Six reasons why community health workers are the unsung heroes of global immunisation
These frontline workers are critical in getting vaccines to those who need them most, yet are rarely prioritised in health systems planning.
- 28 October 2025
- 5 min read
- by Priya Joi

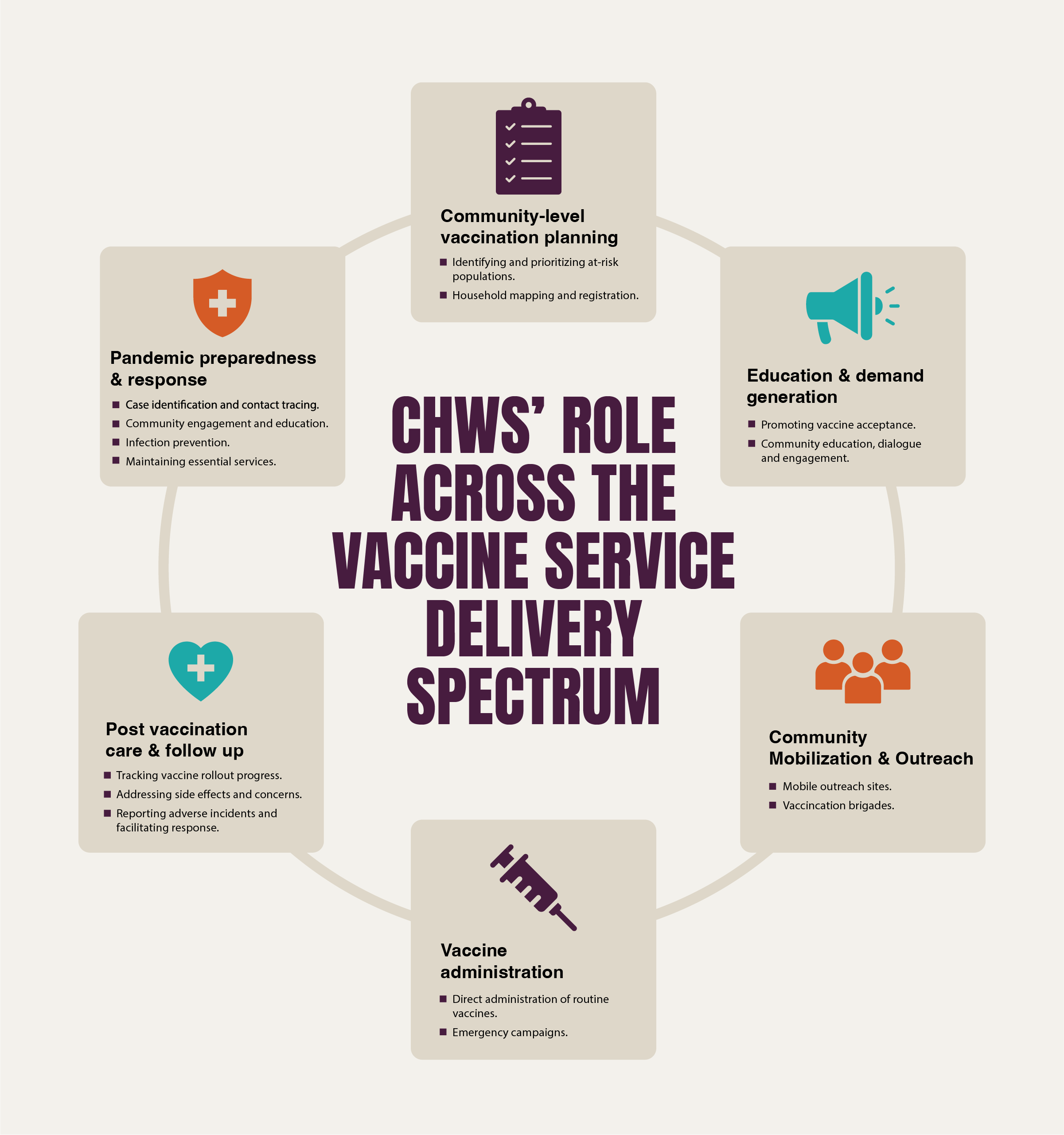
Across the world, community health workers (CHWs) are playing a frontline role in reaching people often left out of mainstream healthcare.
In the wake of the pandemic and rising health disparities, they played a pivotal role in a wide range of tasks related to core health service provision, such as community mobilisation, health promotion and provision of preventive services.
They can be critical in increasing vaccine coverage and turning the tide in neighbourhoods where hesitancy and misinformation once held sway.
As trusted local figures, these health workers don’t just provide information about vaccines; they can be a crucial liaison between families and health systems, a connection that might be broken without them.
Community health workers are the backbone of global vaccination efforts, boosting access, equity, resilience and cost-effectiveness. Yet to fully realise their potential, policies must support their training, salaries, safety and integration into formal health systems.
