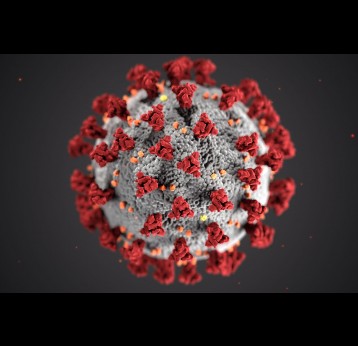
What does COVID-19 mean for this year’s flu season?
Every winter, hundreds of thousands become infected with seasonal influenza, which kills between 290,000 and 650,000 people worldwide each year. But this year, we have another respiratory illness to contend with: COVID-19. So, what does this mean for this year’s flu season?
- 29 September 2020
- 5 min read
- by Priya Joi
-
Republish this article
Disclaimer
If you would like to republish this article, please follow these steps: use the HTML below; do not edit the text; include the author’s byline; credit VaccinesWork as the original source; and include the page view counter script.

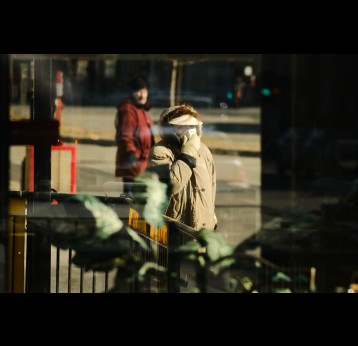
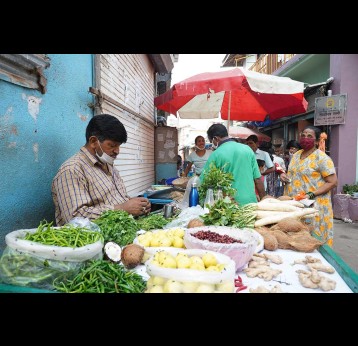
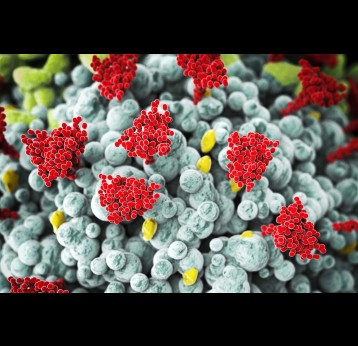
The flu virus spreads when people breathe in respiratory particles from the sneezes and coughs of someone who is infected, or when they touch surfaces which are contaminated with the virus. The best advice to avoid the flu is to not be in crowded areas with poor ventilation, not go to work places or schools where others are infected, and to wash your hands regularly. This year, the southern hemisphere’s flu season coincided with the start of the COVID-19 pandemic, which had a dramatic impact on cases of influenza. The measures introduced to prevent the spread of COVID-19, with human contact reduced to almost zero, increasing wearing of surgical and cloth masks and the increase in regular hand washing, meant there were virtually no flu cases.
Lockdown wiped out the flu season in the South
Seasonal flu kills about 0.1% of people it infects, but since it spreads easily, it is estimated to kill on average 389,000 a year (about 2% of all annual respiratory deaths). Of these deaths, 67% were among people aged 65 years or older.
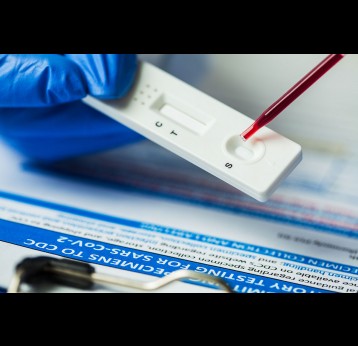
South Africa sees around 11,000 flu deaths every year. To keep track of cases, its National Institute for Communicable Diseases (NICD) undertakes rigorous flu surveillance, involving random laboratory screening. Usually, this would identify about 1,000 cases of flu, but by the end of March, the institute recorded only a single case.
A similar pattern has been observed elsewhere. For instance, a study of flu activity during COVID-19 showed that between April and July 2020, only 33 cases were found among 60,031 specimens tested in Australia, 12 in 21,178 specimens in Chile, and six in 2,098 in South Africa – a total of 51 influenza positive specimens out of 83,307 tested (0.06%). By contrast, during the same months in 2017–2019, 24,512 specimens tested positive for influenza among 178,690 across these three countries. That’s 13.7% - so significantly higher than this year.
The best advice to avoid the flu is to not be in crowded areas with poor ventilation, not go to work places or schools where others are infected, and to wash your hands regularly.
How bad will the northern hemisphere’s flu season be?
The COVID-19 lockdown also had a positive effect on the northern hemisphere’s flu season, which was tailing off at the start of the pandemic. In the United States, there was a 98% decrease in flu sample specimens testing positive, from 19.34% in September to February, down to just 0.33% between March and May.
In many countries with unusually low numbers of flu cases, reduced testing may initially have contributed, But when public health officials and clinicians made renewed efforts to identify adequate numbers of samples to test, they still found little trace of the influenza virus.
So, what does this mean for the northern hemisphere over the coming months?
The main difference now, say scientists, is that whereas countries were shutting down at the start of the southern flu season, they are now opening up – including re-opening schools, which is a major contributor to the spread of flu. It’s true that life has not totally gone back to the ease of movement of pre-pandemic days. In Spain, for example, measures taken to reduce the spread of COVID-19 in schools, such as smaller class sizes, frequent hand-washing and requiring children over the age of six years to wear masks all day, could also slow the spread of flu.
But countries are implementing more varied and complex restrictions around COVID-19 than they did back at the start of the pandemic, meaning many people have far more social contact now than they did during lockdown. Even with continued guidance to maintain social distancing, wear masks and wash hands, pandemic fatigue could mean that people are tiring of these measures, or taking them less seriously than when COVID-19 first emerged.
Why the flu vaccine is more important than ever
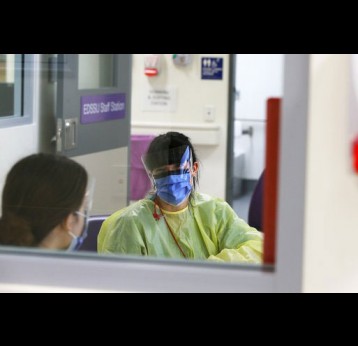
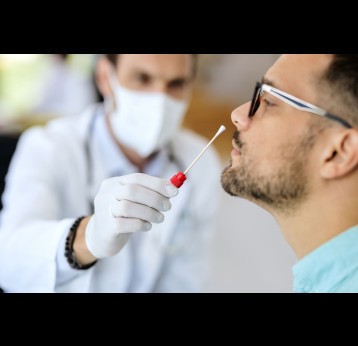
The prospect of the northern hemisphere flu season swamping countries with influenza cases as well as COVID-19 is grim; co-infection with both respiratory viruses could be deadly. Many countries are already seeing a second wave of the coronavirus cases and the additional burden of caring for people with flu could be disastrous. Plus, people with flu symptoms will need testing to rule out COVID-19, and testing systems are already under strain almost everywhere.
Also, there could be an unexpected downside to fewer cases of flu: every year, researchers study circulating influenza viruses to guide the composition of the flu vaccine for the following year. Less circulating flu virus means it is harder to know which genetic variants have been most common, and are therefore most likely to be the dominating ones the following year. By the end of this month, flu experts will need to settle on the make-up of next year’s flu vaccine for the southern hemisphere.
