COVID vaccine is being speeded up but urgency cannot be at expense of safety, says Dr Seth Berkley
As CEO of Gavi, the Vaccine Alliance funded largely by Bill Gates, Dr Seth Berkley has helped vaccinate almost half the world’s children from fatal and debilitating diseases. His current baby is the COVAX Facility to help develop, manufacture and secure doses of Covid-19 vaccines for 92 low and middle-income economies, including India. He speaks to Bachi Karkaria on the hope and hurdles.
- 14 September 2020
- 8 min read
- by Dr Seth Berkley

Q. What has been the main challenge in producing vaccines against this novel coronavirus?
Clearly, the science. This is a new organism, only discovered about nine months ago. Yet, scientists have responded quickly with over 200 vaccines in development and 34 already in clinical trials. Based on previous vaccine development, those at the preclinical stage have less than 10% chances of reaching the final licencing stage. If they make it to clinical trials, the odds improve twice over. Of course, no one knows for sure if these projections will apply to COVID-19 vaccines. Even though so many are already in clinical trials, we still don’t know which will succeed. This is why it’s important to move forward with a broad portfolio.
Q. How can a global platform like Gavi work vis a vis rampant vaccine nationalism?
Yes, this is a major challenge with countries signing bilateral deals with manufacturers. It could lead to what happened in 2009 with swine flu when some countries cornered most of the supply, leaving the rest of the world vulnerable. Fortunately, most countries have also signed up for the COVAX Facility, led by Gavi and Coalition for Epidemic Preparedness Innovations (CEPI). I can say that this is the only truly global solution to this pandemic. It will pool resources from participating countries to scale up manufacturing, and then ensure that each of these countries gets rapid, fair and equitable access to COVID-19 vaccines once they are available, regardless of its economic capacity. With nine vaccines already supported and a further nine being evaluated by CEPI, COVAX has the world’s largest and most diverse actively-managed portfolio of COVID-19 vaccine candidates. But we will be seeking to work with manufacturers of promising candidates anywhere. I think countries recognise our reach. Many that have entered into bilateral dealshave still committed to join the COVAX Facility. The two are not mutually exclusive.
Q. Is the recent setback to the front-runner AstraZeneca vaccine trial worrying? And is fast-tracking a politer phrase for cutting corners - recklessly?
No vaccine at the clinical stage can be anointed a ‘front runner’, because, as this has shown, it’s not over till it’s over. This happens with clinical trials, but doesn’t make headlines. If anything, it should reassure us that that robust monitoring and safety checks are totally in place. Undeniably, the speed at which the scientific community and manufacturers have responded has been breath taking. But let me emphasise that safety is the number one priority in the development, testing and regulatory approval of COVID-19 vaccines. Normally these processes can take more than a decade. We’re trying to get there within an 18-month time-frame by doing things in parallel rather than sequentially. But when we accelerate the clinical trials and regulatory processes for these candidates, the same rigorous safety standards are being applied.
Q. How have time savings been achieved?
First, through the preclinical stage, we have moved candidates forward really quickly without spending too much tinkering around. Then in the clinical trial stage by carrying out adaptive clinical trials, effectively modifying them as we go, adding those from different risk groups and carrying out different phases almost in tandem. This can shave years off this stage. Similarly, fat can safely be trimmed off some regulatory processes. But arguably, the most important time-savings will be in manufacturing.
The most important time-savings will be in manufacturing.
Please elaborate.
Normally companies are reluctant to invest in large-scale production facilities until their vaccine has received regulatory approval. If this were to happen with COVID-19 vaccines, delay and shortages, initially at least, would only prolong this acute phase of the pandemic and take an avoidably huge toll of lives. The COVAX Facility aims to prevent that by creating incentives for manufacturers to invest in production capacity beforehand. This way we will hit the ground running and start making large number of vaccine doses available very soon after approval. Let me reiterate, none of this will compromise safety; the only risks here are financial. But given that this pandemic is costing the global economy US$ 375 billion a month in lost GDP, such at-risk investments are a small price to pay.
Q. The COVAX Facility aims to deliver at least 2 billion vaccines by the end of 2021; how will you decide where the vaccines go, and who gets them?
This is an important question. Through the COVAX Facility, all participating countries will get access to COVID-19 vaccines, as doses become available, at the same time, regardless of their ability to pay. Those that cannot afford them will gain access by having their participation in the Facility supported by the Gavi COVAX Advance Market Commitment, a financing mechanism which will be paid for largely through Official Development Assistance. Even so, initially at least, demand is expected to outstrip supply. So the question of which individuals should be first in line, is important. The World Health Organization is working on a framework for COVID-19 vaccine allocation which will play a role in how the COVAX Facility distributes vaccines. We have to ensure that everyone who is at equal risk has the same equal opportunity to be vaccinated.
Q. What is the greatest leap in biotechnology/AI which has brought us so close to achieving what was inconceivable a decade ago: discovering and manufacturing a vaccine against a previously unknown virus rapidly enough to help end a prevailing pandemic?
In some ways, the drive to develop COVID-19 vaccines may actually trigger a new, and much needed, era in vaccine innovation. The fact that scientists were able to genetically sequence the SARS-CoV-2 virus, which causes COVID-19, so quickly is perhaps one such technological innovation. This allowed research groups to develop vaccine candidates at record speed. That said, most of the technologies now being developed for COVID-19, including highly innovative approaches like mRNA and DNA vaccines, have actually been around in one form or another for a considerable time – although none have yet been licensed.