An impact and cost-effectiveness brief by the Community Health Impact Coalition on the role of community health workers (CHWs) shows how they remain critical in improving immunisation coverage.
1. Community health workers close crucial gaps in immunisation
Community health workers, often deeply rooted in their communities, bridge the gap between families and the formal health system. By delivering vaccine information, combatting misinformation, and providing post-vaccination support, they nurture trust and encourage immunisation.
Around 70% of community health workers are women, reflecting their unique position in community networks. Their empathy and cultural fluency help address vaccine hesitancy more effectively than traditional channels.
This community connection also enables these health workers to tailor health messages that resonate with local beliefs and concerns, which is crucial for overcoming scepticism and misinformation.
2. Community health workers connect with the hard-to-reach
In regions where health services are scarce, ommunity health workers serve as primary sources of vaccine information and care. Outreach campaigns led by these health workers have repeatedly succeeded in linking hard-to-reach families to vaccination services, notably improving equity in coverage.
Their presence in remote or marginalised communities means they often act as the only reliable health contact available, ensuring that even the most isolated families receive life-saving vaccines.
For example, in parts of sub-Saharan Africa and South Asia, community health workers have been instrumental in identifying children missed by routine immunisation programmes and facilitating their inclusion, significantly reducing the number of zero-dose children.
3. Community health workers can help drive demand and boost resilience
Community health workers help build stronger, more resilient communities by ensuring continuity of care – even as budgets tighten and outbreaks surge.
Their role extends beyond vaccine delivery; they organise community mobilisation, educate caregivers, and maintain essential health services during crises. This adaptability was evident during the COVID-19 pandemic, where these health workers were frontline responders not only supporting vaccination efforts but also delivering broader health education and support.
Have you read?
Studies show that in places like Kenya and Uganda, community health worker-led mobilisation has led to marked increases in vaccination uptake and recall for missed doses, reinforcing routine immunisation while strengthening health system resilience.
4. Training community health workers to administer vaccines is cost-effective
In addition to their usual roles in community mobilisation, health promotion and provision of preventive services, the brief encourages countries to consider training CHWs to administer both injectable and oral vaccines.
Training community health workers to administer vaccines has proven highly efficient and safe across diverse settings. Provided that they are well trained, community health workers could ultimately provide direct administration of vaccines in routine immunisation schedules or during emergency campaigns.
The brief gathered evidence to show that in Kenya, community health workers-led interventions made infants 2.5 times more likely to be fully vaccinated.
Meanwhile, in Uganda, upskilled community health workers helped return 68% of children who had missed vaccines, boosting BCG coverage by 35%.
Burkina Faso’s success with health worker training in vaccine administration led to thousands of children immunised during campaigns and the approach was scaled across the Sahel region.
These examples demonstrate that expanding community health workers’ responsibilities, including direct vaccine administration, could not only accelerate coverage but also reduce pressure on health facilities.
5. Community health workers reduce costs and increase impact
Community health workers programmes consistently demonstrate robust cost-effectiveness across health interventions.
Immunisation programmes incorporating community health workers from 2011 to 2030 are projected to prevent illness-related costs totalling over US$ 1.5 trillion in low- and middle-income countries.
The community-based approach minimises costs related to transport and overhead while fostering demand and acceptance of vaccines, resulting in a high return on investment.
Programmes in India’s Accredited Social Health Activist (ASHA) network and Brazil’s Family Health Strategy highlight how effectively trained and supported community health workers can sustain high immunisation rates at relatively low cost.
6. Community health workers are essential for vaccine equity and preparedness
Nearly 80% of populations in 24 Sub-Saharan African countries depend on community health workers for primary health care, including immunisation. Their versatile skill set and local engagement are vital for pandemic preparedness, routine vaccine delivery, and addressing inequities in health.
With growing challenges from emerging infectious diseases and shrinking global health budgets, leveraging community health workers to integrate immunisation with primary health care services will be key to safeguarding communities and ensuring no children are left behind.
To accelerate progress on immunisation, the coalition is urging Gavi, the Vaccine Alliance, the World Health Organization, UNICEF and other partners to fully embed community health workers into their vaccination strategies and funding. Their call includes supporting countries to ensure community health workers are salaried, well-trained, and properly equipped, and strengthening primary care by integrating immunisation campaigns with broader health services.
They emphasise the need for creating practical support tools, promoting community health worker upskilling for expanded vaccine tasks, building stronger data systems, and working with governments and partners to establish clear practice standards and gather evidence on impact.
Community health workers are the backbone of global vaccination efforts, boosting access, equity, resilience and cost-effectiveness. Yet to fully realise their potential, policies must support their training, salaries, safety and integration into formal health systems.
Recognising and investing in community health workers is central to achieving universal immunisation and safeguarding public health worldwide.









