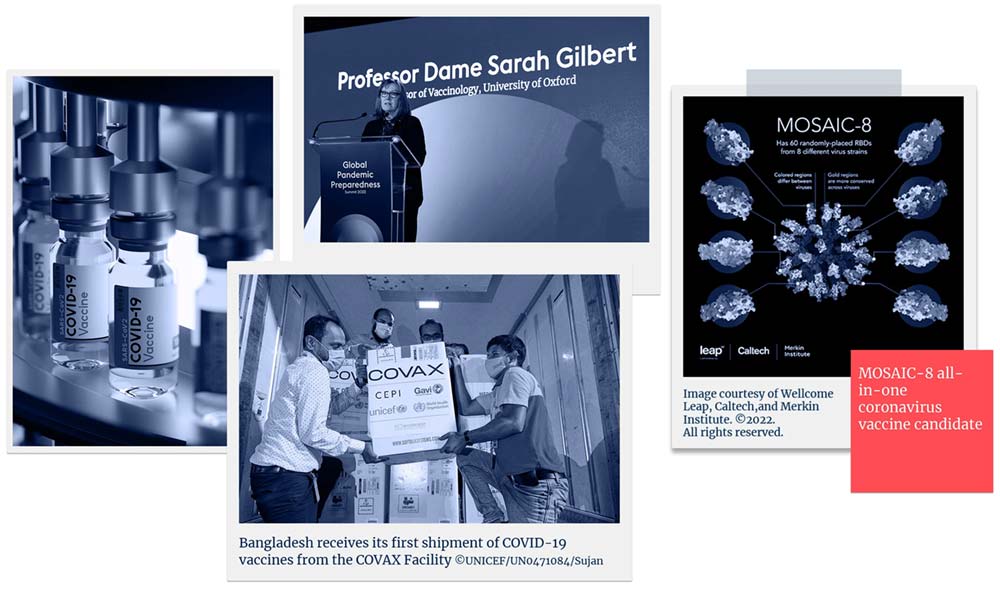
Largely due to the devastating extent of the COVID-19 pandemic, thousands of disease detectives around the world are working on a whole range of ways of combating or defending against outbreaks of infection by members of the Coronavirus family, and in particular the sarbecoviruses, which include SARS-CoV-1 and SARS-CoV-2 and its variants. These multiple lines of enquiry mean that as of March 2023 there were more than 380 COVID-19 vaccines either licensed or in development. In response to the pandemic, CEPI swiftly established one of the world's largest COVID-19 vaccine portfolios, seven of which have been licensed for domestic or global use, and co-led the COVAX initiative which has delivered almost 2 billion vaccines to countries around the world.
While interest in and funding for investigations into how to stop the MERS-CoV infecting and killing people began to wane after the initial epidemic in the Middle East appeared to be petering out, there are still several international teams of scientists working on developing defences against it. MERS-CoV is also designated as a priority pathogen—in other words, a prime suspect—by CEPI and by the World Health Organization. CEPI has supported the development of four MERS-CoV vaccine candidates, two of which are in clinical trials.
A major focus of disease defence efforts against this viral family is seeking ways to protect people against multiple members of it at the same time— a broadly protective Coronavirus vaccine.
The ultimate win—the "Holy Grail" of this disease detective work—would be all-in-one vaccines that target multiple Coronavirus culprits and can also pre-empt the emergence of new viral variants and sub-variants of the prime suspects, all at the same time.
That is a significant scientific challenge, which CEPI has embraced by supporting 13 projects so far, each one exploring a distinct way of designing a vaccine that could be broadly protective against more than one Coronavirus.
Website
This article was originally published by CEPI.