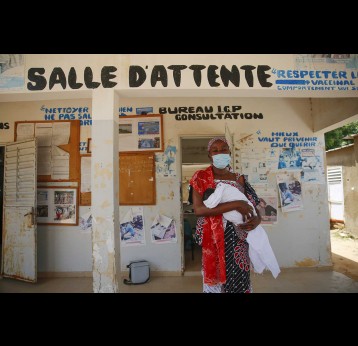
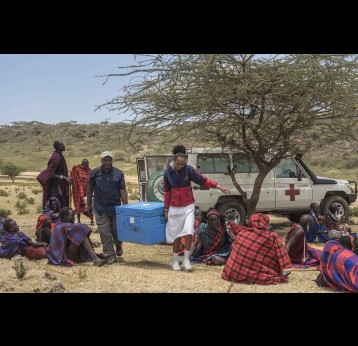
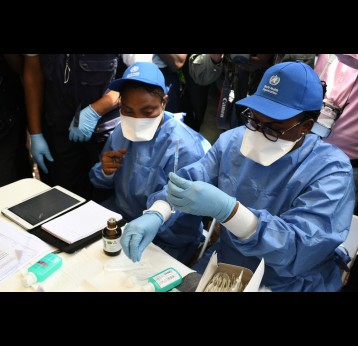
During these uncertain times, flu vaccinations will be more important than ever - especially for older people or those with underlying conditions. Because of this, flu vaccine manufacturers such GlaxoSmithKline and AstraZeneca are ramping up production for the 2020-21 season in northern countries. The US CDC is expected to produce up to 198 million doses - an increase of 20 million compared to last year. Similarly the UK is expanding the age groups eligible for a free flu shot among both children and adults.
We'd love to hear your feedback!
Related content
How long after I get COVID-19 will I test negative?
Testing positive for COVID-19 – even without symptoms – can be disruptive to daily life, but how long should we expect to test positive for?
First published on 29 October 2021, updated on 13 September 2022
Nine factors that could boost your risk of Long COVID
Emerging research is shedding light on why some people are more likely to develop persistent symptoms after catching COVID-19 than others.
Fit for women: 5 things you need to know about global health, gender equality and PPE
Women make up 70% of the health workforce, yet personal protective equipment – or PPE – is still not being designed for them. A landmark conference held this week looked at solutions to the insidious gender bias putting female health workers’…
“Stealth Omicron”: Everything you need to know about the new BA.2 subvariant of SARS-CoV-2
A descendent of the Omicron variant called BA.2 could be more contagious, but it doesn’t appear to cause more severe COVID-19 disease.
Can Omicron evade detection from PCR, rapid antigen or lateral flow tests?
PCR and antigen tests are still reliable in detecting the new variant, although in the first few days saliva could be better than nose swabs at picking up the virus.
Is the Western diet causing a spike in autoimmune diseases?
Autoimmune diseases are becoming more prevalent around the world. They come about when the body’s immune system has difficulty distinguishing healthy cells from unhealthy microorganisms. These diseases include type 1 diabetes, rheumatoid…
Seven reasons why trying to get ‘COVID over with’ is a bad idea
With more than half of all Europeans predicted to be infected with COVID-19 in the next two months, and perceptions of it being mild, it might be tempting to think it’s better to get the infection over with. Here’s why that is a dangerous game to…
The top 5 Omicron symptoms to be aware of
As the Omicron variant of COVID-19 continues to spread around the world, here’s what you need to know about its symptoms.
Infectious period: Are cuts to COVID-19 isolation times a good idea?
Growing numbers of countries are cutting the isolation period for people who test positive for COVID-19, but what does the science say about how long people remain infectious for?
Prioritise first doses of COVID-19 vaccines over boosters, say WHO experts
3.6 million people have still not had even their first dose of COVID-19 vaccine. Ensuring every adult has received at least one dose should be our focus for 2022.
India versus Omicron: How the country’s third COVID-19 wave might unfold
Daily COVID-19 cases have been rising fast, so how well protected is India’s population against Omicron?
Common cold could explain why some people never seem to get COVID-19
A recent cold is no substitute for a COVID-19 vaccine, but lingering immunity from one might protect a lucky few.
How COVID-19 vaccines affect the menstrual cycle
Emerging evidence suggests that COVID-19 vaccination does impact menstrual cycle length – but the effect is minor and temporary.
Could the Omicron variant end the pandemic?
Omicron’s seemingly milder symptoms have prompted some to speculate that the COVID-19 pandemic is burning out. But low vaccination rates mean there could be plenty of obstacles ahead.
Everything you need to know about “Flurona”
Influenza-coronavirus co-infections are increasingly being reported in the media, but how common are they, and should we be worried?
Is Omicron really less severe than previous COVID-19 variants?
Mounting evidence suggests the Omicron variant is associated with fewer hospitalisations and is less likely to infect the lungs. However, it remains a major threat.
How Omicron could make other variants less dangerous
Research from South Africa has found another way in which Omicron could replace Delta and potentially make it less dangerous by boosting immunity to the latter variant.
How can scientists update coronavirus vaccines for omicron?
A microbiologist answers 5 questions about how Moderna and Pfizer could rapidly adjust mRNA vaccines.
How the public came together to support COVID-19 vaccines for the world’s most vulnerable
People around the world have demonstrated global solidarity by donating to the COVAX Facility, providing vaccines to those who would otherwise have no access.
Not so super-immunity: People who’ve recovered from COVID-19 and vaccinated can still be reinfected
Israeli data suggests even those who’ve been double-jabbed or recovered from COVID-19 should take precautions to avoid infection.
COVID passes: they can’t prevent every infection but do make events safer
COVID passes lower the risk of transmission and incentivise vaccine uptake at a time when boosters are desperately needed.
While immunologists often focus on antibody responses to SARS-CoV-2, T cell immunity may hold the key to preventing severe COVID-19 disease.
How do the symptoms of Omicron differ from previous COVID-19 variants?
Reports that the Omicron variant may be associated with milder symptoms increase the need for vigilance and infection control.
How to talk to your children about getting their vaccine - an expert explains
Children might be unsettled by needles and vaccinations. However, vaccinations are an essential tool to stemming the spread of COVID-19. Here an expert explains what you can do to help alieviate children's concerns.
Since being designated a variant of concern on 26 November, the Omicron variant has rapidly spread across the globe. The consequences of this are still unclear, but scientific data is now starting to emerge.
COVID-19 vaccines and pregnancy – here’s what you need to know
Many myths and rumours have spread around the impact COVID-19 vaccinations could have on pregnancy and fertility. The truth is far more reassuring.
How a mix-and-match vaccine approach could boost immunity to COVID-19
Signs are emerging that the way your immune cells encounter SARS-CoV-2 can have a lasting impact on how they respond to it in the future.
How COVID-19 led to devastating rises in malaria
The fight against the killer disease has nearly halved malaria deaths since 2000, but now that hard-won progress could be lost because of the pandemic.
From Alpha to Omicron: Everything you need to know about SARS-CoV-2 variants of concern
All viruses change over time, and SARS-CoV-2 is no exception. Here’s what we know about the current variants circulating globally at the current time.
Omg, Omicron! Why it’s too soon to panic about COVID vaccines and the new variant
We won't know whether Omicron evades COVID vaccines for another few weeks. Here's why.
How next-generation COVID-19 vaccines could help to end the pandemic
A year ago, we had no COVID-19 vaccines, now we have many. Could the next generation of vaccines be better still?