Have you read?
Q. How will Gavi ensure the essential cold chain for delivery around the world?
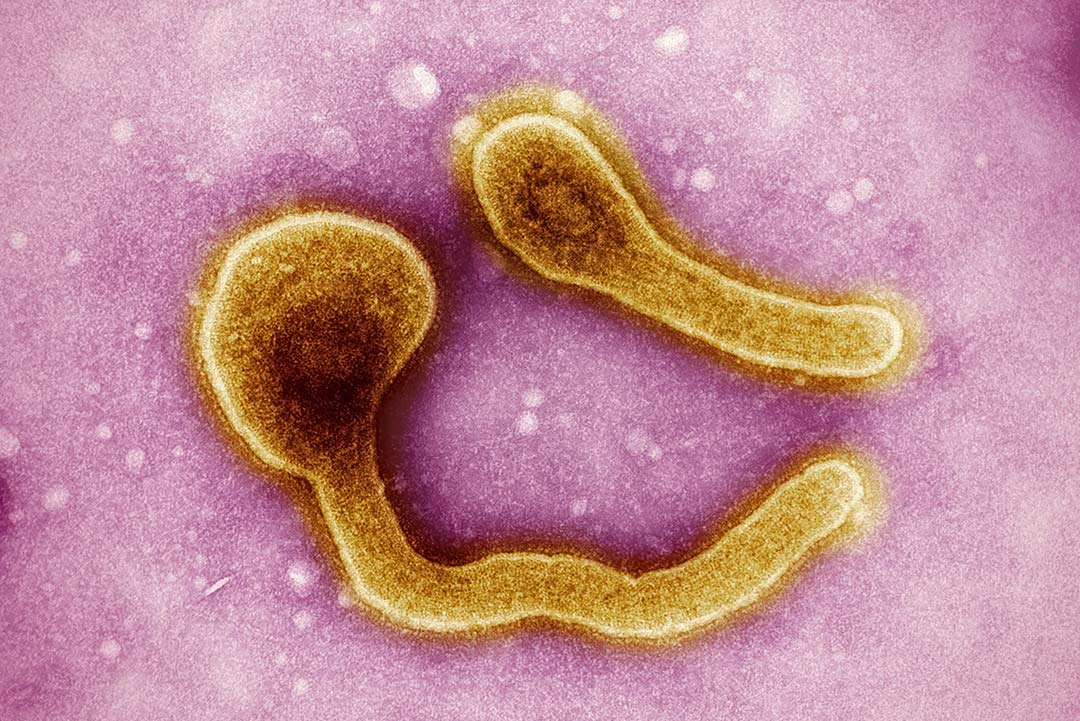
There’s huge variety in the kinds of COVID-19 vaccines under development, and yes a small number may require what we call ultra cold chain, with storage as low as at -80 degrees Celsius -- well beyond traditional refrigeration units. If any of do succeed and get licensed, it may well create deployment challenges, but not insurmountable ones. The vaccine that so successfully help stop the spread of Ebola in the Democratic Republic of the Congo also requires ultra cold chain. If we could manage to deploy it in the midst of a major epidemic and war, I think we can handle it with COVID-19.
Q. Wasn’t that vaccine manufactured by Serum Institute of India? Tell us about your partnership with this company.
Gavi already helps vaccinate half the world’s children, more than 820 million since it was created in 2000, and this has helped prevent more than 14 million deaths. As the world’s largest vaccine manufacturer by volume, SII has played an vital part in helping us achieve that. During this pandemic, it has once again stepped up to the plate, with a new agreement to provide 100 million doses of COVID-19 vaccine for low- and middle-income countries, through Gavi’s COVAX AMC.
Q. How are your efforts to tackle SARS-CoV-2 different than that of your frontline role in trying to find a vaccine against HIV?
They couldn’t be more different. Developing a vaccine for HIV was and still is monumentally challenging because the Human Immunodeficiency Virus is an intensely quick-moving target. In contrast, with this novel coronavirus, the genetic variance – particularly of the postulated target, the spike protein – is much less. This allowed the first vaccine candidate to be developed within weeks of its genetic sequence being made public.
Q. The Covid-19 vaccine is today’s version of the Holy Grail. Will it finally silence the virulent vaccine sceptics or at least neutralise Vaccine Hesitancy, listed among WHO’s ‘10 greatest dangers of 2019’?
I very much doubt it. There have been antivaxxers as long as there have been vaccines. If anything they have been more vocal during this crisis. Today misinformation and false rumours can spread faster than a virus, thanks largely to social media platforms. There are also many people who may support vaccination, but nevertheless have questions and concerns about the speed at which COVID-19 vaccines are being developed. We can make the problem part of the solution: use the same social media to provide factual information about vaccine safety from trusted sources. Sadly, the poorest suffer the most because they are disproportionately hit by vaccine-preventable diseases. So every gain made by antivaxxers is a blow against efforts to end poverty. Ultimately, with COVID-19, when we do get safe and effective vaccines, it will be a tragedy if fear-mongering has left people too afraid to receive them. And given the global impact of COVID-19, the longer it takes to protect everyone, the longer this pandemic will rage.