How do vaccine challenge trials ensure the benefits outweigh the risks?
The UK is expected to host the world’s first COVID-19 human “challenge” trials, which will involve deliberately infecting healthy volunteers with coronavirus to assess the effectiveness of experimental vaccines. So far, around 2,000 potential volunteers have signed up. But do how do we ensure the benefits outweigh the risks?
- 30 September 2020
- 5 min read
- by Priya Joi
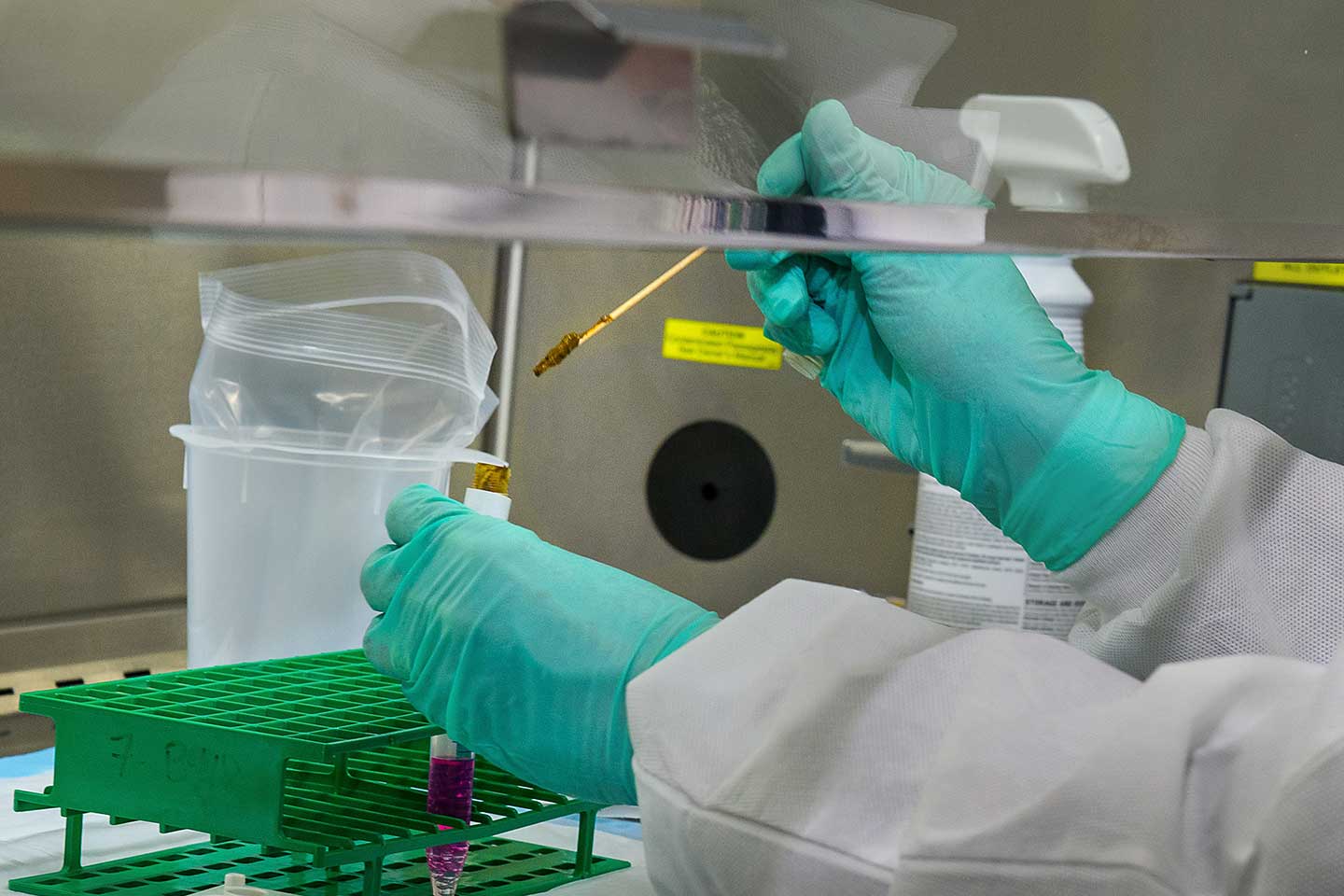
British researchers plan to start inoculating healthy volunteers with experimental COVID-19 vaccine and then exposing them to a challenge dose of coronavirus under controlled conditions. In so doing, they hope to gain earlier insights into vaccine efficacy - and any safety issues - than could be achieved with larger field trials.