The Future of Global Pandemic Security: Navigating shifting landscapes – a Gavi White Paper
The COVID-19 pandemic has demonstrated how ill-prepared health systems and societies are in the face of pandemic shocks and their protracted impact. Now, as global attention begins to shift towards improving the way we prevent and respond to…
What do we know about the new B.1.1.529 coronavirus variant and should we be worried?
The variant was first detected in Botswana and contains a high number of mutations associated with increased immune evasion.
Immune to COVID-19: Why some people test negative when everyone around them is testing positive
Researchers are closing in on why some people are apparently more resistant to COVID-19 infection.
Q&A: Designing a shock-proof health system
How do we ensure resilient health systems and immunisation programmes that can bounce back from future health threats? In this Q&A with Gustavo Correa, Gavi’s Senior Manager for Data systems and Information, and Josh Wunderlich, Gavi…
Doctors, scientists or politicians: who are you most likely to trust after the pandemic?
Doctors are rated as trustworthy by almost two-thirds of people, according to the Ipsos Global Trustworthiness Index 2021. Scientists came in second, at 61% and teachers third, at 55%. How to restore trust is a key and growing theme for…
The Test of Pandemic Preparedness
The COVID-19 pandemic is the product of a globalized, interconnected world. Without new mechanisms that offer truly global approaches to crisis management and prevention, the experience of the past 18 months is likely to be repeated, with…
What you need to know about COVID-19 vaccines and rare neurological complications
Reports of Guillain–Barré syndrome or other neurological complications following COVID-19 vaccination are understandably worrying, but the first study to robustly investigate such links has found that the risk is much greater after COVID-19…
Five reasons why ‘my body, my choice’ doesn’t work for vaccines
With several countries making COVID-19 vaccinations mandatory for health workers, teachers and other frontline staff, anti-vaccination protesters have co-opted the feminist slogan “my body, my choice” from reproductive rights and bodily autonomy…
Ten climate actions that could boost human health
Ahead of the COP26 climate summit, the World Health Organisation flags ten priority actions necessary to protect human and planetary health.
Pandemica, a world where the pandemic goes on forever
Welcome to Pandemica, a world where twice as many people die and life as we once knew it does not return for anyone.
Why we still need vaccines even if we get new COVID-19 treatments
The pharma company Merck has applied for emergency use authorisation for an experimental COVID-19 antiviral treatment but, even if approved, such therapies won’t replace vaccines.
COVID: why are people testing positive on lateral flow tests then negative on PCR?
The reasons for these results have yet to be confirmed – but maths may explain the phenomenon.
Review: Preventing The Next Pandemic: Vaccine Diplomacy in a Time of Anti-Science
Dr Peter J. Hotez’ timely and important book underlines the fact that we need vaccine diplomacy now more than ever to overcome threats to our health.
Super clean: Hand sanitiser helps prevent COVID-19, but what else is it doing to our health?
Hand sanitiser has become a regular feature of our lives since the start of the COVID-19 pandemic, but how effective is it – and is it a good idea to be so clean?
What we really know about waning COVID-19 immunity
Vaccines are still extremely effective at preventing severe disease. Waning antibody levels doesn’t always translate to lessening immunity.
Seven COVID-19 symptoms you shouldn’t ignore
Researchers have identified seven symptoms that are highly predictive of a positive COVID-19 test.
Kids and COVID-19: what we know so far
Although children are less susceptible to COVID-19 than adults, there are still risks associated with infection.
The pandemic has hurt women's health. This is why that's bad for everyone
The pandemic undermined women and girls’ fundamental rights and we must learn lessons about its impacts to build back better and ensure these groups aren't left behind. Empowering women and girls has proven to increase the health and well-being…
Five reasons why it’s a terrible idea to hold a COVID-19 party (even if you’ve been vaccinated)
Although people who have recovered from COVID-19 may be less likely to catch it again, there are many reasons to avoid becoming infected in the first place.
Study finds no increased risk of COVID-19 vaccination in pregnancy
Israeli data adds to mounting evidence that taking a COVID-19 vaccine during pregnancy is safe.
Three things this week’s Global COVID-19 Summit is aiming to achieve
The White House is calling a virtual COVID-19 Summit on Wednesday, 22 September. Its targets for global vaccination are ambitious and essential as we work together to defeat COVID-19.
We need to stop talking about COVID-19 waves
While vaccines have helped save millions of lives in this pandemic, the ever-evolving virus has spread so far that it may be here to stay.
Why India’s latest Nipah case means pandemic preparedness is more vital than ever
With COVID-19 still ongoing, viruses like Nipah are nipping at its heels as the potential next pandemic threat.
How COVID-19 is undermining maternal health and reproductive rights
As the African continent battles a third wave of coronavirus infections, access to reproductive health and rights is an ongoing challenge.
No scientific basis for COVID-19 vaccine boosters in general populations
Even though many wealthy countries are planning to roll out booster doses, a Lancet review has concluded that the standard COVID-19 vaccination regimen is highly effective, even against the Delta variant.
Study of 6.2 million Americans shows no significant side effects from COVID-19 RNA vaccines
A study looking at health issues such as stroke or seizures after COVID-19 vaccination showed that vaccines weren’t linked to any significant number of side effects.
COVID-19 vaccination halves the risk of Long COVID
Data from the UK suggests double vaccination lowers the risk of ongoing COVID-19 symptoms, as well as reducing hospitalisations and the severity of the initial illness.
COVID-19 vaccines are safe. Here’s why.
While most people jumped at the chance to get their COVID-19 vaccine, some have been more hesitant over concerns about safety. Here we explain all the checks and balances in place to make sure the vaccines are safe.
What does the new C.1.2 coronavirus variant mean for COVID-19 vaccines?
A rapidly mutating coronavirus variant called C.1.2 is generating headlines around the world. Here’s what we know about it so far.
People who have already had COVID-19 could be less likely to catch Delta than the vaccinated
A new study from Israel suggests the risk of a breakthrough infection among vaccinated people was higher than among people who’d previously had COVID-19 but had not been vaccinated. However the greatest benefit came to those who'd previously…
Why kids in low-income countries could face a higher risk of dying of COVID-19
Children are increasingly falling sick worldwide, but existing poor health and inadequate access to health care means the most vulnerable kids are most at risk.
A new study suggests the RTS,S malaria vaccine alone is as effective as preventive antimalarials; together they could save thousands of lives.
How artificial intelligence could help the fight against COVID-19
Using big data and deep learning, machines and systems are offering new ways of responding to a pandemic.
COVID-19 boosters: Would a third jab really stop the pandemic?
Rich countries are now considering giving booster doses to vulnerable individuals, having fully-vaccinated most adults. Is this wise?
Is modern life encouraging the evolution of deadlier viruses?
The way we live can shape the evolution of pathogens, for better or worse.
COVID-19: why we can’t use antibody tests to show that vaccines are working
Many COVID-19 antibody tests are not designed to specifically detect antibodies that develop as a result of vaccination, and thus cannot show whether antibodies are of the right quantity or quality for protection against infection or illness.
Are chatbots better than humans at fighting vaccine hesitancy?
Could artificial intelligence succeed where people have failed in helping people overcome their fears about vaccines?
Why are fully-vaccinated people still catching COVID-19?
Breakthrough infections are to be expected, but it doesn’t mean the COVID-19 vaccines aren’t working.
How will COVID vaccines work on compromised immune systems? Here’s what we know
Being immunocompromised appears to affect the vaccine response, but this seems to vary depending on the causes of the person's low immunity.
