A new mpox variant has been identified in the UK. Should we be worried?
The new strain combines both currently recognised strains of the virus – clade I and clade II. Scientists are watching closely.
- 9 December 2025
- 5 min read
- by Priya Joi
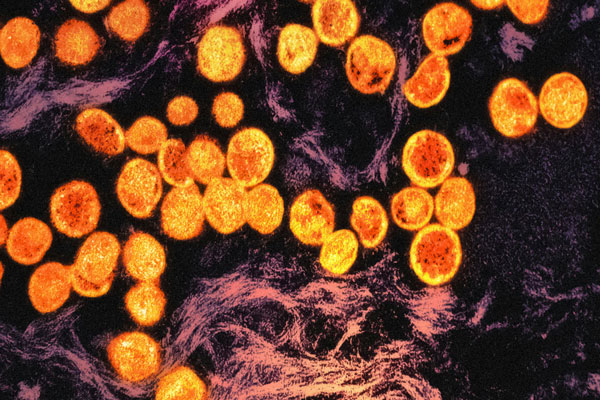
A new hybrid strain of mpox has been reported in the UK, according to the UK Health Security Agency (UKHSA).
The new strain, found in an individual who had recently travelled to Asia, is a mix of clade I and clade II strains of mpox – both of which can spread through close contact with infected people.
Mpox has been a growing concern since the first global outbreak of the virus in 2022, however African epidemiologists have said the worldwide spread might have been curbed if their warnings of the virus resurging in Africa had not been ignored.
Dr Boghuma Titanji, Assistant Professor of Medicine at Emory University, said the discovery of a recombinant strain was “precisely what experts in the field feared would happen if the virus continued to spread globally without a decisive response to stop it."
Dr Katy Sinka, Head of Sexually Transmitted Infections at UKHSA, is urging people to get vaccinated against mpox if they are eligible because “getting vaccinated is a proven effective way to protect yourself against severe disease."
Evolving outbreak
When mpox emerged as a global health concern in 2022, it was through the spread of the clade II strain – which tends to be less deadly than clade I and can spread through sexual contact, which clade I wasn’t known to do at the time.
However, in late 2024, it was the growing circulation of the deadlier clade I that was causing concern, especially as it seemed to have acquired the ability to spread via sexual transmission.
Both clades cause similar symptoms, such as fever, muscle aches and headaches, as well as a distinctive rash with blisters or ulcers. Clade I has been more deadly though, killing up to 10% of people it infects.
The rapid spread of clade I from the Democratic Republic of the Congo (DRC) to several neighbouring countries prompted the World Health Organization (WHO) to declare mpox a public health emergency of international concern in August 2024.
In September 2025, WHO declared that mpox was no longer a global emergency, however late last week WHO published a new alert on broader transmission of clade I mpox virus in several non-endemic countries, including the United States.
Rare recombination
“Orthopoxviruses [like mpox] are well known for their ability to exchange portions of their genome and recombine to generate new variants. This is a core mechanism of their evolution,” said Dr Titanji.
Have you read?
Nevertheless, Professor Geoffrey Smith, University of Oxford, described this recombination of both clades as a “rare event”.
For a hybrid virus to be created, he said, the same cell has to be infected with both strains at the same time because it is inside the infected cell that recombination takes place.
“It is made rarer still,” he added, “by the mechanisms orthopoxviruses deploy to prevent a second infection of a cell that is already infected by another orthopoxvirus. Therefore, to infect a cell with both viruses, the infection with each virus has to be at a very similar time, meaning within just a few hours.”
“The key concern now is whether events like this will alter the virus’s transmissibility or virulence,” said Dr Titanji.
What is the current status of the mpox outbreak?
In its latest situation report on mpox, the WHO said 44 countries recorded a total of 2,501 new cases in October – with around 75% of them in 21 countries in Africa.
However, it also notes that countries reporting the highest number of confirmed cases over the last six weeks – DRC, Liberia, Ghana, Kenya and Uganda – are all showing a downward trend in cases in recent weeks.
In some African countries, vaccination may be helping to drive down mpox rates.
In November 2024, Gavi and partners launched an mpox vaccination campaign to deliver vaccines to countries hit hard by the virus.
Gavi is also funding an mpox vaccine stockpile to ensure a rapid response to viral outbreaks, and this will become operational in 2026.
In Sierra Leone, for example, mpox cases have been falling steadily over the past year as the country strengthened its surveillance systems alongside promoting vaccination through community engagement. Sierra Leone is now aiming to get to zero cases.
There are hopeful signs that the outbreak is waning in neighbouring DRC too, in large part to the engaged community who were actively interested in being vaccinated.
Gavi is also funding an mpox vaccine stockpile to ensure a rapid response to viral outbreaks, and this will become operational in 2026.
The dangers of unrestrained spread
Professor Trudie Lang, Director of the Global Health Network, University of Oxford, warned that monitoring the evolution of the virus will be critical but challenging in places with stretched resources.
“In the UK, we have excellent systems to identify cases, control onward infection and implement vaccination campaigns as needed, and these measures should rapidly control this situation.”
However, she said, “Elsewhere in the world, in more vulnerable populations and where case detection and access to vaccinations is not so assured, this is harder to achieve.”
Dr Titanji said: “There are also implications for how well existing testing platforms can identify these emerging recombinant strains. The more mpox circulation we permit, the more opportunities the virus has to recombine and adapt, further entrenching mpox virus as a human pathogen that is not going away.”