Full details of the UK challenge trial are yet to emerge, but this won’t be the first time that volunteers have been deliberately infected with pathogens to test potential vaccines or treatments. Challenge studies have previously been carried out with other types of coronavirus, such as those that cause the common cold, as well as H1N1 influenza virus. They have also hastened the development of vaccines against typhoid and cholera, as well as improving our understanding of how immunity to influenza, malaria, typhoid, dengue fever and cholera develops.
They have also hastened the development of vaccines against typhoid and cholera, as well as improving our understanding of how immunity to influenza, malaria, typhoid, dengue fever and cholera develops.
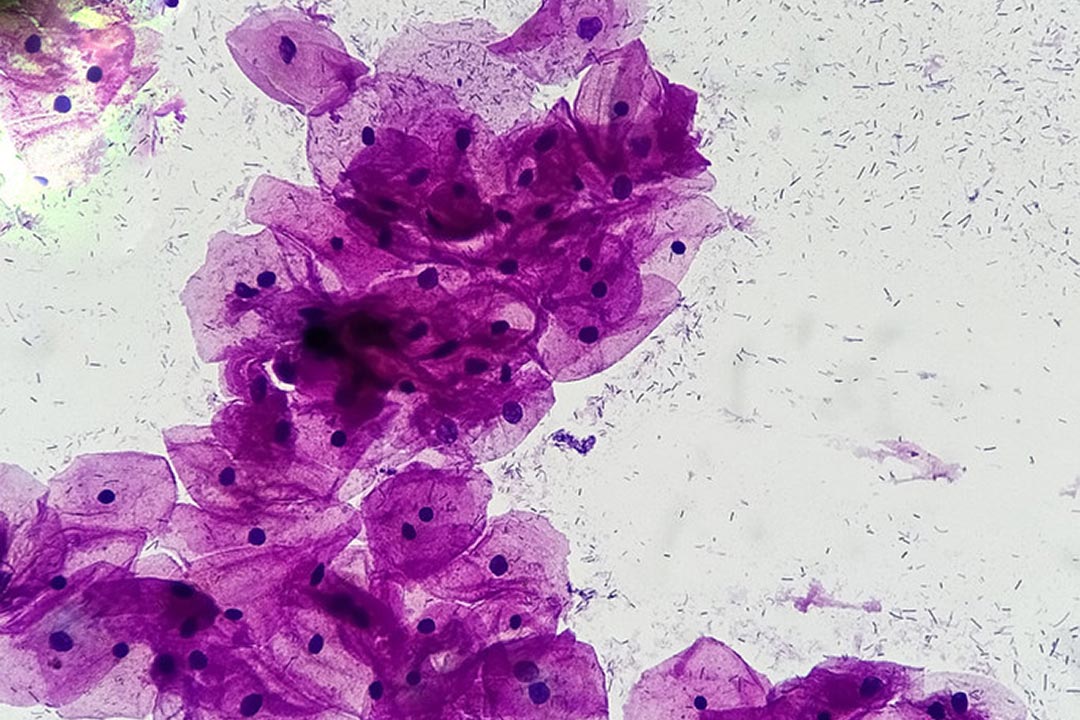
In the case of COVID-19, researchers have suggested that challenge studies could provide faster results than lengthy phase 3 studies. These usually involve monitoring several thousand people for long enough to assess whether the vaccinated group is less likely to develop disease than control groups when both are potentially exposed to the infection during their normal activities. In contrast, human challenge studies involve deliberately exposing healthy vaccinated individuals to COVID-19 in a highly controlled fashion.