Fighting liver cancer with vaccines in The Gambia
Vaccines against cancer may seem like a futuristic notion, but children around the world are already getting protection against two of the biggest causes of cervical and liver cancer: HPV and hepatitis B.
The COVAX No Fault Compensation Programme: Explained
Indemnity and liability was one of the thorniest problems COVAX had to solve to successfully roll out COVID-19 vaccines in lower-income countries. The solution is a world first, which could offer a model for future pandemics.
Will COVID-19 evolve to be more or less deadly?
Some viruses gradually become less virulent over time, but there's no guarantee that SARS-CoV-2 will follow that pattern.
Could a universal coronavirus vaccine soon be a reality?
COVID-19 is unlikely to be the last coronavirus we ever see. Scientists are already trying to make a one-size-fits-all vaccine to stop a future coronavirus epidemic in its tracks.
Are new variants making the COVID-19 virus as deadly as SARS?
Although related to the virus that caused the SARS pandemic in 2003, the COVID-19 virus has never seemed as deadly – until now.
Five ways to mitigate India’s third COVID-19 wave
India’s second wave of COVID-19 has devastated the country through a perfect storm of new variants, low vaccination uptake and a shortage of medical equipment and supplies. Here’s what we need to understand about the ongoing second wave to…
India’s “Covaxin” vaccine shows high efficacy against COVID-19 infections in phase 3 trial
A vaccine that had previously been authorised by the Indian government ahead of phase 3 trials now show promising results. This could add to the global armoury of vaccines against COVID-19.
False negative: How long does it take for coronavirus to become detectable by PCR?
It takes time for coronavirus to become established in the body, so a negative test doesn’t necessarily mean you won’t test positive later on.
There’s now a Delta Plus variant of COVID-19 – what does this mean?
The Delta variant that has caused devastation in countries like India and the UK has now mutated to produce another variant called Delta Plus. Should we be worried?
By identifying people with high levels of neutralising antibodies after a first vaccine dose, rapid tests could potentially identify those who don’t need a booster dose.
How the pandemic is fuelling antimicrobial resistance
For years, a growing number of infections that are resistant to antimicrobials has offered us a grim glimpse into a future with increasingly untreatable diseases. Now, COVID-19 has made antimicrobial resistance so much worse.
Could lifting COVID-19 restrictions trigger a surge in other common infections?
Masks, hand washing and physical distancing don’t only reduce the transmission of coronavirus. So, what will happen when we do away with these measures?
What happens when COVID-19 collides with HIV infection?
Mounting evidence suggests people living with HIV may be at greater risk of dying from COVID-19. The good news is that COVID-19 vaccines appear to be safe and effective in people with HIV.
How vaccines turbo-charge any existing immunity against COVID-19
A previous infection does give you some immunity against COVID-19, but a new study suggests that vaccination gives your body a massive boost – including against variants of concern.
Five Good Reasons to Go Give One
Wondering what you can do to help end the acute phase of the pandemic? Go Give One – is giving everyone everywhere a chance to play their part.
Why we support COVAX: Mastercard
Mastercard, a long-standing partner of Gavi, recently committed US$ 28 million to the Gavi COVAX AMC, to ensure vaccines are accessible to those that needed them the most, no matter where they live. Vaccines Work spoke to Michael Froman to learn…
Seven ways in which COVID-19 could change the way we fight infectious diseases
The pandemic turned our normal ways of working upside down, but there are several ways in which the new normal could bring improvements in the way we fight disease.
Lifesaving but unaffordable: pros and cons of the newest COVID-19 treatment
Antibody therapy reduces COVID-19 fatalities by a fifth, but remains inaccessible to many countries.
Why we still need R&D into COVID-19 vaccines
There are now 17 COVID-19 vaccines approved for emergency use, but as the virus continues to evolve, here is why we can’t pull the plug on research into new vaccines and therapeutics.
How COVID-19 will damage the lives of African children for decades to come
Although the coronavirus doesn’t cause disease and death in children as much as it does in adults, many children around the world are vulnerable to the collateral damage wreaked by the pandemic.
Five things we know about the Delta variant (and two things we don't)
The Delta (B.1.617.2) variant of SARS CoV-2 was first detected in India and is rapidly spreading around the world. Here’s what we know about it so far.
Why speaking without a mask is the easiest way to spread COVID-19
COVID-19 virus particles can be spread via coughing, sneezing, breathing or speech, but the latter is one of the most effective ways of spreading. Here is why talking without a mask indoors could be one of the easiest ways to spread the infection…
How well do first and second vaccine doses work against Covid-19?
Is it risky or wise to delay the second dose of Covid-19 vaccine? Critics warned against the UK government policy of leaving a longer gap between doses of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines. Now we have more data, so what do we…
Do COVID-19 vaccines affect menstruation and fertility?
Ever since the pandemic started there have been news headlines speculating about the effect of the vaccines on our reproductive system, but what does the science tell us?
Six ways to know the COVID-19 pandemic is over
It’s been over a year now since the pandemic first started, and now that vaccines are rolling out in many countries, how long do we have to wait for things to go back to ‘normal’?
While we don't know exactly what causes it yet, there are a few theories put forward by a few researchers around the world.
Can dogs be trained to sniff out COVID-19?
Various countries are training dogs to detect coronavirus, and the results of early clinical trials are looking promising.
Why COVID-19 variants got new Greek names
Calling variants by their country of origin has politicised the pandemic response, leading to countries being blamed and people originating from those countries stigmatised and targeted – sometimes violently. Now, the World Health Organization is…
How the predicted hunger pandemic became a grim reality
Worldwide more than 3.5 million people have died of COVID-19 so far; now millions more are on the brink of starvation because of a connected hunger crisis.
Can you test positive for COVID-19 test after getting the vaccine?
As more people get vaccinated, and testing requirements are becoming commonplace to allow freedom to travel and work, we look at the circumstances under which you could test positive for COVID-19 even after being vaccinated.
COVID-19 in the house: How to reduce the risk of transmission
Further infections are not inevitable, if you take the following steps.
If you’ve had COVID-19 you could be more than 80% protected from reinfection
Whether or not you can become reinfected with COVID-19 hasn’t been clear so far, but a new study from Denmark indicates that immune response triggered by the first infection offers good protection.
Self-COVID-19 tests: do you know your tonsils from your uvula?
Some COVID-19 tests require you to swab your own tonsils, but could you be mistaking them for something else?
How the answer to long-lived immunity to COVID-19 could lie in our bone marrow
People who have had COVID-19 seem to have bone marrow cells that could produce antibodies for years to come, which could mean that immunity both from natural infection and vaccination is long lasting.
Is it safe to mix and match COVID-19 vaccines?
Mixing COVID-19 is being proposed in some countries but is it safe to do so, and how do our immune systems react?
The point of it: Why do vaccine delivery methods vary?
Some vaccines are injected into muscle; others are given orally, or under the skin. What difference does it make to our immune response?
How to give a COVID-mitigated hug
No activity that brings you into someone else’s breathing space is safe, but the risks associated with hugging can be lowered by taking some simple precautions.
Can we stop wearing masks after being vaccinated?
In some countries, wearing masks against COVID-19 is not mandatory anymore, but can the rest of the world follow suit?
Asia and Africa offer lessons in health systems resilience
In this pandemic, the income level of a country proved not to be a guarantee of an effective COVID-19 response; this analysis shows the key factors in a resilient health system to protect against future outbreaks.
Do children need to be vaccinated against COVID-19?
Children have so far been able to evade the worst effects of COVID-19, but this could be changing as new variants and other factors seem to be putting more at risk.
Fighting the flu: 100 years of preparing for pandemics
Although the world’s eyes are currently focused on COVID-19, a network of laboratories has been tracking the emergence and spread of a different virus for seven decades.
Why we support COVAX: UBS and UBS Optimus Foundation
The UBS Optimus Foundation has launched a campaign to help secure funding for the COVAX Advance Market Commitment. Vaccines Work spoke to Tom Hall, the UBS Head of Philanthropy Services to find out why.
China’s Sinopharm COVID-19 vaccine first to carry a smart label to monitor heat-damage
It is the first vaccine developed by a non-Western country to be approved by the WHO, and is welcome at a time of global vaccine shortages.
When refusing a COVID-19 vaccine isn’t about hesitancy
The reasons why people may not take a COVID-19 vaccine even when offered can be complex and varied, but they point to the need to tackle them better if we are to improve vaccine coverage.
What are the most effective ways to improve vaccination rates?
Vaccines are one of our greatest success stories, but vaccination rates for many diseases have been stalling; this has been exacerbated with the disruption caused by Covid-19. Anna Mouser sets out the evidence on what works, and what doesn’t, for…
Are COVID-19 vaccine expiration dates too cautious?
Distributing COVID-19 vaccines has been challenging, meaning in some cases vaccines are being delivered close to their expiration date; but the WHO is urging countries to hold on to the doses while it assesses whether shelf lives can be extended…
There are a broad range of different types of vaccine, but one thing they usually have in common is that they are inherently biological. That means that often their ingredients need to be grown.
Vaccines save millions of lives a year, but what exactly is a vaccine and what goes into making one? And how do we know they are safe? Here, we talk about every aspect of vaccines and why they are so important for our health.
Exercise boosts immunity and makes vaccines more effective – new study
Meeting the recommended guidelines for physical activity reduces the risk of falling ill and dying of infectious diseases by 37%.
The Zero-Dose Child: Explained
Despite decades of progress increasing access to immunisation in lower-income countries, at least 12.4 million children still go without basic, routine vaccines every year. Gavi, the Vaccine Alliance is now focusing on reaching these zero-dose…
What ingredients go into a vaccine?
Vaccines contain active ingredients that trigger an immune response to viruses, bacteria and other pathogens. But in order to work well, it is important that they also contain other key ingredients to keep them safe and effective.
How long does immunity last after COVID-19 vaccination?
Millions of doses of COVID-19 vaccines are being delivered across the world, but what do we know about how long will immunity last?
Why we need to share vaccine doses now and why COVAX is the right way to do it
Covid-19 vaccination efforts are picking up worldwide, bringing hopes of returning to a more normal life. Vaccines are now starting to reach countries across the globe through the COVAX initiative, set up to promote equitable access to vaccines…
5 things to know after you’ve had a COVID-19 vaccine
As more and more people get vaccinated against COVID-19, some are worrying about how ‘normal’ their side effects are. Here’s what you need to know.
Africa’s had a 30% rise in COVID-19 cases in the second wave
The continent had a milder first wave than the rest of the world, but research suggests that relaxed public health measures led to the coronavirus rebounding with a vengeance the second time around.
Why is a global Covid-19 vaccine rollout vital?
The Covid-19 pandemic is global, and to bring the pandemic to a close, a collaborative, global approach is needed. But why is it so important that all countries have access to vaccines as soon as possible?
COVID-19 vaccines: could a squirt up the nose be just as good as a shot in the arm?
There are several COVID-19 vaccines being used around the world, but all need to be injected and some need ultra-cold refrigeration. Could next-generation intranasal vaccines be a quicker and easier way of protecting ourselves?
How far away are we from a new TB vaccine?
Tuberculosis kills millions of people each year, but several recent advances in vaccine development are providing fresh hope.
Why COVID-19 makes you lose your sense of smell and how to get it back
The virus appears to attack support cells at the back of the nose, but “smell training” may help people to recover their missing sense.
Does the AstraZeneca COVID-19 vaccine really cause blood clots?
Various countries have halted the use of the Oxford-AstraZeneca vaccine, while reports of blood clots are investigated. Here’s what we know so far.
Why do some people with COVID-19 get sicker than others?
Our immune systems are supposed to defend us from invading pathogens but, in the case of COVID-19, an immune overreaction may be to blame for severe illness.
Why I volunteered to be infected with coronavirus
Most people have been doing everything they can to avoid getting COVID-19, but in the coming days British history student Jacob Hopkins has chosen to be deliberately infected with SARS-CoV-2 as part of the world’s first Challenge Trial. He…
5 reasons to believe the COVID-19 pandemic might be slowing down
COVID-19 cases are falling week on week, so can we allow ourselves to be hopeful?
Could a universal coronavirus vaccine future-proof our response?
With three major coronavirus outbreaks in the last two decades – first SARS-CoV, then MERS-CoV, and now SARS-CoV-2 that causes COVID-19 – another outbreak is inevitable. Scientists are calling for the world to step up the search for a universal…
What are COVID-19 challenge trials and why do we need them?
A new trial about to start in the UK will deliberately infect people with the virus that causes COVID-19 – if we have vaccines already, why do we need this?
The largest global rollout of vaccines in history just got one step closer
The World Health Organization has given the Oxford-AstraZeneca vaccine an Emergency Use Listing, passing an important milestone before the first delivery of COVAX vaccines worldwide.
Do COVID-19 variants mean that we need a booster shot for our booster?
Oxford scientists are already working on an updated version of their COVID-19 vaccine to ensure people remain fully protected against new variants of SARS-CoV-2. But how would these be delivered and how often would they be needed?
WHO experts have just recommended the Oxford-AstraZeneca vaccine: here’s what they found
The recommendations offer reassurance amid concern over whether some vaccines are as effective against new variants.
What are 'adverse events' and 'emergency use authorisation' in relation to vaccination?
While vaccines are the safest way to prevent the spread of infectious disease, a tiny proportion of those vaccinated may experience an adverse event. Here, we explain how often this happens and why.
Here’s how we could stop antimicrobial resistance becoming the next pandemic
Antimicrobial resistance was already a major global health threat, but now the potential increase in the use of antibiotics in response to the pandemic could exacerbate the problem and threaten a potentially even bigger global crisis.
How COVID-19 is altering cold and flu seasons
Pandemic restrictions and wider use of flu vaccines may have explained 2020’s record low cases of seasonal flu, but will the picture look like in tropical countries with year-round flu?
Why even a low efficacy COVID-19 vaccine could still be extremely useful
Efficacy rates for COVID-19 vaccines are higher than many scientists had dared dream of, but even if they prove less effective in real life, or in the face of new variants, they could still unlock normal life.
Who can’t have a COVID-19 vaccine?
The currently available coronavirus vaccines have been tested on adults of various ages, as well as those with long-term conditions, and appear to be safe. But there are a few groups who should avoid being vaccinated for now.
How safe are COVID-19 vaccines?
Given the speed at which COVID-19 vaccines have been developed, it is understandable that people want to know whether they are safe. So what measures have been put in place to ensure the safety of these new vaccines?
How India is using a digital track and trace system to ensure COVID-19 vaccines reach everyone
A system originally designed to do real-time monitoring of vaccine supply chains in India has now been adapted to help ensure COVID-19 vaccines reach as many people as possible.