If successful, such a study could speed up the time it takes to show that the vaccine candidate reduced the incidence of disease. It could then be combined with a separate placebo-controlled study involving at least 3,000 participants in the vaccinated group - with a focus on assessing short-term safety in a specific group, such as older people or those with pre-existing illnesses that put them at high risk of COVID-related complications. Together the two studies might provide enough evidence to justify accelerated vaccine licensing for both healthy individuals and specific high-risk groups.
Exposing people to infectious agents, such as the SARS-CoV-2 virus which causes COVID-19, obviously carries risks. However, a well-designed challenge study has the potential to subtract months off the vaccine development process. Challenge studies can also be used to directly compare the efficacy of several vaccines, meaning only the most promising are selected for larger studies, and make it more likely that the vaccines ultimately deployed are the most effective.
Besides studying the efficacy of vaccines, challenge studies could also be used to answer important questions, such as how long someone with antibodies to SARS-CoV-2 remains immune, whether immunity to SARS-CoV-2 protects against infection or just against severe disease, and the risk of infection posed by people who carry the virus without displaying symptoms.
Risk-benefit analysis
There are also ways of reducing the risks to study participants. One is to develop ‘challenge strains’ of the pathogen, which are less likely to cause severe disease. The US National Institutes of Health is reported to have awarded US$ 3.6 million to Colorado State University to support the manufacture of SARS-CoV-2 strains which could be used in such challenge studies – although it is unclear if similar strains will be used in the British trials. Doing so takes time, however, and diverging too far from the pandemic strain risks producing misleading results.
Have you read?
Another strategy is to recruit only young and healthy volunteers. For instance, in the case of COVID-19, just 0.6-1% of 20-29-year-olds require admission to hospital because of their infection. For a challenge study, the risk is likely to be lower still, because anyone with pre-existing medical conditions would be barred from participating. Volunteers would also benefit from close monitoring and immediate access to medical care in the event of any difficulties.
There may be other benefits for participants, such as early access to an effective vaccine, or immunity generated through exposure to the live virus – although for COVID-19, it is still unclear how long such immunity lasts or whether it protects against infection as well as severe disease.
On the other hand, because there is still a lot we don’t know about SARS-CoV-2 and there are so few effective treatments for it, the risks of challenge studies are arguably higher than for other diseases for which treatment options are more available. Even challenge studies with more established pathogens, such as malaria and influenza, have led to some unexpected rare but severe outcomes in healthy volunteers.
Ethical guidance
For this reason, it is essential that SARS-CoV-2 challenge studies are conducted to the highest scientific and ethical standards. The British challenge study still needs to be approved by the UK’s Medicines and Healthcare products Regulatory Agency (MHRA) as well as an independent research ethics committee. The World Health Organization (WHO) has also drawn up eight ethical criteria for conducting SARS-CoV-2 challenge studies. These include the need for a strong scientific justification for conducting the study, and an expectation that the potential benefits will outweigh the risks. Particularly important results would include those that would be expected to lead to large public health benefits being achieved sooner than would otherwise be possible, such as informing the selection of the safest and most effective vaccines from among multiple candidates, according to WHO.
Studies should also be informed by consultation and engagement with the public, relevant experts and policy-makers - and involve rigorous informed consent.
We'd love to hear your feedback!
Learn more about Gavi
Gavi’s mission is to save lives and protect people’s health by increasing equitable and sustainable use of vaccines.
Learn about our different types of support, understand how our support works from application to renewal, and find out how we work towards making immunisation programmes sustainable
Since its creation in 2000, Gavi has helped vaccinate over 1 billion children in the world’s poorest countries, preventing more than 17.3 million future deaths. Learn about how we've performed against our strategic goals, the independent…