When Your Chance for a Covid Shot Comes, Don’t Worry About the Numbers
When getting vaccinated against covid-19, there’s no sense being picky. You should take the first authorized vaccine that’s offered, experts say.
COVID-19 impact ‘vastly underestimated’ in African countries
Zambian data challenges the assumption African populations may have been spared from COVID-19.
How accurate are lateral flow tests?
Will these rapid tests really allow us to lower our guard during the pandemic?
Lasting immunity: Why COVID-19 vaccines may succeed where natural infections fail
Immunity to most coronaviruses is short-lived, but will the same hold true for the virus that causes COVID-19 or vaccines against it?
5 Reasons to Wear a Mask Even After You’re Vaccinated
Vaccination, face coverings and physical distancing are essential parts of a team effort against the coronavirus.
Will the new variant of COVID-19 make re-infection more likely?
New variants of the coronavirus are causing alarm across the UK and South Africa, with many countries closing their borders to travellers from these countries. But what effect could new strains have on our ability to control the pandemic?
If I delay getting a COVID-19 vaccine, what impact will it have?
Taking a wait-and-see approach to COVID-19 vaccines could lead to only pockets of the population being protected. Will this be enough to end the pandemic?
How South Africa is preparing for its COVID-19 vaccine introduction
As participating countries look towards receiving their first batch of COVID-19 vaccines through the COVAX Facility, we examine how South Africa is ramping up its readiness.
Could COVID-19 vaccines be tweaked to cover new coronavirus variants?
We’ve always been able to adapt vaccines to protect against emerging variants and additional pathogen strains, but new vaccine platforms could make this even easier.
Why lockdown can be bad for your immune system - and what to do about it
Lockdowns are an effective way of reducing COVID-19 infections, but they could take a more general toll on our health if we allow them to.
COVID-19 vaccines are set to become the quickest vaccines in history to go from initial trials to rollout, but what lessons can we learn from its speedy predecessor: the Ebola vaccine?
What do the new COVID-19 variants mean for vaccine development?
Viruses are constantly mutating and often this process does not have any impact on the risk they pose to humans. However, occasionally mutations can occur which make it easier for viruses to infect us, or which could render vaccines against them…
What you need to know about a COVID-19 vaccine
Answers to the most common questions about coronavirus vaccine development.
What are whole virus vaccines and how could they be used against COVID-19?
Whole virus vaccines use a weakened or deactivated version of the disease-causing virus to trigger protective immunity against it.
Seven vital questions about RNA Covid-19 vaccines
The Pfizer-BioNTech and Moderna Covid-19 vaccines are more than 90% effective, as reported in phase III clinical trials – and the Pfizer-BioNTech vaccine is the first Covid-19 vaccine to be licensed.
What are viral vector-based vaccines and how could they be used against COVID-19?
Viral vector-based vaccines use a harmless virus to smuggle the instructions for making antigens from the disease-causing virus into cells, triggering protective immunity against it.
What are protein subunit vaccines and how could they be used against COVID-19?
Protein subunit vaccines use fragments of protein from the disease-causing virus to trigger protective immunity against it.
What are nucleic acid vaccines and how could they be used against COVID-19?
Nucleic acid vaccines use genetic material from a disease-causing virus to trigger protective immunity against it.
What you need to know about COVID-19 vaccine approvals in Nigeria and South Africa
Before any COVID-19 vaccines can be delivered to the public, their use must be approved by national regulatory authorities. We look into the process before vaccines would be approved for distribution and use in Nigeria and South Africa.
What to expect when you get a COVID-19 vaccine
Now that the first COVID-19 vaccine has been approved, and others are on the way, what does getting vaccinated actually involve? Here are some of the logistics involved and what to expect after you’ve had your vaccine.
There are four types of COVID-19 vaccines: here’s how they work
The fight against COVID-19 has seen vaccine development move at record speed, with more than 170 different vaccines in trials. But how are they different from each other and how will they protect us against the disease?
Two billion doses of COVID-19 vaccines have been secured to ensure that no-one misses out
The COVAX Facility plans to start rolling out the doses in early 2021 to high-risk groups in participating countries, with the aim of vaccinating up to 20% of populations of participating countries by the end of the year.
There’s a new strain of COVID-19 – should we worry?
Viruses mutate all the time, but this new mutation affects the viral protein that invades human cells. What does this mean for the pandemic and the vaccine?
How did scientists manage to develop safe COVID-19 vaccines in just ten months?
The COVID-19 vaccines currently rolling off production lines have been developed faster than any other vaccine against a new disease in history. How have scientists achieved this incredible feat? And could the lessons learned enable more rapid…
Can I catch COVID-19 from Christmas wrapping paper?
Coronavirus can survive on surfaces, so should unwrapping presents be considered risky? We examine the evidence.
How to stay safe from COVID-19 this festive period
COVID-19-related restrictions differ from country to country, but as families gather to celebrate during the festive holidays there are some important things you can do to protect yourselves and your loved ones against coronavirus.
What do immunity passports and vaccination certificates mean for COVID-19 restrictions?
Here’s why continuing to physically distance and wear masks is vital until we can be sure how long vaccine-acquired immunity lasts.
How small clinical trial sample sizes can offer important findings
Scientists have been racing to develop COVID-19 vaccines that could reach millions, yet many of the studies have surprisingly small sample sizes drawn from the clinical trials. Does that matter?
COVID-19 could undermine progress towards reducing infant mortality
Over the past three decades, improvements to maternal and newborn health have led to many more infants surviving beyond the first 28 days of life. But disruptions to health services caused by the COVID-19 pandemic may now be undoing years of hard…
Anxiety, depression and insomnia: the impact of COVID-19 on mental health
COVID-19 patients are at an increased risk of being diagnosed with anxiety, depression or insomnia. Here’s a closer look at how the SARS-CoV-2 virus can impact your mental health.
COVID-19 ‘Vaccine for the World’ shows up to 90% efficacy
Interim analysis of the AstraZeneca/Oxford COVID-19 vaccine candidate – to which Gavi has secured access – suggests an efficacy of 62– 90%. Crucially, the vaccine can be administered and distributed using existing health care and supply chain…
What is lateral flow testing and how could it be deployed against coronavirus?
Unlike PCR tests, which involve complex laboratory equipment and highly trained staff, lateral flow tests can be processed on the spot and return a result far quicker. But how exactly do they work, and could they really make a difference to the…
What is the difference between efficacy and effectiveness?
The two terms used to describe how well a drug or vaccine works are often used interchangeably, but they are not actually the same thing – here’s why.
A smart label on vaccine vials will be vital for safely rolling out future COVID-19 vaccines
Interim results suggesting that Pfizer/BioNTech’s COVID-19 vaccine provides more than a 90% efficacy, offers hope that immunisation can be effective against COVID-19. But the need to store this vaccine at “ultra cold” temperatures could pose…
Six in ten children are immune to the COVID-19 virus despite never being infected by it
Immunity triggered by exposure to the coronaviruses that cause the common cold could protect people, especially children, against the SARS-CoV-2 virus.
Adverse events following immunisation: what are they, and when are they cause for concern?
A successful vaccine produces the best possible immune response, whilst keeping side effects to a minimum. When adverse events following immunisation (AEFIs) do occur, it is important that they are reported, especially if they are serious, even…
Pfizer’s COVID-19 vaccine may be over 90% efficacious, so what happens next?
An interim analysis of the Pfizer/BioNTech vaccine candidate suggests is more efficacious than many had dared to expect. The announcement is a welcome indication that a safe and effective COVID-19 vaccine might be within reach, but there are…
Why we will always need vaccinations
Vaccination programmes have prevented millions of deaths worldwide, but their continued success relies on our continued participation.
Do mutations of COVID-19 virus in mink pose a threat to people?
With Denmark culling its entire farmed mink population following discovery of a mutated form of SARS-CoV2, are we at risk of further complications and diseases from animal-human transmission?
Why understanding superspreaders could be one key way of controlling the COVID-19 pandemic
Superspreading events, where one person infects tens of others, appear to be playing an increasingly significant role in the spread of COVID-19. So what have we learned about these events and how can we stop them from fuelling the pandemic?
How does COVID-19 trigger a loss of smell and other olfactory disorders?
Anosmia is the medical term for a sudden loss of smell and has been associated with COVID-19. Here’s a closer look at the olfactory dysfunctions linked to the SARS-CoV-2 virus.
We need Covid-19 treatments as well as vaccines – and they have to work for everyone
Effective treatments that are accessible to everyone who needs them have to be part of the solution to the coronavirus pandemic – here's why.
What impact does malnutrition have on the effectiveness of vaccination?
Malnutrition can affect the immune system and the quality of immune response to vaccinations, with potential implications for low-income countries where COVID-19 is already fuelling a "hunger pandemic" in the most vulnerable people.
How COVID-19 may have increased dengue infections in Thailand and Singapore
Spending less time in the workplace usually results in lower rates of infectious disease, but workplace closures in Southeast Asia and the Western Pacific may be increasing exposure to the mosquitoes that transmit dengue virus.
How geospatial technology can help to zero in on zero-dose children
Combining geographical information on populations, locations of health care sites, and the movement of vaccinators can offer insights into how efficient and equitable vaccination coverage is, and has great potential to improve immunisation…
Why some people might be immune to certain COVID-19 vaccines
Vaccines based on the common cold virus are at the forefront of the COVID-19 vaccine race, but they may be less effective in people who have previously been infected by these common pathogens. So how could we overcome this challenge?
Why handwashing with soap is the most effective way to stop viruses
Global Handwashing Day and the ongoing spread of COVID-19 is a timely reminder about the importance of handwashing with soap as an effective and affordable way to stay healthy.
Will silent reinfections drive the spread of COVID?
People who have had COVID-19 can develop an immune response that normally protects people from recurrent infection. But now that reinfections of COVID-19 have been recorded, what does that mean for our ability to fight the virus?
What are monoclonal antibodies – and can they treat Covid-19?
For more than 30 years, monoclonal antibodies have transformed the way we treat many diseases. Researchers think they are also one of the most promising treatments for Covid-19. Here's why.
How emergency use authorisations could accelerate access to COVID-19 vaccines
Emergency use procedures are designed to make potentially life-saving medical products available as quickly as possible during health emergencies. A record number have been granted since the arrival of COVID-19 pandemic, but what does this mean…
From equality to global poverty: how Covid-19 is affecting societies and economies
The Covid-19 pandemic is a social and an economic crisis just as much as it is a health crisis – its repercussions, severe and far-reaching, are being felt across the world.
How do vaccine challenge trials ensure the benefits outweigh the risks?
The UK is expected to host the world’s first COVID-19 human “challenge” trials, which will involve deliberately infecting healthy volunteers with coronavirus to assess the effectiveness of experimental vaccines. So far, around 2,000 potential…
What does COVID-19 mean for this year’s flu season?
Every winter, hundreds of thousands become infected with seasonal influenza, which kills between 290,000 and 650,000 people worldwide each year. But this year, we have another respiratory illness to contend with: COVID-19. So, what does this mean…
Which COVID-19 test is most relevant to me?
At the beginning of the pandemic there was a mad scramble to develop a test which would accurately diagnose COVID-19 infection. Now, six months in, hundreds of testsare available – but how do they differ, and which test is the…
How can we make fair and equitable access to COVID-19 vaccines a reality?
How will COVAX ensure that COVID-19 vaccine doses reach all countries at the same time, and protect those people that need it the most?
There’s more than one way for a COVID-19 vaccine to end this pandemic
Effective vaccines prevent individuals from developing disease, but some also stop people transmitting the pathogens that cause them. What role will they have to play in ending the COVID-19 pandemic?
Why is no one safe until everyone is safe during a pandemic?
No one is safe until everyone is safe. This phrase has become a slogan for global health figures but what does it mean in the worldwide COVID-19 response?
Are vaccines a global public good?
As COVID-19 vaccines have a critical role to play in ending this pandemic crisis, many experts have described them as a global public good. But what exactly does that mean?
How vaccination can reduce sepsis and save millions of lives
Many of the infections that can lead to sepsis are becoming resistant to antibiotics, which means that preventing them by vaccination is critical.
Different types of immunity and why they matter to COVID-19
Antibodies are one route to immunity against disease, but T cells and innate immunity also play a crucial role in protecting us. So, how could these different types of immunity be mobilised against COVID-19
To end this global health crisis we don’t just need COVID-19 vaccines, we also need to ensure that everyone in the world has access to them.
Who should we vaccinate first?
When COVID-19 vaccines become available demand is likely to outstrip supply, at least initially. So, who should be first in line?
Is it possible to get COVID-19 more than once?
What do the first confirmed cases of reinfection with COVID-19 mean for the rest of us and future of this pandemic?
Can vaccine clinical trials be sped up safely for COVID-19?
One of the most time-consuming parts of vaccine research and development is the testing of a vaccine. How does this work, and how, in the context of COVID-19, are scientists trying to speed it up?
How do vaccines actually work?
Vaccines prevent millions of deaths every year by harnessing the body’s immune system to create defences against future infection. But how exactly does this work?
Why COVID-19 means Gavi is supporting more countries than ever before
Since 2000, Gavi has been increasing equitable access to vaccines by working with the world’s poorest countries. Yet during a pandemic, more prosperous countries are also at risk of falling through the net. How will Gavi respond?
Gavi has helped lower-income nations narrow the vaccine coverage gap
Lower-income countries are seeing better vaccination coverage than they have had in decades, but the COVID-19 pandemic is threatening to hamper progress.
Can the BCG vaccine protect against COVID-19?
While researchers racing to develop a COVID-19 vaccine, the potential of the BCG vaccine – used to prevent TB – to slow the pandemic has been hotly debated. New research suggesting that the BCG could prevent severe COVID-19 disease has made…
How do we know who is immune to COVID-19?
With surveys using antibody tests yielding disappointing results, there are growing concerns that fewer people may have already been infected with SARS-CoV-2 than was previously hoped. Yet antibodies are only part of our immune system’s response…
Ebola is officially over in North Kivu and Ituri - what can we learn for COVID-19?
On 25 June, the outbreak of Ebola in the Democratic Republic of the Congo that has raged for more than 2 years is over. What does this mean for the country and what can it teach us about ending the COVID-19 pandemic?
Why development aid transparency matters
At a time when economies are under pressure and government spending is under scrutiny, transparency and accountability within the development sector is more important than ever.
Will we see a deadly second wave of COVID-19 later in the year?
Beijing, a city month’s ahead of Europe in COVID-19 terms, is now plunging back into lockdown. Many are concerned that this could be the first hint of a second wave. But is that likely and what would it look like?
The long-term health effects of COVID-19
Even mild symptoms from the new coronavirus can last for weeks, or disappear only to rebound with renewed intensity, so what long-term effects does the disease have on our health?
When it comes to COVID-19 vaccines how can governments back a winner?
With so many COVID-19 candidate vaccines in development, and with most of them likely to fail, what’s the best way for governments to ensure they back a winner and ensure there are enough doses for everyone?
A third of the world has been under some form of lockdown to tackle the COVID-19 pandemic, but has it made any difference to the number of cases and deaths?
How are Gavi's private sector partners stepping up to help fight COVID-19?
Despite the devastating economic impact this pandemic has had on businesses across the world, many are doing their part to bring this crisis to an end.
Gavi provides funding to support the pandemic response in Myanmar
As one of the poorest low-income countries in South East Asia, Myanmar faces many barriers to implementing a strong and effective response to COVID-19. Gavi has now allocated over US$ 8.8 million to help ensure that Myanmar is better able to…
When will it be safe to hug people again?
The physical distancing necessary to slow the spread of COVID-19 can be emotionally distressing, but since the virus is unlikely to disappear soon, when will life regain a semblance of normality?
Why is the Global Vaccine Summit so important?
The pandemic will only strengthen our commitment to vaccinate vulnerable communities. On 4 June 2020 Gavi will hold its third donor pledging conference online with the aim to raise vital funds for the next five years.
How does COVID-19 compare to past pandemics?
The COVID-19 pandemic is most often compared to the H1N1 influenza pandemic of 1918, or Spanish flu, even though there have been three other major pandemics since then. So how does this coronavirus pandemic compare to those?
Why are BAME groups experiencing high rates of death from COVID-19?
Black, Asian and minority ethnic (BAME) communities in Europe and the USA are overrepresented in COVID-19 deaths. In the bid to slow and, ultimately, stop the spread of COVID-19 it is vital to understand the reasons why, in order to adequately…
COVID-19’s collateral damage could devastate low- and middle-income countries
While the number of COVID-19 cases and deaths stays relatively low across Africa, Asia and Latin America compared with the rest of the world, the economic and social consequences are likely to reverberate for decades to come.
Could COVID-19 accelerate the digitisation of vaccine records?
The COVID-19 pandemic is disrupting vaccination programmes across the world, but this could provide an opportunity to hasten the move to digital record-keeping systems.
What is COVID-19’s ‘R number’ and why does it matter?
Altering the ease with which the new coronavirus spreads in the population is critical to controlling the pandemic. The number of people infected by any single case - the R number – will be key. If the virus is able to infect more than one person…
How quickly can we get a COVID-19 vaccine?
It is clear that the search for COVID-19 vaccines is being fast-tracked like never before. In just a few months, we now have over 100 vaccine candidates in development, ten of which are being tested in clinical trials.
What is contact tracing, how could it reduce the spread of COVID-19, and how could it affect me?
Controlling the pandemic demands a multi-pronged approach with other key methods like contact tracing to help stop the chain of transmission.
The future with COVID-19: three potential scenarios
What our lives will look in the short to medium term future is uncertain, but what does seem clear is we won’t return to a pre-COVID-19 life any time soon. Here are three potential scenarios that infectious disease experts have sketched out for…
How COVID-19 could be causing a rare complication in children
Initially, children seemed to be least affected by the new coronavirus. However, new evidence suggests that a small number might have a rare immune reaction to COVID-19, with some needing intensive care.
How equipment is protecting us against COVID-19
Personal protective equipment, or PPE, such as masks and gloves are becoming part of our daily lives, but what counts as effective PPE and what doesn’t?
How can the technology in our pockets track COVID-19?
Tracking who is infected is essential to controlling the transmission of contagious diseases. Could digital technology prove to be a game-changer for the current pandemic?
10 infectious diseases that could be the next pandemic
Because of vaccination, many deadly diseases are now preventable. But we still lack vaccines for other potentially lethal diseases that could spread to become pandemics like COVID-19. Here is a list of 10 diseases to watch.
COVID-19: Diagnostic testing uses, types and challenges
Even when a COVID-19 vaccine is available, testing can help pinpoint populations who should be prioritised for immunisation.
What is an Advance Market Commitment and how could it help beat COVID-19?
How we can ensure that once a COVID-19 vaccine is available, it is accessible to everyone that needs it.
When is it safe to lift COVID-19 lockdown?
With so many lives and livelihoods at stake, when will the lockdowns end, and what will they look like across the world?
Will wearing a mask protect me from COVID-19?
How exactly is the COVID-19 virus spread and will a mask protect me?
Can routine immunisation be carried out safely during COVID-19 pandemic?
How does the benefit of stopping the spread of coronavirus weigh up against the risks from diseases such as measles?
When is COVID-19 most contagious and why is self-isolation so important?
Although there are guidelines on how long people should self-isolate when infected, the data on how long people remain contagious is not yet fully understood.
Why human impact on the environment is leading to infections like COVID-19
As we continue to encroach on the environment and erode natural habitats, the likelihood of other diseases like COVID-19 emerging to devastate the planet are high.
What kind of tests are there for COVID-19?
Large-scale testing for COVID-19 could help solve some of the mysteries surrounding the virus that are still puzzling scientists.
What is COVID-19 and how is it spread?
With nearly 550,000 people infected, almost 25,000 dead, and hundreds of millions in lockdown across the globe, the coronavirus pandemic has brought the world to a standstill. But what do we know about COVID-19 and what can we do to fight this…
The idea of herd immunity as the solution to the COVID-19 pandemic has triggered heated debate, but what is herd immunity and how does it work?
Why is coronavirus lockdown necessary?
With an increasing number of countries around the globe going into lockdown because of the COVID-19 pandemic, many people forced to stay home may be wondering why these measures are necessary, how long they will need to go on for and what it will…
What is Gavi’s role in stopping the COVID-19 pandemic?
On the most recent issue of The Bio Report podcast, Gavi's Aurélia Nguyen discusses COVID-19 vaccine development, the role of the Vaccine Alliance in stopping the pandemic, and shares lessons learned from the 2014 Ebola outbreak that may prove…
Research summary: How do you beat the COVID-19 pandemic in the absence of a drug or vaccine?
If COVID-19 epidemics are not controlled, 510,000 people could die in the UK and 2.2 million in the USA.
What not to touch: how to avoid contact with the new coronavirus
We touch countless objects every day, from house keys to our mobile phones. The virus that causes COVID-19 can last for anywhere from 30 minutes to several hours in the air (in the form of aerosol droplets) before drifting down onto surfaces,…
How clinical vaccine trials are speeding up in a pandemic
Clinical trials for vaccines can take 10-15 years and cost hundreds of millions of dollars, which is why pharmaceutical companies can be reluctant to start down that challenging road without a definite pay-off at the end. As the COVID-19 pandemic…
From travel restrictions to social distancing, what is the best way to stop a pandemic?




























































































































![© UNICEF/UN0200242/Singh [NOTE: This is a file photo] In India, pentavalent vaccines are being checked for imperfections.](/sites/default/files/styles/content_feed_thumbnail/public/vaccineswork/2020/Thumbnail/UN0200242_h2.jpg?itok=hJ_OHDIY)